Abstract
Purpose
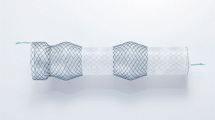
Presentation of results of non-stenting treatment versus endoscopic stenting placement in gastric staple leaks after laparoscopic sleeve gastrectomy (LSG).
Methods
Between January 2007 and August 2020, 1371 eligible patients underwent LSG. After gastric leak detection, patients were classified into treatment groups A (endoscopic stent placement) and B (non-stenting management). Overall hospital stay, the time to complete gastric leak resolution and the incidence of further operative management constituted the main outcome measures. Statistical analysis included descriptive statistics and linear regression tests as needed.
Results
A total of 27 patients (19 F/8 M, median age: 44.8 years (range: 36–58) with median preoperative BMI: 43.5 kg/m2 (range: 37.0–48.7)) presented with gastric staple line leak (1.9%) — mean detection day 5.8 postop (range: 1–12). Eight patients enrolled in group A and 19 patients in group B. The mean hospital stay for group A was 41.2 days (range: 24–60) versus 15 days (range: 12–18) for group B (p < 0.001). Complete leakage resolution was observed at mean 42.4 days (range 25–60) for group A and 34.5 days (range: 28–40) for group B patients, (p = 0.025). Only 2 group A patients accomplished complete leak resolution without additional intervention. Five group A patients (62.5%) versus 4 group B patients (21.1%) needed operative intervention during the treatment course (p = 0.037).
Conclusions
Conservative, non-stenting treatment of staple line leaks after LSG is feasible and is associated with superior results in terms of hospital say and leak resolution in comparison to endoscopic stenting.



Similar content being viewed by others
Availability of data and material
Authors, Andreas Kiriakopoulos MD, Nefeli Kounatidis MS, Menenakos Ilias, Kostrova Maria MD, Zografos Konstantinos MD, Evangelos Menenakos MD, declare that the data of the study are available upon reasonable request.
Code availability
Authors, Andreas Kiriakopoulos MD, Nefeli Kounatidis MS, Menenakos Ilias, Kostrova Maria MD, Zografos Konstantinos MD, Evangelos Menenakos MD, declare that all software applications are available upon reasonable request.
References
Angrisani L, Santonicola A, Iovino P et al (2018) IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg 28:3783–3794. https://doi.org/10.1007/s11695-018-3450-2
Salman MA, El-Ghobary M, Soliman A et al (2020) Long-term changes in leptin, chemerin, and ghrelin levels following Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. Obes Surg 30(3):1052–1060. https://doi.org/10.1007/s11695-019-04254-z
Kalinowski P, Paluszkiewicz R, Wróblewski T, Remiszewski P, Grodzicki M, Bartoszewicz Z, Krawczyk M (2017) Ghrelin, leptin, and glycemic control after sleeve gastrectomy versus Roux-en-Y gastric bypass-results of a randomized clinical trial. Surg Obes Relat Dis 13(2):181–188. https://doi.org/10.1016/j.soard.2016.08.025201618
Gagner M, Hutchinson C, Rosenthal R (2016) Fifth International Consensus Conference: current status of sleeve gastrectomy. Surg Obes Relat Dis 12(4):750–756. https://doi.org/10.1016/j.soard.2016.01.022
McTigue KM, Wellman R, Nauman E, Anau J, Coley RY, Odor A et al (2020) Comparing the 5-year diabetes outcomes of sleeve gastrectomy and gastric bypass: the National Patient-Centered Clinical Research Network (PCORNet) Bariatric Study. JAMA Surg 155(5):e200087. https://doi.org/10.1001/jamasurg.2020.0087
Kichler K, Rosenthal RJ, DeMaria E, Higa K (2019) Reoperative surgery for non-responders and complicated sleeve gastrectomy operations in patients with severe obesity. An international expert panel consensus statement to define best practice guidelines. Surg Obes Relat Dis 15(2):173–186. https://doi.org/10.1016/j.soard.2018.11.006
Gagner M, Buchwald JN (2014) Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Relat Dis 10(4):713–723. https://doi.org/10.1016/j.soard.2014.01.016
Chen B, Kiriakopoulos A, Tsakayannis D, Wachtel MS, Linos D, Frezza EE (2009) Reinforcement does not necessarily reduce the rate of staple line leaks after sleeve gastrectomy. A review of the literature and clinical experiences. Obes Surg 19(2):166–172. https://doi.org/10.1007/s11695-008-9668-7
Nedelcu M, Skalli M, Delhom E, Fabre J, Nocca D (2013) New CT scan classification of leak after sleeve gastrectomy. Obes Surg 23(8):1341–1343
Csendes A, Burdiles P, Burgos AM, Maluenda F, Diaz JC (2005) Conservative management of anastomotic leaks after 557 open gastric bypasses. Obes Surg 15:1252–1256
Burgos AM, Braghetto I, Csendes A, Maluenda F, Korn O, Yarmuch J et al (2009) Gastric leak after laparoscopic-sleeve gastrectomy for obesity. Obes Surg 19:1672–7
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801–810. https://doi.org/10.1001/jama.2016.0287
Bhattacharjee P, Edelson DP, Churpek MM (2017) Identifying patients with sepsis on the hospital wards. Chest 151(4):898–907. https://doi.org/10.1016/j.chest.2016.06.020
Abou Rached A, Basile M, El Masri H (2014) Gastric leaks post sleeve gastrectomy: review of its prevention and management. World J Gastroenterol 20(38):13904–13910. https://doi.org/10.3748/wjg.v20.i38.13904
Berger ER, Clements RH, Morton JM, Huffman KM, Wolfe BM, Nguyen NT et al (2016) The impact of different surgical techniques on outcomes in laparoscopic sleeve gastrectomies: the first report from the metabolic and bariatric surgery accreditation and quality improvement program (MBSAQIP). Ann Surg 264:464–73
Stroh C, Köckerling F, Volker L, Frank B, Stefanie W, Christian K et al (2016) Results of more than 11,800 sleeve gastrectomies: data analysis of the German Bariatric Surgery Registry. Ann Surg 263:949–955
Yolsuriyanwong K, Ingviya T, Kongkamol C, Marcotte E, Chand B (2019) Effects of intraoperative leak testing on postoperative leak-related outcomes after primary bariatric surgery: an analysis of the MBSAQIP database. Surg Obes Relat Dis 15(9):1530–1540. https://doi.org/10.1016/j.soard.2019.06.008
Mumtaz H, BaroneGW KBL et al (2002) Successful management of a non-malignant esophageal perforation with a coated stent. Ann Thorac Surg 74:1233–1235
Salinas A, Baptista A, Santiago E et al (2006) Self-expandable metal stents to treat gastric leaks. Surg Obes Relat Dis 2:570–572
Iannelli A, Schneck AS, Ragot E, Liagre A, Anduze Y, Msika S et al (2009) Laparoscopic sleeve gastrectomy as revisional procedure for failed gastric banding and vertical banded gastroplasty. Obes Surg 19:1216–1220
Shehab H (2018) Enteral stents in the management of post-bariatric surgery leaks. Surg Obes Relat Dis 14(3):393–403
Swinnen J, Eisendrath P, Rigaux J, Kahegeshe L, Lemmers A, Le Moine O, Devière J (2011) Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest Endosc 73(5):890–899. https://doi.org/10.1016/j.gie.2010.12.019
Schiesser M, Kressig P, Bueter M, Nocito A, Bauerfeind P, Gubler C (2014) Successful endoscopic management of gastrointestinal leakages after laparoscopic Roux-en-Y gastric bypass surgery. Dig Surg 31(1):67–70. https://doi.org/10.1159/000358849
Morell B, Murray F, Vetter D et al (2019) Endoscopic vacuum therapy (EVT) for early infradiaphragmal leakage after bariatric surgery—outcomes of six consecutive cases in a single institution. Langenbecks Arch Surg 404:115–121. https://doi.org/10.1007/s00423-019-01750-9
Acknowledgements
We, authors: Andreas Kiriakopoulos MD, Nefeli Kounatidis MS, Menenakos Ilias, Kostrova Maria MD, Zografos Konstantinos MD, Evangelos Menenakos MD, declare that no other personal assistance has taken place in creating this work.
Author information
Authors and Affiliations
Contributions
Andreas Kiriakopoulos: study conception and design, analysis and interpretation of data, drafting of manuscript, critical revision of manuscript. Nefeli Kounatidis: acquisition of data, drafting of manuscript. Menenakos Ilias: study conception and design, acquisition of data, analysis and interpretation of data. Kostrova Maria: study conception and design, acquisition of data, drafting of manuscript. Zografos Konstantinos: acquisition of data, drafting of manuscript, critical revision of manuscript. Menenakos Evangelos: study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript, critical revision of manuscript.
Corresponding author
Ethics declarations
Consent to participate
Authors, Andreas Kiriakopoulos MD, Nefeli Kounatidis MS, Menenakos Ilias, Kostrova Maria MD, Zografos Konstantinos MD, Evangelos Menenakos MD, declare that all participants have consent to this research study.
Consent to publication
Authors, Andreas Kiriakopoulos MD, Nefeli Kounatidis MS, Menenakos Ilias, Kostrova Maria MD, Zografos Konstantinos MD, Evangelos Menenakos MD, declare that we consent to the publication of our research study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kiriakopoulos, A., Kounatidis, N., Menenakos, I. et al. Non-stenting treatment versus endoscopic stent placement in staple line leaks after laparoscopic sleeve gastrectomy. Langenbecks Arch Surg 407, 1863–1872 (2022). https://doi.org/10.1007/s00423-022-02498-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02498-5