Abstract
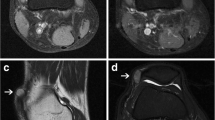
Intra-articular loose bodies (ILBs) are not uncommon conditions in patients with various joint diseases. Their morphological alterations have been investigated in detail, but little attention has been paid to their fatty lesions. In this study, we examined fatty bone marrow, fat cells without bone marrow structures (extramedullary fat cells), and their necrotic changes in 55 ILBs surgically removed from 42 patients, excluding primary synovial chondromatosis cases. The presence of viable re-vascularized vessels with or without enchondral ossification could discriminate 19 re-attached ILBs from 36 true free ILBs. Fatty bone marrow was found in 25 ILBs, and its necrosis was recognized in 11 (44.0%) of them. Extramedullary fat cells, characterized by single or clustered fat cells focally or multifocally distributed in fibrous or cartilaginous stroma, were identified in seven true free ILBs (7of 55, 12.7%), and all of them were focally necrotic. Unique lipomembranous changes were detected in 7 (12.7%) of 55 ILBs; they were found in 4 (36.4%) of 11 ILBs of necrotic bone marrow and were associated with 3 (42.9%) of 7 necrotic extramedullary fatty lesions. These changes were highlighted by periodic-acid Schiff and Masson's trichrome stain more clearly. We concluded that extramedullary fat cells represent lipometaplasia in ILBs with no blood supply. We considered that lipomembranous changes in ILBs can be a useful hallmark for necrotic bone marrow or necrosis of extramedullary lipometaplastic lesions.



Similar content being viewed by others
References
Aurich M, Anders J, Trommer T et al (2006) Histological and cell biological characterization of dissected cartilage fragments in human osteochondritis dissecans of the femoral condyle. Arch Orthop Trauma Surg 126:606–614
Ishida T, Imamura T (2003) Surgical pathology of non-neoplastic bone and joint diseases. Bunkoudo, Tokyo, In Japanese
Milgram JW (1977) The classification of loose bodies in human joints. Clin Orthop Relat Res 124:282–291
Milgram JW (1990) Radiologic and histologic pathology of nontumorous diseases of bones and joints. Northbook Publishing Company, Northbook
O'Connell JX (2000) Pathology of the synovium. Am J Clin Pathol 114:773–784
Phemister DB (1924) The causes of and changes in loose bodies arising from the articular surface of the joint. J Bone Joint Surg 6:278–315
Villacin AB, Brigham LN, Bullough PG (1979) Primary and secondary synovial chondrometaplasia: histopathologic and clinicoradiologic differences. Hum Pathol 10:439–451
Barrie HJ (1978) Intra-articular loose bodies regarded as organ cultures in vivo. J Pathol 125:163–169
Barrie HJ (1980) Hypertrophy and laminar calcification of cartilage in loose bodies as probable evidence of an ossification abnormality. J Pathol 132:161–168
Milgram JW (1977) The development of loose bodies in human joints. Clin Orthop Relat Res 124:292–303
Milgram JW, Gilden JJ, Gilula LA (1996) Multiple loose bodies: formation, revascularization, and resorption. A 29-year followup study. Clin Orthop Relat Res 322:152–157
Saotome K, Tamai K, Koguchi Y, Sakai H, Yamaguchi T (1999) Growth potential of loose bodies: an immunohistochemical examination of primary and secondary synovial osteochondromatosis. J Orthop Res 17:73–79
Saotome K, Tamai K, Osada D, Oshima F, Koguchi Y, Hoshikawa A (2006) Histologic classification of loose bodies in osteoarthrosis. J Orthop Sci 11:607–613
McNutt NS, Moreno A, Contreras F (2005) Inflammatory diseases of the subcutaneous fat. In: Elder DE, Elenitsas R, Johnson BL Jr, Murphy GF (eds) Lever's histopathology of the skin, 9th edn. Lippincott Williams & Wilkins, Philadelphia, pp 519–549
Poppiti RJ Jr, Margulies M, Cabello B, Rywlin AM (1986) Membranous fat necrosis. Am J Surg Pathol 10:62–69
Strangeways TSP (1920) Observations on the nutrition of articular cartilage. Brit Med J 1:661–663
Davis RI, Hamilton A, Biggart JD (1998) Primary synovial chondromatosis: a clinicopathologic review and assessment of malignant potential. Hum Pathol 29:683–688
Brooks JSJ, Perosio PM (1997) Adipose tissue. In: Sternberg SS (ed) Histology for pathologist, 2nd edn. Lippincott-Raven, Philadelphia, pp 167–196
Farrington-Rock C, Crofts NJ, Doherty MJ, Ashton BA, Griffin-Jones C, Canfield AE (2003) Chondrogenic and adipogenic potential of microvascular pericytes. Circulation 110:2226–2232
Alsalameh S, Amin R, Gemba T, Lotz M (2004) Identification of mesenchymal progenitor cells in normal and osteoarthritic human articular cartilage. Arthritis Rheum 50:1522–1532
de la Fuente R, Abad JL, García-Castro J et al (2004) Dedifferentiated adult articular chondrocytes: a population of human multipotent primitive cells. Exp Cell Res 297:313–328
Machinami R (1983) Membranous lipodystrophy-like changes in ischemic necrosis of the legs. Virchows Arch [Pathol Anat] 399:191–205
Machinami R (1984) Incidence of membranous lipodystrophylike change among patients with limb necrosis caused by chronic arterial obstruction. Arch Pathol Lab Med 108:823–826
Nasu T, Tsukahara Y, Terayama K (1973) A lipid metabolic disease–“membranous lipodystrophy”–an autopsy case demonstrating numerous peculiar membrane-structures composed of compound lipid in bone and bone marrow and various adipose tissues. Acta Pathol Jpn 23:539–558
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matsukuma, S., Takeo, H., Okada, K. et al. Fatty lesions in intra-articular loose bodies: a histopathological study of non-primary synovial chondromatosis cases. Virchows Arch 460, 103–108 (2012). https://doi.org/10.1007/s00428-011-1172-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-011-1172-0