Abstract
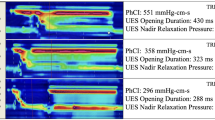
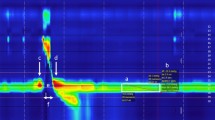
Determining intrabolus pressure (IBP) at the upper esophageal sphincter (UES) and in the esophagus has given compelling evidence that IBP can be a predictor for swallowing dysfunction. Studies have looked most superiorly at the low hypopharynx region but there has been no inquiry into what IBP measures throughout the entire pharynx can tell us. We present a study to describe the pressures within and surrounding the moving bolus throughout the pharynx and into the UES. Simultaneous high-resolution manometry (HRM) and videofluoroscopy were performed in ten healthy subjects swallowing ten 10 mL thin-liquid barium boluses. Three events surrounding bolus movement were tracked via videofluoroscopy, and two additional events were found using manometric measures. As the bolus passes through the pharynx, low pressure is created at and below the head of the bolus. A modest pressure increase is seen as the bolus passes through the pharynx, and finally, high pressure is observed at the bolus tail, followed by an even larger pressure generation of a clearance event. HRM allows for greater resolution in data collection in the pharynx and in this study, aided in identifying semi-unique characteristics around the hypopharynx and the UES which are consistent with the complex anatomy of the regions and the transition of the UES from active closure to relaxed opening. In the future, additional studies designed to look at aged and diseased populations may lead to better understanding of disease etiology, and treatment options.






Similar content being viewed by others
References
Massey BT. Physiology of oral cavity, pharynx and upper esophageal sphincter. GI Motility online 2006.
McConnel FM. Analysis of pressure generation and bolus transit during pharyngeal swallowing. Laryngoscope. 1988;98:71–8.
Mcconnel FMHD, Jackson K, O’Connorn A. Analysis of intrabolus forces in patients with zenker’s diverticulum. Laryngoscope. 1994;104:571–81.
Ali GN, Wallace KL, Laundl TM, Hunt DR, deCarle DJ, Cook IJ. Predictors of outcome following cricopharyngeal disruption for pharyngeal dysphagia. Dysphagia. 1997;12:133–9.
Colizzo JM, Clayton SB, Richter JE. Intrabolus pressure on high-resolution manometry distinguishes fibrostenotic and inflammatory phenotypes of eosinophilic esophagitis. Dis Esophagus, 2015.
Pal A, Williams RB, Cook IJ, Brasseur JG. Intrabolus pressure gradient identifies pathological constriction in the upper esophageal sphincter during flow. Am J Physiol. 2003;285:G1037–48.
Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJ. Normal values for esophageal high-resolution manometry. Neurogastroenterol Motil. 2013;25:762–e795.
Chen CL, Yi CH, Liu TT, Hsu CS, Omari TI. Characterization of esophageal pressure-flow abnormalities in patients with non-obstructive dysphagia and normal manometry findings. J Gastroenterol Hepatol. 2013;28:946–53.
Loots C, van Herwaarden MY, Benninga MA, VanderZee DC, van Wijk MP, Omari TI. Gastroesophageal reflux, esophageal function, gastric emptying, and the relationship to dysphagia before and after antireflux surgery in children. J Pediatr. 2013;162(3):566–73.
Dire C, Shi G, Manka M, Kahrilas PJ. Manometric characteristics of the upper esophageal sphincter recorded with a microsleeve. Am J Gastroenterol. 2001;96:1383–9.
Williams RB, Wallace KL, Ali GN, Cook IJ. Biomechanics of failed deglutitive upper esophageal sphincter relaxation in neurogenic dysphagia. Am J Physiol. 2002;283:G16–26.
Ren J, Massey BT, Dodds WJ, Kern MK, Brasseur JG, Shaker R, Harrington SS, Hogan WJ, Arndorfer RC. Determinants of intrabolus pressure during esophageal peristaltic bolus transport. Am J Physiol. 1993;264:G407–13.
Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Kahrilas PJ. Deglutitive upper esophageal sphincter relaxation: a study of 75 volunteer subjects using solid-state high-resolution manometry. Am J Physiol. 2006;291:G525–31.
Lazarus C, Logemann JA, Song CW, Rademaker AW, Kahrilas PJ. Effects of voluntary maneuvers on tongue base function for swallowing. Folia Phoniatr et Logop. 2002;54:171–6.
Logemann JA, Kahrilas PJ, Kobara M, Vakil NB. The benefit of head rotation on pharyngoesophageal dysphagia. Arch Phys Med Rehabil. 1989;70:767–71.
Hind JA, Nicosia MA, Roecker EB, Carnes ML, Robbins J. Comparison of effortful and noneffortful swallows in healthy middle-aged and older adults. Arch Phys Med Rehabil. 2001;82:1661–5.
Takasaki K, Umeki H, Enatsu K, Tanaka F, Sakihama N, Kumagami H, Takahashi H. Investigation of pharyngeal swallowing function using high-resolution manometry. Laryngoscope. 2008;118:1729–32.
McCulloch TM, Hoffman MR, Ciucci MR. High-resolution manometry of pharyngeal swallow pressure events associated with head turn and chin tuck. Ann Otol Rhinol Laryngol. 2010;119:369–76.
Umeki H, Takasaki K, Enatsu K, Tanaka F, Kumagami H, Takahashi H. Effects of a tongue-holding maneuver during swallowing evaluated by high-resolution manometry. Otolaryngology. 2009;141(1):119–22.
Hoffman MR, Ciucci MR, Mielens JD, Jiang JJ, McCulloch TM. Pharyngeal swallow adaptations to bolus volume measured with high-resolution manometry. Laryngoscope. 2010;120:2367–73.
Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut. 2008;57:405–23.
Knigge MA, Thibeault S, McCulloch TM. Implementation of high-resolution manometry in the clinical practice of speech language pathology. Dysphagia. 2014;29:2–16.
Jones CA, Ciucci MR, Hammer MJ, McCulloch TM. A multisensor approach to improve manometric analysis of the upper esophageal sphincter. Laryngoscope. 2016;126:657–64.
Geng Z, Hoffman MR, Jones CA, McCulloch TM, Jiang JJ. Three-dimensional analysis of pharyngeal high-€∙resolution manometry data. The Laryngoscope. 2013;123:1746–53.
Ryu JS, Park D, Kang JY. Application and interpretation of high-resolution manometry for pharyngeal dysphagia. J Neurogastroenterol Motil. 2015;21(2):283–7.
Isberg A, Nilsson ME, Schiratzki H. The upper esophageal sphincter during normal deglutition. A simultaneous cineradiographic and manometric investigation. Acta Radiol. 1985;26(5):563–8.
Sokol EM, Heitmann P, Wolf BS, Cohen BR. Simultaneous cineradiographic and manometric study of the pharynx, hypopharynx, and cervical esophagus. Gastroenterology. 1966;51:960–74.
Jacob P, Kahrilas PJ, Logemann JA, Shah V, Ha T. Upper esophageal sphincter opening and modulation during swallowing. Gastroenterology. 1989;97:1469–78.
Omari TI, Hammer MJ, Cock C, Dinning PG, Wiklendt L, Costa MC, McCulloch TM, Jones CAMC-S. Predicting the activation states of the muscles governing upper esophageal sphincter relaxation and opening. Am J Physiol Gastrointest Liver Physiol. 2016;310(6):G359–66.
Kwiatek MA, Mirza F, Kahrilas PJ, Pandolfino JE. Hyperdynamic upper esophageal sphincter pressure: a manometric observation in patients reporting globus sensation. Am J Gastroenterol. 2009;104:289–98.
Cook IJ, Dent J, Shannon S, Collins SM. Measurement of upper esophageal sphincter pressure. Effect of acute emotional stress. Gastroenterology. 1987;93:526–32.
Mason RJ, Bremner CG, DeMeester TR, Crookes PF, Peters JH, Hagen JA, DeMeester SR. Pharyngeal swallowing disorders: selection for and outcome after myotomy. Ann Surg. 1998;228:598–608.
Pouderoux P, Kahrilas PJ. Function of upper esophageal sphincter during swallowing: the grabbing effect. Am J Physiol. 1997;272:G1057–63.
Acknowledgments
The authors would like to acknowledge University of Wisconsin-Madison Department of Surgery biostatisticians Glen Leverson, Ph.D., and Ying Shan, M.S., for their assistance with statistical analysis. The authors would also like to acknowledge Levi Brown, B.A., and William Bleifuss, B.S., for their assistance with data analysis.
Funding
This research was supported by National Institutes of Health Grant Number 1R21DC011130-01A1. CAJ was also supported by T32GM007507.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Walczak, C.C., Jones, C.A. & McCulloch, T.M. Pharyngeal Pressure and Timing During Bolus Transit. Dysphagia 32, 104–114 (2017). https://doi.org/10.1007/s00455-016-9743-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9743-5