Abstract
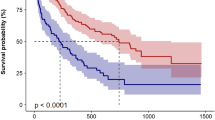
Dysphagia and malnutrition seem to be associated, but little research in detail has been reported. We aimed to clarify the association between dysphagia and malnutrition by adopting accurate diagnosis and mathematical evaluation of dysphagia using videofluorography and nutritional assessment calculated by a well-established nutritional risk index. We conducted a retrospective analysis of 165 enrolled patients who were admitted to our hospital for acute diseases and underwent videofluorography on suspicion of dysphagia in the year 2016. We diagnosed high-risk dysphagia in patients with 8-point penetration–aspiration scale (PAS) score over 4. We used the geriatric nutritional risk index (GNRI) as a nutritional assessment tool. A GNRI score less than 91.2 corresponds to malnutrition. The median age of 165 enrolled patients was 76.0, and the number of female patients was 53. The mean GNRI was 81.2, and 134 patients (81.2%) had malnutrition. The number of the patients with a diagnosis of high-risk dysphagia was 54 (32.7%). The GNRI of patients with high-risk dysphagia was significantly less than that of patients without (mean value 77.7 ± 10.5 vs. 83.0 ± 10.5, P = 0.003). GNRI < 91.2 was independently and significantly associated with high-risk dysphagia (OR 3.094; CI 1.057–9.058; P = 0.039). Based on the current study, the authors propose evaluating nutritional status to predict dysphagia risk of patients in the acute phase.

Similar content being viewed by others
References
United Nations, Department of Economic and Social Affairs, Population Division. World population prospects: the 2015 revision, key findings and advance. 2015.
Dziewas R, Beck AM, Clave P, et al. Recognizing the importance of dysphagia: stumbling blocks and stepping stones in the twenty-first century. Dyspagia. 2016;. doi:10.1007/s00455-016-9746-2.
Martino R, Foley N, Bhogal S, et al. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Pirlich M, Schütz T, Norman K, et al. The German hospital malnutrition study. Clin Nutr. 2006;25:563–72.
Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22:235–9.
Carrión S, Cabré S, Monteis R, et al. Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clin Nutr. 2015;34:436–42.
Serra-Prat M, Hinojosa G, López D, et al. Prevalence of oropharyngeal dysphagia and impaired safety and efficacy of swallow in independently living older persons. J Am Geriatr Soc. 2011;59:186–7.
Nishioka S, Okamoto T, Takayama M, et al. Malnutrition risk predicts recovery of full oral intake among older adult stroke patients undergoing enteral nutrition: secondary analysis of a multicentre survey (the APPLE study). Clin Nutr. 2016;. doi:10.1016/j.cinu2016.06.028.
Kaiser MJ, Bauer JM, Rämsch C, et al. Mini nutritional assessment international group. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58:578–83.
Horner J, Massey EW. Silent aspiration following stroke. Neurology. 1998;38:317–9.
Smith HA, Lee SH, O’Neill PA, et al. The combination of bedside swallowing assessment and oxygen saturation monitoring of swallowing in acute stroke: a safe and humane screening tool. Age Ageing. 2000;29:495–9.
Ramsey D, Smithard DG, Kalra L. Early assessment of dysphagia and aspiration risk in acute stroke patients. Stroke. 2003;34:1252–7.
Takeuchi K, Aida J, Furuta M, et al. Nutritional status and dysphagia risk among community-dwelling frail older adults. J Nutr Health Aging. 2014;18:352–7.
Kawashima K, Motohashi Y, Fujishima I. Prevalence of dysphagia among community-dwelling elderly individuals as estimated using a questionnaire for dysphagia screening. Dysphagia. 2004;19:266–71.
Steele CM, Grace-Martin K. Reflections on clinical and statistical use of the penetration-aspiration scale. Dysphagia. 2017;. doi:10.1007/s00455-017-9809-z.
Moon JH, Jung JH, Won YS, et al. Effects of expiratory muscle strength training on swallowing function in acute stroke patients with dysphagia. J Phys Ther Sci. 2017;29:609–12.
Tabor L, Gaziano J, Watts S, et al. Defining swallowing-related quality of life profiles in individuals with amyotrophic lateral sclerosis. Dysphagia. 2016;31:376–82.
Lee JH, Lee KW, Kim SB, et al. The functional dysphagia scale is a useful tool for predicting aspiration pneumonia in patients with Parkinson disease. Ann Rehabil Med. 2016;40:440–6.
Tutor JD, Srinivasan S, Gosa MM, et al. Pulmonary function in infants with swallowing dysfunction. PLoS ONE. 2015;10:e0123125.
Krisciunas GP, Castellano K, McCulloch TM, et al. Impact of compliance on dysphagia rehabilitation in head and neck cancer patients: results from a multi-center clinical trial. Dysphagia. 2017;32:327–36.
The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group. Perioperative total parenteral nutrition in surgical patients. N Engl J Med. 1991;47:366–81.
Buzby GP, Knox LS, Crosby LO, et al. Study protocol: a randomized clinical trial of total parenteral nutrition in malnourished surgical patients. Am J Clin Nutr. 1988;47:366–81.
Bouillanne O, Morineau G, Dupont C, et al. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82:277–83.
Yamada K, Furuya R, Takita T, et al. Simplified nutritional screening tools for patients on maintenance hemodialysis. Am J Clin Nutr. 2008;87:106–13.
Cereda E, Pedrolli C. The use of the geriatric nutritional risk index (GNRI) as a simplified nutritional screening tool. Am J Clin Nutr. 2008;87:1966–7.
James WP, Francois PJ. The choice of cut-off point for distinguishing normal body weights from underweight or ‘chronic energy deficiency’ in adults. Eur J Clin Nutr. 1994;48:S179.
Kuzuya M, Kanda S, Koike T, et al. Evaluation of mini-nutritional assessment for Japanese frail elderly. Nutrition. 2005;21:498–503.
Kidd D, Lawson J, Nesbitt R, et al. Aspiration in acute stroke: a clinical study with videofluoroscopy. QJM. 1993;86:825–9.
Gates J, Hartnell GG, Gramigna GD. Videofluoroscopy and swallowing studies for neurologic disease: a primer. Radiographics. 2005;26:e22.
Splaingard ML, Hutchins B, Sulton LD, et al. Aspirations in rehabilitation patients: videofluoroscopy vs. bedside clinical assessment. Arch Phys Med Rehabil. 1988;69:637–40.
Rosenbek JC, Robbins JA, Roecker EB, et al. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Robbins J, Coyle J, Rosenbek J, et al. Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia. 1999;14:228–32.
Yoshikawa M, Yoshida M, Nagasaki T, et al. Aspects of swallowing in healthy dentate elderly persons older than 80 years. J Gerontol A Biol Sci Med Sci. 2005;60:506–9.
Veldee MS, Peth LD. Can protein-calorie malnutrition cause dysphagia? Dysphagia. 1992;7:86–101.
Saito T, Hayashi K, Nakazawa H, et al. Clinical characteristics and lesions responsible for swallowing hesitation after acute cerebral infarction. Dysphagia. 2016;31:567–73.
Ghosh S, Vaid K, Mohan M, et al. Effect of degree and duration of protein-calorie malnutrition and well nourished children. J Neurol Neurosurg Psychiatry. 1979;42:760–3.
Kumar A, Ghai OP, Singh N. Delayed nerve conduction velocities in children with protein-calorie malnutrition. J Pediatr. 1977;90:149–53.
Keys A, Brozek J, Henschel A, et al. The biology of human starvation, vol. 1. Minneapolis: University of Minnesota Press; 1950. p. 184–208.
Wurtman RJ, Fernstrom JD. Control of brain neurotransmitter synthesis by precursor availability and nutritional state. Biochem Pharmacol. 1976;25:1691–6.
Kessler JP, Jean A. Inhibitory influence of monoamines and brainstem monoaminergic regions of the medullary swallowing reflex. Neurochi Lett. 1986;65:41–6.
Leslie P, Drinnan MJ, Ford GA, et al. Swallow respiratory patterns and aging: presbyphagia or dysphagia? J Gerontol A Biol Sci Med Sci. 2005;60:391–5.
Sura L, Madhavan A, Carnaby G, et al. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012;7:287–98.
Ney DM, Weiss JM, Kind AJ, et al. Senescent swallowing: impact, strategies, and interventions. Nutr Clin Pract. 2009;24:395–413.
Moreira NC, Krausch-Hofmann S, Matthys C, et al. Risk factors for malnutrition in older adults: a systematic review of the literature based on longitudinal data. Adv Nutr. 2016;16:507–22.
Wysokiński A, Sobów T, Kłoszewska I, Kostka T. Mechanisms of the anorexia of aging-a review. Age. 2015;37:81.
Takata Y, Ansai T, Soh I, et al. Body mass index and disease-specific mortality in an 80-year-old population at the 12-year follow-up. Arch Gerontol Geriatr. 2013;57:46–53.
Ballmer PE. Causes and mechanisms of hypoalbuminemia. Clin Nutr. 2001;20:271–3.
Jones CH, Smye SW, Newstead CG, et al. Extracellular fluid volume determined by bioelectric impedance and serum albumin in CAPD patients. Nephrol Dial Transpl. 1998;13:393–7.
Carrión S, Roca M, Costa A, et al. Nutritional status of older patients with oropharyngeal dysphagia in a chronic versus an acute clinical situation. Clin Nutr. 2016;. doi:10.1016/j.clnu.2016.07.009.
Garrow J. Starvation in hospital. BMJ. 1994;308:934.
Gariballa SE, Parker SG, Taub N, et al. Nutritional status of hospitalized acute stroke patients. Br J Nutr. 1998;79:481–7.
Yoo SH, Kim JS, Kwon SU, et al. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol. 2008;65:39–43.
Gyan E, Raynard B, Durand JP, et al. NutriCancer2012 Investigator Group. Malnutrition in patients with cancer. JPEN J Parenter Enteral Nutr. 2017;1:148607116688881. doi:10.1177/0148607116688881.
Saitoh M, Dos Santos MR, Ebner N, et al. Nutritional status and its effects on muscle wasting in patients with chronic heart failure: insights from studies investigating co-morbidities aggravating heart failure. Wien Klin Wochenschr. 2016;128:497–504.
Collins PF, Eila M, Kurukulaaratchy RJ, et al. The influence of deprivation on malnutrition risk in outpatients with chronic obstructive pulmonary disease (COPD). Clin Nutr. 2016;. doi:10.1016/j.clnu.2016.11.005.
Gonzalez Lindh M, Blom Johansson M, Jennische M, et al. Prevalence of swallowing dysfunction screened in Swedish cohort of COPD patients. Int J Obstruct Pulmon Dis. 2017;12:331–7.
Pikus L, Levine MS, Yang YX, et al. Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. Am J Roentgenol. 2003;180:1613–6.
Ribeiro PW, Cola PC, Gatto AR, et al. Relationship between dysphagia, national institutes of health stroke scale score, and predictors of pneumonia after ischemic stroke. J Stroke Cerebrovasc Dis. 2015;24:2088–94.
Nii M, Maeda K, Wakabahashi H, et al. Nutritional improvement and energy intake are associated with functional recovery in patients after cerebrovascular disorders. J Stroke Cerebrovasc Dis. 2016;25:57–62.
Davies M. Nutritional screening and assessment in cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9:S64–73.
Acknowledgements
We thank Mayumi Ito, nurse in our department, for her excellent management and assistance in VF.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Saito, T., Hayashi, K., Nakazawa, H. et al. A Significant Association of Malnutrition with Dysphagia in Acute Patients. Dysphagia 33, 258–265 (2018). https://doi.org/10.1007/s00455-017-9855-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9855-6