Abstract
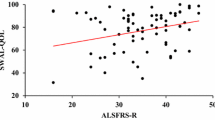
Dysphagia is common in individuals with amyotrophic lateral sclerosis (ALS) and associated with reductions in quality of life and health-related outcomes. Despite the high prevalence of dysphagia in ALS, functional impairment profiles of swallowing safety and efficiency have not been comprehensively examined. We therefore aimed to determine the relative prevalence of unsafe and inefficient swallowing in a large cohort of individuals with ALS. We further sought to examine the impact of global and bulbar disease progression (Amyotrophic Lateral Sclerosis Functional Rating Scale-Revised "ALSFRS-R" total and bulbar scores, respectively), disease duration, and onset type on swallowing impairment profiles. One hundred individuals with ALS completed a standardized videofluoroscopic swallowing examination Two independent and blinded raters performed validated ratings of safety (Penetration-Aspiration Scale, PAS) and efficiency (Analysis of Swallowing Physiology: Events, Kinematics, and Timing, ASPEKT % residue). Binary classifications of safety (unsafe: PAS ≥ 3), efficiency (inefficient: total residue ≥ 3% of C2-42) and global swallowing status were derived. The ALSFRS-R was completed to derive ALSFRS-R total and bulbar subscale scores. Demographic data (disease duration and onset type) for each participant was also recorded. Descriptives, 2 × 2 contingency tables with Fishers exact test, and independent samples t-tests were performed (α = 0.05). Prevalence of unsafe and inefficient swallowing was 48% and 73%, respectively. Global swallowing profiles were, in rank order: unsafe and inefficient (39%), inefficient but safe (34%), safe and efficient (18%), and unsafe but efficient (9%). There were no differences in global disease progression or disease duration across swallowing impairment profiles. ALSFRS-R bulbar subscale scores were significantly lower in unsafe versus safe swallowers, p < 0.05. Spinal onset patients had a greater proportion of safe swallowers as compared to bulbar onset patients (p = 0.000, Fisher's exact test). Both spinal and bulbar onset patients demonstrated a higher prevalence of inefficient swallowers as compared to efficient swallowers (p = 0.04, Fisher's exact test). Dysphagia was prevalent in this group of individuals with ALS. Approximately half demonstrated safety impairments and two-thirds had impairments in swallowing efficiency. Inefficient swallowing was approximately four times more likely to be the initial functional impairment in patients with one pathophysiologic functional impairment. A longitudinal study is needed to examine the temporal evolution of dysphagia in ALS.



Similar content being viewed by others
References
Chen A, Garrett CG. Otolaryngologic presentations of amyotrophic lateralsclerosis. Otolaryngol Head Neck Surg England. 2005;132:500–4.
Kuhnlein P, Gdynia H-J, Sperfeld A-D, Lindner-Pfleghar B, Ludolph AC, Prosiegel M, et al. Diagnosis and treatment of bulbar symptoms in amyotrophic lateral sclerosis. Nat Clin Pract Neurol England. 2008;4:366–74.
Logemann JA, Kahrilas PJ, Cheng J, Pauloski BR, Gibbons PJ, Rademaker AW, et al. Closure mechanisms of laryngeal vestibule during swallow. Am J Physiol United States. 1992;262:G338–44.
Vose A, Humbert I. “Hidden in Plain Sight”: a descriptive review of laryngeal vestibule closure. Dysphagia. 2019;34:281–9. https://doi.org/10.1007/s00455-018-9928-1.
Park T, Kim Y, Ko D-H, McCullough G. Initiation and duration of laryngeal closure during the pharyngeal swallow in post-stroke patients. Dysphagia United States. 2010;25:177–82.
Higo R, Tayama N, Nito T. Longitudinal analysis of progression of dysphagia in amyotrophic lateral sclerosis. Auris Nasus Larynx. 2004. https://doi.org/10.1016/j.anl.2004.05.009
Robbins J. Swallowing in ALS and motor neuron disorders. Neurol Clin. 1987;5:213–29.
Murono S, Hamaguchi T, Yoshida H, Nakanishi Y, Tsuji A, Endo K, et al. Evaluation of dysphagia at the initial diagnosis of amyotrophic lateral sclerosis. Auris Nasus Larynx. 2015;42:213–7.
Tabor L, Robison R, Wymer J, Plowman E. Mechanisms of Airway Protection in Individuals with ALS. Univ Florida T32 Neuroplast Train Progr Symp. Gainesville, FL; 2017.
Lo Re G, Galia M, La Grutta L, Russo S, Runza G, Taibbi A, et al. Digital cineradiographic study of swallowing in patients with amyotrophic lateral sclerosis. Radiol Med. 2007;112:1173–87.
Solazzo A, Del Vecchio L, Reginelli A, Monaco L, Sagnelli A, Monsorro M, et al. Search for compensation postures with videofluoromanometric investigation in dysphagic patients affected by amyotrophic lateral sclerosis. Radiol Med Italy. 2011;116:1083–94.
Gaziano J, Tabor L, Richter J, Plowman EK (2015) Prevalence Timing and Source of Aspiration in Individuals with ALS. Dysphagia Res Soc. Chicago, IL.
Tabor-Gray LC, Gallestagui A, Vasilopoulos T, Plowman EK. Characteristics of impaired voluntary cough function in individuals with amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener England. 2019;20:37–42.
Tabor-Gray L, Vasilopoulos T, Plowman EK. Differences in voluntary and reflexive cough strength in individuals with amyotrophic lateral sclerosis and healthy adults. Muscle Nerve. 2020;62:597–600. https://doi.org/10.1002/mus.27040.
Pearson W, Griffeth J, Ennis A. Functional anatomy underlying pharyngeal swallowing mechanics and swallowing performance goals. Perspect ASHA Spec Interes Groups. 2019;4:648–55. https://doi.org/10.1044/2019_PERS-SIG13-2018-0014.
Steele CM, Bayley MT, Peladeau-Pigeon M, Nagy A, Namasivayam AM, Stokely SL, et al. A Randomized Trial Comparing Two Tongue-Pressure Resistance Training Protocols for Post-Stroke Dysphagia. Dysphagia [Internet]. 2016;31:452–61. Available from: https://pubmed.ncbi.nlm.nih.gov/26936446
Dejaeger E, Pelemans W, Ponette E, Joosten E. Mechanisms involved in postdeglutition retention in the elderly. Dysphagia. 1997;12:63–7.
Logemann JA. Critical Factors in the Oral Control Needed for Chewing and Swallowing. J Texture Stud [Internet]. 2014;45:173–9. Available from: https://pubmed.ncbi.nlm.nih.gov/25386030
Corbin-Lewis K, Liss JM. Clinical Anatomy & Physiology of the Swallow Mechanism [Internet]. Cengage Learning; 2014. Available from: https://books.google.com/books?id=1nTzAgAAQBAJ
Walczak CC, Jones CA, McCulloch TM. Pharyngeal Pressure and Timing During Bolus Transit. Dysphagia [Internet]. 2017;32:104–14. Available from: https://pubmed.ncbi.nlm.nih.gov/27565155
Waito AA, Valenzano TJ, Peladeau-Pigeon M, Steele CM. Trends in research literature describing dysphagia in motor neuron diseases (MND): a scoping review. Dysphagia. 2017;32:734–47.
Waito A, Plowman E, Barbon C, Peladeau-Pigeon M, Tabor-Gray L, Magennis K, et al. A cross-sectional, quantitative videofluoroscopic analysis of swallowing physiology and function in individuals with amyotrophic lateral sclerosis. J Speech Lang Hear Res. 2020;63:948–62. https://doi.org/10.1044/2020_JSLHR-19-00051.
Chio A, Logroscino G, Hardiman O, Swingler R, Mitchell D, Beghi E, et al. Prognostic factors in ALS: A critical review. Amyotroph Lateral Scler [Internet]. 2009/11/20. 2009;10:310–23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19922118
Watts CR, Vanryckeghem M. Laryngeal dysfunction in amyotrophic lateral sclerosis: a review and case report. BMC Ear Nose Throat Disord. 2001;1:1. https://doi.org/10.1186/1472-6815-1-1.
Pouderoux P, Kahrilas PJ. Deglutitive tongue force modulation by volition, volume, and viscosity in humans. Gastroenterology [Internet]. 1995;108:1418–26. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7729634
Kahrilas PJ, Lin S, Logemann JA, Ergun GA, Facchini F. Deglutitive tongue action: volume accommodation and bolus propulsion. Gastroenterol. 1993;104:152–62.
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, et al. The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. J Neurol Sci. 1999;169:13–21.
Lechtzin N, Rothstein J, Clawson L, Diette GB, Wiener CM. Amyotrophic lateral sclerosis: evaluation and treatment of respiratory impairment. Amyotroph Lateral Scler Other Mot Neuron Disord [Internet]. Taylor & Francis Ltd; 2002;3:5–13. Available from: http://lp.hscl.ufl.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=aph&AN=6798016&site=eds-live
Ferrari R, Kapogiannis D, Huey ED, Momeni P. FTD and ALS: a tale of two diseases. Curr Alzheimer Res [Internet]. 2011;8:273–94. Available from: https://pubmed.ncbi.nlm.nih.gov/21222600
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Molfenter SM, Brates D, Herzberg E, Noorani M, Lazarus C. The Swallowing Profile of Healthy Aging Adults: Comparing Noninvasive Swallow Tests to Videofluoroscopic Measures of Safety and Efficiency. J Speech Lang Hear Res [Internet]. American Speech-Language-Hearing Association; 2018;61:1603–12. Available from: https://pubmed.ncbi.nlm.nih.gov/29893767
Namasivayam-MacDonald AM, Riquelme LF. Quantifying Airway Invasion and Pharyngeal Residue in Patients with Dementia. Geriatr (Basel, Switzerland) [Internet]. MDPI; 2019;4:13. Available from: https://pubmed.ncbi.nlm.nih.gov/31023981
Plowman EK, Watts SA, Robison R, Tabor L, Dion C, Gaziano J, et al. Voluntary Cough Airflow Differentiates Safe versus Unsafe Swallowing in Amyotrophic Lateral Sclerosis. Dysphagia [Internet]. 2016;31:383–90. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4871758/
Steele CM, Peladeau-Pigeon M, Barbon CAE, Guida BT, Namasivayam-MacDonald AM, Nascimento WV, et al. Reference values for healthy swallowing across the range from thin to extremely thick liquids. J Speech Lang Hear Res. 2019;62:1338–63.
Steele CM, Peladeau-Pigeon M, Barrett-Connor E, Wolkin TS. What is the Risk of Penetration-Aspiration Related to Residue in the Pharynx? Dysphagia Res Soc Annu Meet. San Juan, Puerto Rico; 2020.
McHugh ML. Interrater reliability: the kappa statistic. Biochem medica [Internet]. Croatian Society of Medical Biochemistry and Laboratory Medicine; 2012;22:276–82. Available from: https://pubmed.ncbi.nlm.nih.gov/23092060
Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med [Internet]. 2016;15:155–63. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1556370716000158
Isaacs JD, Dean AF, Shaw CE, Al-Chalabi A, Mills KR, Leigh PN. Amyotrophic lateral sclerosis with sensory neuropathy: part of a multisystem disorder? J Neurol Neurosurg Psychiatry [Internet]. BMJ Group; 2007;78:750–3. Available from: https://pubmed.ncbi.nlm.nih.gov/17575021
Troche MS, Brandimore AE, Okun MS, Davenport PW, Hegland KW. Decreased cough sensitivity and aspiration in Parkinson disease. Chest [Internet]. American College of Chest Physicians; 2014;146:1294–9. Available from: https://pubmed.ncbi.nlm.nih.gov/24968148
Fullerton A, Mou Y, Silver N, Chheda N, Bolser DC, Wheeler-Hegland K. Impact of Tussigenic Stimuli on Perceived Upper Airway Sensation and Motor Cough Response Following Total Laryngectomy. Front Physiol [Internet]. Frontiers Media S.A.; 2020;11:477. Available from: https://pubmed.ncbi.nlm.nih.gov/32547408
Rogus-Pulia NM, Plowman EK. Shifting tides toward a proactive patient-centered approach in dysphagia management of neurodegenerative disease. Am J speech-language Pathol United States. 2020;29:1094–109.
PE K. Is there a role for exercise in the management of bulbar dysfunction in amyotrophic lateral sclerosis? J Speech Lang Hear Res. 2015;58:1151–66. https://doi.org/10.1044/2015_JSLHR-S-14-0270.
DePaul R, Brooks BR. Multiple orofacial indices in amyotrophic lateral sclerosis. J Speech Hear Res [Internet]. 1993/12/01. 1993;36:1158–67. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8114482
DePaul R, Abbs JH, Caligiuri M, Gracco VL, Brooks BR. Hypoglossal, trigeminal, and facial motoneuron involvement in amyotrophic lateral sclerosis. Neurology [Internet]. 1988;38:281. Available from: http://n.neurology.org/content/38/2/281.abstract
Langmore SE, Lehman ME. Physiologic deficits in the orofacial system underlying dysarthria in amyotrophic lateral sclerosis. J Speech Hear Res [Internet]. 1994;37:28–37. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8170127
Hillel AD, Miller R. Bulbar amyotrophic lateral sclerosis: patterns of progression and clinical management. Head Neck. 1989;11:51–9.
Molfenter SM, Steele CM. The relationship between residue and aspiration on the subsequent swallow: an application of the normalized residue ratio scale. Dysphagia. 2013;28:494–500.
Simon NG, Turner MR, Vucic S, Al-Chalabi A, Shefner J, Lomen-Hoerth C, et al. Quantifying disease progression in amyotrophic lateral sclerosis. Ann Neurol [Internet]. BlackWell Publishing Ltd; 2014;76:643–57. Available from: https://pubmed.ncbi.nlm.nih.gov/25223628
Onesti E, Schettino I, Gori MC, Frasca V, Ceccanti M, Cambieri C, et al. Dysphagia in amyotrophic lateral sclerosis: impact on patient behavior, diet adaptation, and riluzole management. Front Neurol. 2017;8:94.
Acknowledgements
We would like to thank Dr. Catriona Steele of the Swallowing Rehabilitation Research Laboratory for lending her scientific expertise and insight to support this research. This manuscript was (partially) prepared with the use of resources and facilities at the William S. Middleton Memorial Veterans Hospital, Madison WI (GRECC Manuscript 008-2021). The views and content expressed in this article are solely the responsibility of the authors and do not necessarily reflect the position, policy, or official views of the Department of Veterans Affairs, the U.S. Government, or the NIH. This work was based on a dissertation chapter submitted by the first author to the University of Florida in partial fulfillment of requirements for the degree of Doctor of Philosophy.
Funding
This work was supported by National Institute of Neurological Disorders and Stroke (NINDS) Grant Numbers: 1R01 NS100859-01, 5R01NS10859-02S1, and 1F99 NS115339-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Robison, R., DiBiase, L., Ashley, A. et al. Swallowing Safety and Efficiency Impairment Profiles in Individuals with Amyotrophic Lateral Sclerosis. Dysphagia 37, 644–654 (2022). https://doi.org/10.1007/s00455-021-10315-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-021-10315-2