Abstract
Background
Ulcer perforation carries up to a 30 % 1-year mortality rate. Intervention-related adverse events are among statistically significant predictors of 1-year mortality. A natural orifice transluminal endoscopic surgical (NOTES) approach may be less invasive and may decrease procedure-related adverse events by diminishing the so-called second hit, thus leading to decreased morbidity and mortality. We sought to assess the feasibility of an endoscopic transluminal omental plug technique in patients with perforated gastroduodenal ulcers under laparoscopic guidance.
Methods
Patients with suspected acute gastroduodenal ulcer perforations were offered participation in this prospective pilot study. Closure of the perforation was attempted using the NOTES omental plug technique. Demographic, clinical, endoscopic, and radiographic data were abstracted, as were data for morbidity, mortality, and pilot data regarding quality of life (QOL).
Results
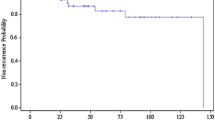
From February 2010 through February 2012, a total of 17 patients presented to a tertiary care center with clinically suspected perforated ulcer. Of seven patients (mean age 79 years, range 64–89 years) who consented to the study, three underwent the study procedure. All patients had multiple comorbidities. Two patients presented with 4–6 mm perforated peptic ulcers and underwent successful laparoscopic-assisted NOTES omental and falciform ligament patch closure, respectively. Postoperative radiographic contrast studies showed no leak, and patients were discharged home on postoperative days 3 and 4. The third patient had undergone enterocutaneous fistula repair with herniorrhaphy 6 weeks before. Although a transluminal endoscopic approach was feasible, the omentum was under too much tension to be secured. This procedure was converted to an open omental patch repair. For all but one patient who provided consent, obtaining QOL data was feasible.
Conclusions
Initial results from a laparoscopic-assisted NOTES approach for closure of perforated peptic ulcers appear promising and enable swift recovery in selected patients. This is especially important in elderly and/or immunocompromised patients. Technical details and patient selection criteria continue to evolve.








Similar content being viewed by others
References
Kashiwagi H (2007) Ulcer and gastritis. Endoscopy 39:101–105
Svanes C (2000) Trends in perforated peptic ulcer: incidence, etiology, treatment, and prognosis. World J Surg 24:277–283
Thorsen K, Glomsaker TB, von Meer A, Soreide K, Soreide JA (2011) Trends in diagnosis and surgical management of patients with perforated peptic ulcer. J Gastrointest Surg 15:1329–1335
Imhof M, Epstein S, Ohmann C, Roher HD (2008) Duration of survival after peptic ulcer perforation. World J Surg 32:408–412
Bonin EA, Moran E, Gostout CJ, McConico AL, Zielinski M, Bingener J (2012) Natural orifice transluminal endoscopic surgery for patients with perforated peptic ulcer. Surg Endosc 26:1534–1538
Graham R (1937) The treatment of perforated duodenal ulcers. Surg Gynecol Obstet 64:235–238
Turner WW Jr, Thompson WM Jr, Thal ER (1988) Perforated gastric ulcers. A plea for management by simple closures. Arch Surg 123:960–964
Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson JJ, Chung SC, Li AK (1996) A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg 224:131–138
Siu WT, Leong HT, Law BKB, Chau CH, Li ACN, Fung KH, Tai YP, Li MKW (2002) Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg 235:313–319
Lam PWF, Lam MCS, Hui EKL, Sun YW, Mok FPT (2005) Laparoscopic repair of perforated duodenal ulcers: the “three-stitch” Graham patch technique. Surg Endosc 19:1627–1630
So JB, Kum CK, Fernandes ML, Goh P (1996) Comparison between laparoscopic and conventional omental patch repair for perforated duodenal ulcer. Surg Endosc 10:1060–1063
Moran EA, Gostout CJ, McConico AL, Bingener J (2010) Natural orifice translumenal endoscopic surgery used for perforated viscus repair is feasible using lower peritoneal pressures than laparoscopy in a porcine model. J Am Coll Surg 210:474–479
Hashiba K, Carvalho AM, Diniz G Jr, Barbosa de Aridrade N, Guedes CA, Siqueira Filho L, Lima CA, Coehlo HE, de Oliveira RA (2001) Experimental endoscopic repair of gastric perforations with an omental patch and clips. Gastrointest Endosc 54:500–504
Korolija D, Sauerland S, Wood-Dauphinee S, Abbou CC, Eypasch E, Caballero MG, Lumsden MA, Millat B, Monson JR, Nilsson G, Pointner R, Schwenk W, Shamiyeh A, Szold A, Targarona E, Ure B, Neugebauer E (2004) Evaluation of quality of life after laparoscopic surgery: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc 18:879–897
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmulling C, Neugebauer E, Troidl H (1995) Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg 82:216–222
Urbach DR, Harnish JL, McIlroy JH, Streiner DL (2006) A measure of quality of life after abdominal surgery. Qual Life Res 15:1053–1061
Boey J, Choi SK, Poon A, Alagaratnam TT (1987) Risk stratification in perforated duodenal ulcers. A prospective validation of predictive factors. Ann Surg 205:22–26
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Lee KH, Chang HC, Lo CJ (2004) Endoscope-assisted laparoscopic repair of perforated peptic ulcers. Am Surg 70:352–356
Pescatore P, Halkic N, Calmes JM, Blum A, Gillet M (1998) Combined laparoscopic–endoscopic method using an omental plug for therapy of gastroduodenal ulcer perforation. Gastrointest Endosc 48:411–414
Costalat G, Alquier Y (1995) Combined laparoscopic and endoscopic treatment of perforated gastroduodenal ulcer using the ligamentum teres hepatis (LTH). Surg Endosc 9:677–679
Marks J, Ponsky J, Pearl J, McGee M (2007) PEG “rescue”: a practical NOTES technique. Surg Endosc 21:816–819
Acknowledgments
Supported in part by a NOSCAR Grant and CTSA support (ULIRR024150).
Disclosures
Drs. Bingener, Loomis, Gostout, Zielinski, Buttar, Wong Kee Song, Baron, Ghahfarokhi, and Rajan have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bingener, J., Loomis, E.A., Gostout, C.J. et al. Feasibility of NOTES omental plug repair of perforated peptic ulcers: results from a clinical pilot trial. Surg Endosc 27, 2201–2208 (2013). https://doi.org/10.1007/s00464-012-2740-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2740-3



