Abstract
Background
The Universal Health Coverage goals call for access to affordable palliative care to reduce inequities in “total pain” and suffering. To achieve this, a patient-centred understanding of these inequities is required.
Aim
To assess association of total pain and suffering (i.e. physical, psychological, social, and spiritual health outcomes) and perceived health care quality with financial difficulties among stage IV solid malignancy patients.
Design
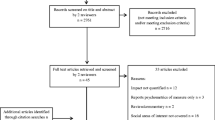
Using baseline data from the COMPASS cohort study, we assessed total pain and suffering including physical (physical and functional well-being, pain, symptom burden), psychological (anxiety, depression, emotional well-being), social (social well-being), and spiritual (spiritual well-being, hope) outcomes and perceived health care quality (physician communication, nursing care, and coordination/responsiveness). Financial difficulties were scored by assessing patient perception of the extent to which their resources were meeting expenses for their treatments, daily living, and other obligations. We used multivariable linear/logistic regression to test association between financial difficulties and each patient-reported outcome.
Setting/participants
Six hundred stage IV solid malignancy patients in Singapore.
Results
Thirty-five percent reported difficulty in meeting expenses. A higher financial difficulties score was associated with worse physical, psychological, social, spiritual outcomes, and lower perceived quality of health care coordination and responsiveness (i.e. greater total pain and suffering) (all p < 0.05). These associations persisted after adjustment for socio-economic indicators.
Conclusion
Results identify advanced cancer patients with financial difficulties to be a vulnerable group with greater reported total pain and suffering. A holistic patient-centred approach to care at end-of-life may help meet goals for Universal Health Coverage.
Similar content being viewed by others
References
Clark D (1999) ‘Total pain’, disciplinary power and the body in the work of Cicely Saunders, 1958-1967. Soc Sci Med 49:727–736
Krikorian A, Limonero JT, Maté J (2012) Suffering and distress at the end-of-life. Psycho-Oncology. 21:799–808
Wilson KG, Chochinov HM, McPherson CJ, LeMay K, Allard P, Chary S, Gagnon PR, Macmillan K, de Luca M, O'Shea F, Kuhl D, Fainsinger RL (2007) Suffering with advanced cancer. J Clin Oncol 25:1691–1697
Knaul FM, Farmer PE, Krakauer EL, de Lima L, Bhadelia A, Jiang Kwete X, Arreola-Ornelas H, Gómez-Dantés O, Rodriguez NM, Alleyne GAO, Connor SR, Hunter DJ, Lohman D, Radbruch L, del Rocío Sáenz Madrigal M, Atun R, Foley KM, Frenk J, Jamison DT, Rajagopal MR, Lancet Commission on Palliative Care and Pain Relief Study Group (2018) Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: the Lancet Commission report. Lancet. 391:1391–1454
Gwyther L, Brennan F, Harding R (2009) Advancing palliative care as a human right. J Pain Symptom Manag 38:767–774
Langa KM, Fendrick AM, Chernew ME, Kabeto MU, Paisley KL, Hayman JA (2004) Out-of-pocket health-care expenditures among older Americans with cancer. Value Health 7:186–194
Davidoff AJ, Erten M, Shaffer T, Shoemaker JS, Zuckerman IH, Pandya N, Tai MH, Ke X, Stuart B (2013) Out-of-pocket health care expenditure burden for Medicare beneficiaries with cancer. Cancer. 119:1257–1265
Bernard DS, Farr SL, Fang Z (2011) National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. J Clin Oncol 29:2821–2826
Stump TK, Eghan N, Egleston BL et al (2013) Cost concerns of patients with cancer. J Oncol Pract 9:251–257
Barbaret C, Brosse C, Rhondali W et al (2017) Financial distress in patients with advanced cancer. PLoS One 12:e0176470
Gupta D, Lis CG, Grutsch JF (2007) Perceived cancer-related financial difficulty: implications for patient satisfaction with quality of life in advanced cancer. Support Care Cancer 15:1051–1056
Delgado-Guay M, Ferrer J, Rieber AG, Rhondali W, Tayjasanant S, Ochoa J, Cantu H, Chisholm G, Williams J, Frisbee-Hume S, Bruera E (2015) Financial distress and its associations with physical and emotional symptoms and quality of life among advanced cancer patients. Oncologist. 20:1092–1098
Arman M, Rehnsfeldt A, Lindholm L, Hamrin E, Eriksson K (2004) Suffering related to health care: a study of breast cancer patients’ experiences. Int J Nurs Pract 10:248–256
Ramsey SD, Bansal A, Fedorenko CR, Blough DK, Overstreet KA, Shankaran V, Newcomb P (2016) Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol 34:980–986
Perrone F, Jommi C, Di Maio M et al (2016) The association of financial difficulties with clinical outcomes in cancer patients: secondary analysis of 16 academic prospective clinical trials conducted in Italy. Ann Oncol 27:2224–2229
Zafar SY, Abernethy AP (2013) Financial toxicity, Part II: how can we help with the burden of treatment-related costs? Oncology (Williston Park) 27:253–254 6
Zafar SY, Abernethy AP (2013) Financial toxicity, part I: a new name for a growing problem. Oncology (Williston Park) 27:80–81 149
Zafar SY, Peppercorn JM, Schrag D, Taylor DH, Goetzinger AM, Zhong X, Abernethy AP (2013) The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 18:381–390
Weissman JS, Schneider EC (2005) Social disparities in cancer: lessons from a multidisciplinary workshop. Cancer Causes Control 16:71–74
Byers TE, Wolf HJ, Bauer KR, Bolick-Aldrich S, Chen VW, Finch JL, Fulton JP, Schymura MJ, Shen T, van Heest S, Yin X, Patterns of Care Study Group (2008) The impact of socioeconomic status on survival after cancer in the United States : findings from the National Program of Cancer Registries Patterns of Care Study. Cancer. 113:582–591
Cheyne L, Taylor A, Milton R, Fear J, Callister ME (2013) Social deprivation does not affect lung cancer stage at presentation or disease outcome. Lung Cancer 81:247–251
Fagundes C, Jones D, Vichaya E, Lu C, Cleeland CS (2014) Socioeconomic status is associated with depressive severity among patients with advanced non-small-cell lung cancer: treatment setting and minority status do not make a difference. J Thorac Oncol 9:1459–1463
Lam K, Chow E, Zhang L, Wong E, Bedard G, Fairchild A, Vassiliou V, Alm el-Din M, Jesus-Garcia R, Kumar A, Forges F, Tseng LM, Hou MF, Chie WC, Bottomley A (2013) Determinants of quality of life in advanced cancer patients with bone metastases undergoing palliative radiation treatment. Support Care Cancer 21:3021–3030
The World Bank (2018) World Health Organization Global Health Expenditure database. The World Bank URL: https://apps.who.int/nha/database/country_profile/Index/en. Accessed 8 December 2019
Hsiao WC (1995) Medical savings accounts: lessons from Singapore. Health Aff 14:260–266
Massaro TA, Wong Y-N (1995) Positive experience with medical savings accounts in Singapore. Health Aff 14:267–272
Barr MD (2001) Medical savings accounts in Singapore: a critical inquiry. J Health Polit Policy Law 26:709–726
Lim M-K (2004) Shifting the burden of health care finance: a case study of public–private partnership in Singapore. Health Policy 69:83–92
Ministry of Social and Family Development (2017) ComCare Long Term Assistance URL: https://www.msf.gov.sg/Comcare/Pages/Public-Assistance.aspx. Accessed 8 December 2019
Sahadevan S, Lim PPJ, Tan NJ, Chan SP (2000) Diagnostic performance of two mental status tests in the older Chinese: influence of education and age on cut-off values. Int J Geriatric Psychiatry 15:234–241
Gerard T (2012) Eastern Cooperative Oncology Group performance status. Chemotherapy. 5:10
Teo I, Singh R, Malhotra C et al (2018) Cost of Medical Care of Patients with Advanced Serious Illness in Singapore (COMPASS): prospective cohort study protocol. BMC Cancer 18:459
George LK, Fillenbaum GG (1985) OARS methodology. J Am Geriatr Soc 33:607–615
Cella DF, Tulsky DS, Gray G et al (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 11:570–579
Kemmler G, Holzner B, Kopp M et al (1999) Comparison of two quality-of-life instruments for cancer patients: the functional assessment of cancer therapy-general and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-C30. J Clin Oncol 17:2932–2940
Luckett T, King MT, Butow PN, Oguchi M, Rankin N, Price MA, Hackl NA, Heading G (2011) Choosing between the EORTC QLQ-C30 and FACT-G for measuring health-related quality of life in cancer clinical research: issues, evidence and recommendations. Ann Oncol 22:2179–2190
Victorson D, Barocas J, Song J, Cella D (2008) Reliability across studies from the functional assessment of cancer therapy-general (FACT-G) and its subscales: a reliability generalization. Qual Life Res 17:1137–1146
Gao F, Ng G-Y, Cheung Y-B, Thumboo J, Pang G, Koo WH, Sethi VK, Wee J, Goh C (2009) The Singaporean English and Chinese versions of the EQ-5D achieved measurement equivalence in cancer patients. J Clin Epidemiol 62:206–213
Cleeland C, Ryan K (1994) Pain assessment: global use of the Brief Pain Inventory. Annals Academy of Medicine, Singapore
Lyons KD, Bakitas M, Hegel MT, Hanscom B, Hull J, Ahles TA (2009) Reliability and validity of the Functional Assessment of Chronic Illness Therapy-Palliative care (FACIT-Pal) scale. J Pain Symptom Manag 37:23–32
Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res 52:69–77
Carroll BT, Kathol RG, Noyes R Jr, Wald TG, Clamon GH (1993) Screening for depression and anxiety in cancer patients using the Hospital Anxiety and Depression Scale. Gen Hosp Psychiatry 15:69–74
Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D (2002) Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 24:49–58
Ayanian JZ, Zaslavsky AM, Arora NK et al (2010) Patients’ experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol 28:4154
The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 9th edition. 2016
Singapore Department of Statistics (2017) Population trends 2017:15 URL: https://www.singstat.gov.sg/-/media/files/publications/population/population2017.pdf. Accessed 8 December 2019
Fenn KM, Evans SB, McCorkle R, DiGiovanna MP, Pusztai L, Sanft T, Hofstatter EW, Killelea BK, Knobf T, Lannin DR, Abu-Khalaf M, Horowitz NR, Chagpar AB (2014) Impact of financial burden of cancer on survivors’ quality of life. J Oncol Pract 10:332–338
Meneses K, Azuero A, Hassey L, McNees P, Pisu M (2012) Does economic burden influence quality of life in breast cancer survivors? Gynecol Oncol 124:437–443
Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D (2015) Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pract 11:145–150
Kale HP, Carroll NV (2016) Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer. 122:283–289
Sharp L, Carsin AE, Timmons A (2013) Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology. 22:745–755
Meeker CR, Geynisman DM, Egleston BL et al (2016) Relationships among financial distress, emotional distress, and overall distress in insured patients with cancer. J Oncol Pract 12:e755–e764
Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D (2016) Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol 34:1732–1740
Nekolaichuk CL, Jevne RF, Maguire TO (1999) Structuring the meaning of hope in health and illness. Soc Sci Med 48:591–605
McClement SE, Chochinov HM (2008) Hope in advanced cancer patients. Eur J Cancer 44:1169–1174
Benzein E, Norberg A, Saveman BI (2001) The meaning of the lived experience of hope in patients with cancer in palliative home care. Palliat Med 15:117–126
McClain CS, Rosenfeld B, Breitbart W (2003) Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. Lancet. 361:1603–1607
Organisation WH (2018) Constitution of WHO: principles
Owusu-Addo E, Cross R (2014) The impact of conditional cash transfers on child health in low- and middle-income countries: a systematic review. Int J Public Health 59:609–618 https://www.who.int/about/who-we-are/constitution
Lagarde M, Haines A, Palmer N (2007) Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA. 298:1900–1910
Acknowledgements
We thank Ratna Singh for the excellent project management for this study and Jing Rong for the research assistance provided on this paper. COMPASS Study team: Dent RA, Kumarakulasinghe NB, Malhotra R, Cheung YB, Nadkarni N, Yee ACP, Yang GM, Chan N, Yeo WL.
Authorship
CM and RH conceptualized the study and led the writing for the manuscript. All authors participated in interpretation of data analysis, and revising and editing the manuscript for submission.
Funding
This work was supported by Singapore Millennium Foundation and Lien Centre for Palliative Care (LCPC-IN14-0003).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethics and consent
The study was approved by SingHealth Centralised Institutional Review Board (ref no: 2015/2781).
Additional information
What is already known about the topic?
•Goals for Universal Health Coverage aim to reduce inequities in total pain and suffering among patients at end of life.
•A holistic patient-centred approach to understanding these inequities is currently lacking.
What this paper adds?
•We comprehensively assessed inequities in total pain and suffering outcomes comprising of physical, psychological, social, and spiritual outcomes and perceived health care quality.
•We demonstrate that advanced cancer patients with financial difficulties are worse in all total pain and suffering outcomes.
Implications for practice, theory, or policy
•Direct assessment of financial difficulties among patients with advanced cancer should be done to identify patients at-risk of greater total pain and suffering.
•To achieve Universal Health Coverage goals, a patient-centred approach focusing on reducing inequities in all total pain and suffering outcomes is required.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Malhotra, C., Harding, R., Teo, I. et al. Financial difficulties are associated with greater total pain and suffering among patients with advanced cancer: results from the COMPASS study. Support Care Cancer 28, 3781–3789 (2020). https://doi.org/10.1007/s00520-019-05208-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05208-y