Abstract
Purpose
It is well established that posterior spinal surgery results in damage to the paraspinal musculature. The effects of such iatrogenic changes on spinal loading have not been previously investigated, particularly at levels adjacent to a spinal fusion. Therefore, the objective of this study was to investigate the effect of simulated muscle damage on post-operative spinal loading at the adjacent levels to a spinal fusion during upright postures using a mathematical model.
Methods
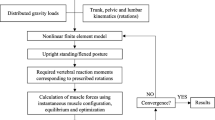
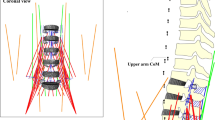
A musculoskeletal model of the spine using ArtiSynth with 210 muscle fascicles was used to predict spinal loading in an upright posture. The loading at L1–L2 and L5–S1 were estimated before and after simulated paraspinal muscle damage (i.e., removal of muscle attachments at L2–L5) along the lumbar spine, both with a spinal fusion at L2–L5 and without a spinal fusion.
Results
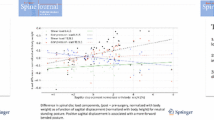
The axial compressive forces at the adjacent levels increased after simulated muscle damage, with the largest changes being at the rostral level (78 % increase in presence of spinal fusion; 73 % increase without spinal fusion) compared to the caudal level (41 % in presence of fusion and 32 % without fusion). Shear forces increased in a similar manner at both the rostral and caudal levels. These changes in loading were due to a redistribution of muscle activity from the local lumbar to the global spinal musculature.
Conclusions
The results suggest that the paraspinal muscles of the lumbar spine play an important role in adjacent segment loading of a spinal fusion, independent of the presence of rigid spinal instrumentation.









Similar content being viewed by others
References
Park P, Garton HJ, Gala VC et al (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944
Wai EK, Santos ERG, Morcom RA, Fraser RD (2006) Magnetic resonance imaging 20 years after anterior lumbar interbody fusion. Spine (Phila Pa 1976) 31:1952–1956
Axelsson P, Johnsson R, Strömqvist B (2007) Adjacent segment hypermobility after lumbar spine fusion after surgery. Acta Orthop 78:834–839. doi:10.1080/17453670710014635
Seitsalo S, Schlenzka D (1997) Disc degeneration in young patients with isthmic spondylolisthesis treated operatively or conservatively: a long-term follow-up. Eur Spine J 6:393–397
Korovessis P, Repantis T, Zacharatos S, Zafiropoulos A (2009) Does Wallis implant reduce adjacent segment degeneration above lumbosacral instrumented fusion? Eur Spine J 18:830–840. doi:10.1007/s00586-009-0976-y
Kaito T, Hosono N, Mukai Y et al (2010) Induction of early degeneration of the adjacent segment after posterior lumbar interbody fusion by excessive distraction of lumbar disc space. J Neurosurg Spine 12:671–679. doi:10.3171/2009.12.SPINE08823
Mannion AF, Leivseth G, Brox J-I, et al. (2014) Long-term follow up suggests spinal fusion is associated with increased adjacent segment disc degeneration but without influence on clinical outcome: results of a combined follow-up from 4 RCTs. Spine (Phila. Pa. 1976) 39:1373–83. doi:10.1097/BRS.0000000000000437
Lotz JC, Chin JR (2000) Intervertebral disc cell death is dependent on the magnitude and duration of spinal loading. Spine (Phila Pa 1976) 25:1477–1483
Stokes IAF, Iatridis JC (2004) Mechanical conditions that accelerate intervertebral disc degeneration: overload versus immobilization. Spine (Phila Pa 1976) 29:2724–2732
Walter BA, Korecki CL, Purmessur D et al (2011) Complex loading affects intervertebral disc mechanics and biology. Osteoarthr Cartil 19:1011–1018
Chan SCW, Ferguson SJ, Gantenbein-Ritter B (2011) The effects of dynamic loading on the intervertebral disc. Eur Spine J 20:1796–1812
Kim J, Yang S-J, Kim H et al (2012) Effect of shear force on intervertebral disc (IVD) degeneration: an in vivo rat study. Ann Biomed Eng 40:1996–2004
Hodges PW, Richardson CA (1996) Inefficient muscular stabilization of the lumbar spine associated with low back pain: a motor control evaluation of transversus abdominis. Spine (Phila Pa 1976) 21:2640–2650
Cholewicki J, Silfies SP, Shah RA et al (2005) Delayed trunk muscle reflex responses increase the risk of low back injuries. Spine (Phila Pa 1976) 30:2614–2620
Lee AS, Cholewicki J, Reeves NP et al (2010) Comparison of trunk proprioception between patients with low back pain and healthy controls. Arch Phys Med Rehabil 91:1327–1331
Tsao H, Tucker KJ, Hodges PW (2011) Changes in excitability of corticomotor inputs to the trunk muscles during experimentally-induced acute low back pain. Neuroscience 181:127–133
Haig AJ, London Z, Sandella DE (2013) Symmetry of paraspinal muscle denervation in clinical lumbar spinal stenosis: support for a hypothesis of posterior primary ramus stretching? Muscle Nerve 48:198–203
Leinonen V, Määttä S, Taimela S et al (2003) Paraspinal muscle denervation, paradoxically good lumbar endurance, and an abnormal flexion–extension cycle in lumbar spinal stenosis. Spine (Phila Pa 1976) 28:324–331
Wang G, Karki SB, Xu S et al (2014) Quantitative MRI and X-ray analysis of disc degeneration and paraspinal muscle changes in degenerative spondylolisthesis. J Back Musculoskelet Rehabil. doi:10.3233/BMR-140515
Gejo R, Matsui H, Kawaguchi Y et al (1999) Serial changes in trunk muscle performance after posterior lumbar surgery. Spine (Phila Pa 1976) 24:1023–1028
Kawaguchi Y, Matsui H, Gejo R, Tsuji H (1998) Preventive measures of back muscle injury after posterior lumbar spine surgery in rats. Spine (Phila Pa 1976) 23:2282–2287
Kawaguchi Y, Matsui H, Tsuji H (1996) Back muscle injury after posterior lumbar spine surgery: a histologic and enzymatic analysis. Spine (Phila Pa 1976) 21:941–944
Cawley DT, Alexander M, Morris S (2014) Multifidus innervation and muscle assessment post-spinal surgery. Eur Spine J 23:320–327
Keller A, Gunderson R, Reikerås O, Brox JI (2003) Reliability of computed tomography measurements of paraspinal muscle cross-sectional area and density in patients with chronic low back pain. Spine (Phila Pa 1976) 28:1455–1460. doi:10.1097/01.BRS.0000067094.55003.AD
Keller A, Brox JI, Gunderson R et al (2003) Trunk muscle strength, cross-sectional area, and density in patients with chronic low back pain randomized to lumbar fusion or cognitive intervention and exercises. Spine (Phila Pa 1976) 29:3–8
Wang H-L, Lu F-Z, Jiang J-Y et al (2011) Minimally invasive lumbar interbody fusion via MAST Quadrant retractor versus open surgery: a prospective randomized clinical trial. Chin Med J-Beijing 124:3868
Kramer M, Katzmaier P, Eisele R et al (2001) Surface electromyography-verified muscular damage associated with the open dorsal approach to the lumbar spine. Eur Spine J 10:414–420
Kim D-Y, Lee S-H, Chung SK, Lee H-Y (2004) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976) 30:123–129
Mayer TG, Vanharanta H, Gatchel RJ et al (1989) Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine (Phila Pa 1976) 14:33–36
Panjabi MM (2007) Hybrid multidirectional test method to evaluate spinal adjacent-level effects. Clin Biomech (Bristol, Avon) 22:257–265. doi:10.1016/j.clinbiomech.2006.08.006
Malakoutian M, Volkheimer D, Street J et al (2015) Do in vivo kinematic studies provide insight into adjacent segment degeneration?—a qualitative systematic literature review. Eur Spine J 24:1865–1881
Anderst WJ, Donaldson WF, Lee JY, Kang JD (2013) Cervical spine intervertebral kinematics with respect to the head are different during flexion and extension motions. J Biomech 46:1471–1475
Volkheimer D, Malakoutian M, Oxland TR, Wilke H-J (2015) Limitations of current in vitro test protocols for investigation of instrumented adjacent segment biomechanics: critical analysis of the literature. Eur J Spine 24:1882–1892
Weinhoffer SL, Guyer RD, Herbert M, Griffith SL (1995) Intradiscal pressure measurements above an instrumented fusion: a cadaveric study. Spine (Phila Pa 1976) 20:526–531
Chow DHK, Luk KDK, Evans JH, Leong JCY (1996) Effects of short anterior lumbar interbody fusion on biomechanics of neighboring unfused segments. Spine (Phila Pa 1976) 21:549–555
Cunningham BW, Kotani Y, McNulty PS et al (1997) The effect of spinal destabilization and instrumentation on lumbar intradiscal pressure: an in vitro biomechanical analysis. Spine (Phila Pa 1976) 22:2655–2663
Pfeiffer M, Hoffman H, Goel VK et al (1997) In vitro testing of a new transpedicular stabilization technique. Eur Spine J 6:249–255
Bastian L, Lange U, Knop C et al (2001) Evaluation of the mobility of adjacent segments after posterior thoracolumbar fixation: a biomechanical study. Eur Spine J 10:295–300
Schmoelz W, Huber JF, Nydegger T et al (2003) Dynamic stabilization of the lumbar spine and its effects on adjacent segments: an in vitro experiment. J Spinal Disord Tech 16:418–423
Moore J, Yoganandan N, Pintar FA et al (2006) Tapered cages in anterior lumbar interbody fusion: biomechanics of segmental reactions. J Neurosurg Spine 5:330–335
Schmoelz W, Huber JF, Nydegger T et al (2006) Influence of a dynamic stabilisation system on load bearing of a bridged disc: an in vitro study of intradiscal pressure. Eur Spine J 15:1276–1285
McGill SM, Norman RW (1986) Partitioning of the L4–L5 dynamic moment into disc, ligamentous, and muscular components during lifting. Spine (Phila Pa 1976) 11:666–678
Stokes IAF, Gardner-Morse M (1995) Lumbar spine maximum efforts and muscle recruitment patterns predicted by a model with multijoint muscles and joints with stiffness. J Biomech 28:173–186
Arjmand N, Shirazi-Adl A (2006) Model and in vivo studies on human trunk load partitioning and stability in isometric forward flexions. J Biomech 39:510–521. doi:10.1016/j.jbiomech.2004.11.030
de Zee M, Hansen L, Wong C et al (2007) A generic detailed rigid-body lumbar spine model. J Biomech 40:1219–1227. doi:10.1016/j.jbiomech.2006.05.030
Christophy M, Faruk Senan NA, Lotz JC, O’Reilly OM (2012) A musculoskeletal model for the lumbar spine. Biomech Model Mechanobiol 11:19–34. doi:10.1007/s10237-011-0290-6
Han K-S, Zander T, Taylor WR, Rohlmann A (2012) An enhanced and validated generic thoraco-lumbar spine model for prediction of muscle forces. Med Eng Phys 34:709–716. doi:10.1016/j.medengphy.2011.09.014
Bresnahan L, Fessler RG, Natarajan RN (2010) Evaluation of change in muscle activity as a result of posterior lumbar spine surgery using a dynamic modeling system. Spine (Phila Pa 1976) 35:E761–E767. doi:10.1097/BRS.0b013e3181e45a6e
Malakoutian M, Street J, Wilke H-J et al (2015) A musculoskeletal model of the lumbar spine using ArtiSynth—development and validation. Comput Methods Biomech Biomed Eng Imag Vis 1–8. doi:10.1080/21681163.2016.1187087
Lloyd JE, Stavness I, Fels S (2012) ArtiSynth: A fast interactive biomechanical modeling toolkit combining multibody and finite element simulation. In: Soft Tissue Biomechanical Modeling for Computer Assisted Surgery. Springer, pp 355–394. doi:10.1007/8415_2012_126
Stavness I, Lloyd JE, Payan Y, Fels S (2011) Coupled hard–soft tissue simulation with contact and constraints applied to jaw–tongue–hyoid dynamics. Int J Numer Method Biomed Eng 27:367–390
Stavness I, Lloyd JE, Fels S (2012) Automatic prediction of tongue muscle activations using a finite element model. J Biomech 45:2841–2848
Dao TT, Pouletaut P, Charleux F Lazáry Á, Eltes P, Varga PP, Tho MC (2014) Estimation of patient specific lumbar spine muscle forces using multi-physical musculoskeletal model and dynamic MRI. In: Huynh VN, Denoeux T, Tran DH, Le AC, Pham SB (eds) Knowledge and Systems Engineering vol. 2, Advances in Intelligent Systems and Computing. Springer International Publishing, Cham, pp 411–422. doi:10.1007/978-3-319-02821-7_36
Panjabi MM, Brand RA Jr, White AA III (1976) Three-dimensional flexibility and stiffness properties of the human thoracic spine. J Biomech 9:185–192
Heuer F, Schmidt H, Klezl Z et al (2007) Stepwise reduction of functional spinal structures increase range of motion and change lordosis angle. J Biomech 40:271–280
Gardner-Morse MG, Stokes IA (2004) Structural behavior of human lumbar spinal motion segments. J Biomech 37:205–212. doi:10.1016/j.jbiomech.2003.10.003
Millard M, Uchida T, Seth A, Delp SL (2013) Flexing computational muscle: modeling and simulation of musculotendon dynamics. J Biomech Eng 135:21005
Cobb WS, Burns JM, Kercher KW et al (2005) Normal intraabdominal pressure in healthy adults. J Surg Res 129:231–235
Stavness IK (2010) Byte your tongue. PhD dissertation, University of British Columbia
Wilke H-J, Neef P, Hinz B et al (2001) Intradiscal pressure together with anthropometric data—a data set for the validation of models. Clin Biomech 16:S111–S126
Poh S-Y, Yue W-M, Chen JL-T et al (2011) Two-year outcomes of transforaminal lumbar interbody fusion. J Orthop Surg 19:135–140
Min J-H, Jang J-S, Lee S-H (2007) Comparison of anterior-and posterior-approach instrumented lumbar interbody fusion for spondylolisthesis. J Neurosurg Spine 7(1):21–26
Chou W-Y, Hsu C-J, Chang W-N, Wong C-Y (2002) Adjacent segment degeneration after lumbar spinal posterolateral fusion with instrumentation in elderly patients. Arch Orthop Trauma Surg 122:39–43
Yee TJ, Terman SW, La Marca F, Park P (2014) Comparison of adjacent segment disease after minimally invasive or open transforaminal lumbar interbody fusion. J Clin Neurosci Off J Neurosurg Soc Australas 21(10):1796–1801
Kim H-J, Moon S-H, Chun H-J et al (2009) Comparison of mechanical motion profiles following instrumented fusion and non-instrumented fusion at the L4–5 segment. Clin Invest Med 32:E64–E69
Acknowledgments
The authors gratefully acknowledge financial support from the Natural Sciences and Engineering Research Council of Canada (NSERC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Malakoutian, M., Street, J., Wilke, HJ. et al. Role of muscle damage on loading at the level adjacent to a lumbar spine fusion: a biomechanical analysis. Eur Spine J 25, 2929–2937 (2016). https://doi.org/10.1007/s00586-016-4686-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4686-y