Abstract
Purpose
Lateral mass mini-screws used in plated cervical laminoplasty might penetrate into facet joints. The objective is to observe this complication incidence and to identify the optimal areas for 5- and 7-mm-long mini-screws to implant on lateral mass.
Methods
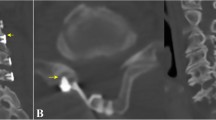
47 patients who underwent plated cervical laminoplasty were included. The optimal area for mini-screws implanting was set according to pre-operative 3D CT reconstruction data. Then, each posterior–lateral mass surface was divided into three regions: 7-mm region, 5-mm region, and dangerous area. The mini-screw implanted region was recorded. Post-operative CT images were used to identify whether the mini-screws penetrated into facet joints.
Results
235 mini-plates and 470 lateral mass mini-screws were used in the study. 117 (24.9%) mini-screws penetrated 88 (37.4%) facet joints. The 5-mm-long mini-screw optimal area occupied the upper 72, 65, 65, 64, and 65 % area of the posterior–lateral mass surface for C3–7, while the 7-mm-long mini-screw optimal area encompassed the upper 54, 39, 40, 33, and 32 %. Only 7-mm-long mini-screws were used to fix the plate to the lateral mass. 4 of 240 mini-screws in 7-mm region, 67 of the 179 mini-screws in 5-mm region, and 46 of the 51 mini-screws in dangerous region penetrated into the facet joint. The differences in the rate of facet joint penetration related to region were statistically significant (P < 0.001).
Conclusions
The facet joint destruction by mini-screws was not a rare complication in plated cervical laminoplasty. The optimal areas we proposed may help guide the mini-screw implantation positions.






Similar content being viewed by others
References
Luk KD, Kamath V, Avadhani A, Rajasekaran S (2010) Cervical laminoplasty. Eur Spine J 19:347–348
Mitsunaga LK, Klineberg EO, Gupta MC (2012) Laminoplasty techniques for the treatment of multilevel cervical stenosis. Adv Orthop 2012:307916
Hale JJ, Gruson KI, Spivak JM (2006) Laminoplasty: a review of its role in compressive cervical myelopathy. Spine J 6:S289–S298
Chen H, Deng Y, Li T, Gong Q, Song Y, Liu H (2015) Clinical and radiography results of mini-plate fixation compared to suture suspensory fixation in cervical laminoplasty: a five-year follow-up study. Clin Neurol Neurosurg 138:188–195
Park AE, Heller JG (2004) Cervical laminoplasty: use of a novel titanium plate to maintain canal expansion–Surgical technique. J Spinal Disord Tech 17:265–271
Rhee JM, Register B, Hamasaki T, Franklin B (2011) Plate-only open door laminoplasty maintains stable spinal canal expansion with high rates of hinge union and no plate failures. Spine 36:9–14
Wang SJ, Jiang SD, Jiang LS, Dai LY (2011) Axial pain after posterior cervical spine surgery: a systematic review. Eur Spine J 20:185–194
Riew KD, Raich AL, Dettori JR, Heller JG (2013) Neck pain following cervical laminoplasty: does Preservation of the C2 Muscle Attachments and/or C7 Matter? Evid Based Spine Care J 4:42–53
Cho CB, Chough CK, Oh JY, Park HK, Lee KJ, Rha HK (2010) Axial neck pain after cervical laminoplasty. J Korean Neurosurg Soc 47:107–111
Watanabe K, Katsumi K, Yamazaki A, Ohashi M (2010) Features of axial neck pain after open-door laminoplasty for cervical myelopathy. Spine J 10:80S–81S
Chen H, Liu H, Deng Y, Gong Q, Li T, Song Y (2016) Multivariate analysis of factors associated with axial symptoms in unilateral expansive open-door cervical laminoplasty with miniplate fixation. Medicine (Baltimore) 95:e2292
Manchikanti L, Cash KA, Pampati V, Malla Y (2014) Two-year follow-up results of fluoroscopic cervical epidural injections in chronic axial or discogenic neck pain: a randomized, double-blind, controlled trial. Int J Med Sci 11:309–320
Yoshida M, Tamaki T, Kawakami M, Nakatani N, Ando M, Yamada H, Hayashi N (2002) Does reconstruction of posterior ligamentous complex with extensor musculature decrease axial symptoms after cervical laminoplasty? Spine 27:1414–1418
Chen G, Luo Z, Nalajala B, Liu T, Yang H (2012) Expansive open-door laminoplasty with titanium miniplate versus sutures. Orthopedics 35:e543–e548
Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K (2001) Interobserver and intraobserver reliability of the Japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine 26:1890–1894
Suk KS, Kim KT, Lee JH, Lee SH, Kim JS, Kim JY (2009) Reevaluation of the Pavlov ratio in patients with cervical myelopathy. Clin Orthop Surg 1:6–10
Takeuchi K, Yokoyama T, Ono A, Numasawa T, Wada K, Kumagai G, Ito J, Ueyama K, Toh S (2007) Cervical range of motion and alignment after laminoplasty preserving or reattaching the semispinalis cervicis inserted into axis. J Spinal Disord Tech 20:571–576
Bogduk N, Marsland A (1988) The cervical zygapophysial joints as a source of neck pain. Spine 13:610–617
Bykowski JL, Wong WH (2012) Role of facet joints in spine pain and image-guided treatment: a review. AJNR Am J Neuroradiol 33:1419–1426
Sakaura H, Hosono N, Mukai Y, Fujii R, Iwasaki M, Yoshikawa H (2007) Persistent local pain after posterior spine surgery for thoracic lesions. J Spinal Disord Tech 20:226–228
Yeh KT, Yu TC, Chen IH, Peng CH, Liu KL, Lee RP, Wu WT (2014) Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosis. J Orthop Surg Res 9:49
Tofuku K, Koga H, Komiya S (2012) Cervical pedicle screw insertion using a gutter entry point at the transitional area between the lateral mass and lamina. Eur Spine J 21:353–358
Hockel K, Maier G, Rathgeb J, Sirichativapee W, Wisanuyotin T, Kosuwon W, Jeeravipoolvarn P (2014) Morphometric subaxial lateral mass evaluation allows for preoperative optimal screw trajectory planning. Eur Spine J 23:1705–1711
Hu Y, Dong WX, Spiker WR, Yuan ZS, Sun XY, Zhang J, Xie H, Albert TJ (2015) Optimal entry point and trajectory for anterior C1 lateral mass screw. J Spinal Disord Tech. doi:10.1097/BSD.0000000000000280 [epub ahead of print]
Lin JM, Hipp JA, Reitman CA (2013) C1 lateral mass screw placement via the posterior arch: a technique comparison and anatomic analysis. Spine J 13:1549–1555
Schmeiser G, Schilling C, Grupp TM, Papavero L, Püschel K, Kothe R (2015) Unilateral laminoplasty with lateral mass screw fixation for less invasive decompression of the cervical spine: a biomechanical investigation. Eur Spine J 24:2781–2787
Lee SE, Jahng TA, Kim HJ (2016) En bloc cervical laminoplasty using translaminar screws (T-laminoplasty): novel procedure for preserving midline ligamentous structures. Clin Spine Surg 29:E296–E302
Coe JD, Vaccaro AR, Dailey AT, Skolasky RL Jr, Sasso RC, Ludwig SC, Brodt ED, Dettori JR (2013) Lateral mass screw fixation in the cervical spine: a systematic literature review. J Bone Joint Surg Am 95:2136–2143
Fujimori T, Le H, Ziewacz JE, Chou D, Mummaneni PV (2013) Is there a difference in range of motion, neck pain, and outcomes in patients with ossification of posterior longitudinal ligament versus those with cervical spondylosis, treated with plated laminoplasty? Neurosurg Focus 35:E9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest concerning the materials or methods used in this study or the findings specified in this study.
Rights and permissions
About this article
Cite this article
Chen, H., Li, H., Deng, Y. et al. Optimal area of lateral mass mini-screws implanted in plated cervical laminoplasty: a radiography anatomy study. Eur Spine J 26, 1140–1148 (2017). https://doi.org/10.1007/s00586-016-4785-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4785-9