Abstract
Purpose
Recently, strategies aimed at optimizing provider factors have been proposed, including regionalization of surgeries to higher volume centers and adoption of volume standards. With limited literature promoting the regionalization of spine surgeries, we undertook a systematic review to investigate the impact of surgeon volume on outcomes in patients undergoing spine surgery.
Methods
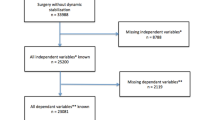
We performed a systematic review examining the association between surgeon volume and spine surgery outcomes. To be included in the review, the study population had to include patients undergoing a primary or revision spinal procedure. These included anterior cervical discectomy and fusion (ACDF), anterior/posterior cervical fusion, laminectomy/decompression, anterior/posterior lumbar decompression with fusion, discectomy, and spinal deformity surgery (spine arthrodesis).
Results
Studies were variable in defining surgeon volume thresholds. Higher surgeon volume was associated with a significantly lower risk of postoperative complications, a lower length of stay (LOS), lower cost of hospital stay and a lower risk of readmissions and reoperations/revisions.
Conclusions
Findings suggest a trend towards better outcomes for higher volume surgeons; however, further study needs to be carried out to define objective volume thresholds for individual spine surgeries for surgeons to use as a marker of proficiency.

Similar content being viewed by others
References
Friedly J, Standaert C, Chan L (2010) Epidemiology of spine care: the back pain dilemma. Phys Med Rehabil Clin N Am 21(4):659–677
Dagenais S, Caro J, Haldeman S (2008) A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 8(1):8–20
Deyo RA, Weinstein JN (2001) Low back pain. N Engl J Med 344(5):363–370
Allegri M et al (2016) Mechanisms of low back pain: a guide for diagnosis and therapy. F1000Res 5. https://doi.org/10.12688/f1000research.8105.2
Martin BI et al (2008) Expenditures and health status among adults with back and neck problems. JAMA 299(6):656–664
Weiner DK et al (2006) Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med 7(2):143–150
Deyo RA et al (2005) United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 30(12):1441–1445 (discussion 1446–7)
Oglesby M et al (2012) Epidemiological trends in cervical spine surgery for degenerative diseases between 2002 and 2009. Spine (Phila Pa 1976) 38(14):1226–1232
Mehta A et al (2017) Effect of surgeon and hospital volume on emergency general surgery outcomes. J Am Coll Surg 225(5):666–675
Wang HH et al (2015) Hospital surgical volume and associated postoperative complications of pediatric urological surgery in the United States. J Urol 194(2):506–511
Almatar A et al (2016) Effect of radical prostatectomy surgeon volume on complication rates from a large population-based cohort. Can Urol Assoc J 10(1–2):45–49
Mowat A, Maher C, Ballard E (2016) Surgical outcomes for low-volume vs high-volume surgeons in gynecology surgery: a systematic review and meta-analysis. Am J Obstet Gynecol 215(1):21–33
Vree FE et al (2014) The impact of surgeon volume on perioperative outcomes in hysterectomy. JSLS 18(2):174–181
Weng SF et al (2014) Renal transplantation: relationship between hospital/surgeon volume and postoperative severe sepsis/graft-failure. A Nationwide Population-based study. Int J Med Sci 11(9):918–924
Lau RL et al (2012) The role of surgeon volume on patient outcome in total knee arthroplasty: a systematic review of the literature. BMC Musculoskelet Disord 13:250
Ames JB et al (2010) Does surgeon volume for total hip arthroplasty affect outcomes after hemiarthroplasty for femoral neck fracture? Am J Orthop (Belle Mead NJ) 39(8):E84–E89
Katz JN et al (2003) Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum 48(2):560–568
Moher D et al (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341
Atkins D et al (2004) Grading quality of evidence and strength of recommendations. BMJ 328(7454):1490
Farjoodi P, Skolasky RL, Riley LH (2011) The effects of hospital and surgeon volume on postoperative complications after lumbar spine surgery. Spine (Phila Pa 1976) 36(24):2069–2075
Dasenbrock HH et al (2012) The impact of provider volume on the outcomes after surgery for lumbar spinal stenosis. Neurosurgery 70(6):1346–1353 (discussion 1353–4)
Cole T et al (2017) Surgeon procedure volume and complication rates in anterior cervical discectomy and fusions: analysis of a national longitudinal database. Clin Spine Surg 30(5):E633–E639
Basques BA et al (2017) Effect of surgeon volume on complications, length of stay, and costs following anterior cervical fusion. Spine (Phila Pa 1976) 42(6):394–399
Paul JC, Lonner BS, Toombs CS (2015) Greater operative volume is associated with lower complication rates in adolescent spinal deformity surgery. Spine (Phila Pa 1976) 40(3):162–170
De la Garza Ramos R et al (2017) Volume-outcome relationship after 1 and 2 level anterior cervical discectomy and fusion. World Neurosurg 105:543–548
Blais MB et al (2017) Establishing objective volume-outcome measures for anterior and posterior cervical spine fusion. Clin Neurol Neurosurg 161:65–69
Bederman SS et al (2009) The who, what and when of surgery for the degenerative lumbar spine: a population-based study of surgeon factors, surgical procedures, recent trends and reoperation rates. Can J Surg 52(4):283–290
Paul JC et al (2015) Complication rates are reduced for revision adult spine deformity surgery among high-volume hospitals and surgeons. Spine J 15(9):1963–1972
Schoenfeld AJ et al (2017) Examining healthcare segregation among racial and ethnic minorities receiving spine surgical procedures in the state of Florida. Spine 42(24):1917–1922
Shervin N, Rubash HE, Katz JN (2007) Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res 457:35–41
Agency for Healthcare Research Quality (AHRQ) Agency for Healthcare Research Quality (AHRQ) HCUP Databases, Healthcare Cost and Utilization Project (HCUP): overview of the Nationwide Inpatient Sample (NIS) (2013). http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 01 Sep 2017
An introduction to statewide inpatient databases. https://www.hcup-us.ahrq.gov/db/state/siddist/SID_Introduction.jsp. Accessed 01 Sep 2017
Birkmeyer JD et al (2003) Surgeon volume and operative mortality in the United States. N Engl J Med 349(22):2117–2127
Luft HS, Hunt SS, Maerki SC (1987) The volume-outcome relationship: practice-makes-perfect or selective-referral patterns? Health Serv Res 22(2):157–182
Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137(6):511–520
Bozic KJ et al (2010) The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Jt Surg Am 92(16):2643–2652
Coffey RJ et al (1992) An introduction to critical paths. Qual Manag Health Care 1(1):45–54
Chung SB et al (2012) Implementation and outcomes of a critical pathway for lumbar laminectomy or microdiscectomy. J Korean Neurosurg Soc 51(6):338–342
Dimick J et al (2013) Black patients more likely than whites to undergo surgery at low-quality hospitals in segregated regions. Health Aff (Millwood) 32(6):1046–1053
Sclafani JA, Kim CW (2014) Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res 472(6):1711–1717
Nandyala SV et al (2014) Minimally invasive transforaminal lumbar interbody fusion: one surgeon’s learning curve. Spine J 14(8):1460–1465
Funding
No funding was required for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest was declared by the authors.
Rights and permissions
About this article
Cite this article
Malik, A.T., Panni, U.Y., Mirza, M.U. et al. The impact of surgeon volume on patient outcome in spine surgery: a systematic review. Eur Spine J 27, 530–542 (2018). https://doi.org/10.1007/s00586-017-5447-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5447-2