Abstract
Purpose
To review the anatomy and function of the sacroiliac joint (SIJ), as well as the pathophysiology, clinical presentation, diagnostic criteria, and treatment options for SIJ dysfunction.
Methods
The SIJ serves an extremely crucial function in mobility, stability, and resistance against shear forces. Joint mobility becomes increasingly limited with age-related cartilaginous changes that begin in puberty and continue throughout life. Pain can also be localized to the SIJ itself, known as SIJ dysfunction. A literature review was performed on the anatomy, etiology, risk factors, diagnostic modalities, and treatment options for SIJ dysfunction.
Results
SIJ dysfunction is an under-recognized source of low back pain. Dysfunction can result from various clinical conditions, as well as abnormal motion or malalignment of the joint. Diagnosis and evaluation of SIJ dysfunction are difficult, with use of physical maneuvers and image-guided anesthetic injection. Non-operative treatment options are considered first-line due to high surgical complication rates. Such options include conservative management, radiofrequency treatment, nerve blocks, and articular injections. Surgical management involves open and percutaneous approaches.
Conclusion
With the aging nature of the population, SIJ dysfunction has emerged as an extremely prevalent issue. Current research into the pathophysiology and risk factors of SIJ dysfunction is extremely important for planning preventative and therapeutic strategies. Various treatment options exist including conservative management, radiofrequency, nerve blocks, intra-articular or peri-articular injections, and surgical fixation. Improved diagnostic methods in clinical practice are thus critical to properly identify patients suffering from SIJ dysfunction, plan early intervention, and hasten return to function.
Level of Evidence I
Diagnostic: individual cross-sectional studies with the consistently applied reference standard and blinding.
Similar content being viewed by others
Background
SIJ: anatomy and function
The sacroiliac joints (SIJ) are the largest axial joints in the human body [1]. They are auricular-shaped, diarthrodial synovial joints located in the pelvis that link the iliac bones to the sacrum. The anterior one-third of the interface is a true synovial joint, while the posterior two-third is comprised of various ligamentous connections that stabilize the joint and limit range of motion. The ligamentous and muscular networks surrounding the SIJ are interrelated and contribute to joint mobility. Normal motion in the stabilized joint is minimal, around 2–4 mm of movement in all planes. Women have a weaker SIJ ligamentous complex. The SIJ undergoes the most mobility during pregnancy when sex hormones result in increased ligamentous laxity [1]. In contrast, decreased mobility is present in males and associated with aging.
SIJs undergo various changes with aging. In early adulthood, the joint surfaces are smooth and allow for multi-directional gliding motions. Age-related changes begin during puberty and continue throughout life. The SIJ is covered by two different cartilages. The concave sacral surface is covered with a thick hyaline articular cartilage that reaches 4 mm in thickness by adulthood. The convex iliac surface is lined by a thin fibrocartilage. Beginning in puberty, the iliac surfaces become rougher and coated in fibrous plaques. They reach a maximal thickness of 1–2 mm by adulthood [2]. Morphological changes restrict motion and accelerate during the third decade. Further changes resemble osteoarthritic degeneration and include surface irregularities, fissures, chondrocyte clustering, and fibrillation [1]. As the capsule becomes increasingly collagenous, extreme restriction of motion may occur by the sixth decade [3]. By the eighth decade, plaque formation and erosions are evident. Sacral surface changes also occur, but often remain 10–20 years after iliac surface changes.
Cartilage changes are present from embryonic life until the eighth decade. Such changes were originally misinterpreted as degenerative arthrosis, but were later shown to be adaptations to shear forces [4]. The SIJs are particularly vulnerable to shear loading due to their flat articular surfaces. Samples from normal SIJs demonstrate high-friction coefficients for both coarse texture and complementary ridges and grooves. Such features reflect adaptation to human bipedalism, contribute to joint stability and resistance against shear, and allow for less muscle and ligament force to support the upper trunk. Further stabilization and friction reduction occur through form closure and force closure. Form closure refers to interlocking of the ridges and grooves on the joint surface, minimizing the need for lateral forces [5, 6]. However, with close interlocking of the sacrum and pelvis, mobility would be virtually non-existent. Force closure refers to the compressive forces of the ligaments, muscles, and fascia. Muscle weakness and insufficient ligamentous tension would negatively influence load transfer [6]. The combination of force closure and form closure establishes SIJ stability.
SIJ dysfunction: pathophysiology
Pain localized to the SIJ region includes a broad differential, including pain from the lumbar spine, SIJ, and hip joint, as well as visceral pain. Pain and stiffness experienced from the SIJ is referred to as SIJ dysfunction. SIJ dysfunction typically results from abnormal motion and malalignment of the joint. Abnormal motion includes hyper or hypo-mobile SIJs. Increased production of estrogen and relaxin during pregnancy, along with the pressure of a growing fetus, may cause hypermobility of the SIJ [7]. In contrast, pelvic fractures and sedentary lifestyle can lead to hypo-mobility and joint fixation.
Abnormal mobility can result in malalignment of the joint, with subsequent SIJ dysfunction. As bipedal organisms, mankind is designed to stand erect. During normal standing posture, the line of gravity passes posterior to the center of the acetabula. The pelvis is forced to rotate downward posteriorly around the acetabula and a pelvic tilt is created automatically [8]. However, dysfunction can occur during abnormal lifting, bending forward, or lordotic posturing when the line of gravity is displaced relative to the center of the acetabula. Dysfunction will occur if the abdominal muscles cannot support the rotational and transfer of force [8].
SIJ dysfunction can result from various clinical conditions, including high-velocity trauma, degenerative arthritis, inflammatory arthropathy, infection, and moderate impact exercise. High-velocity trauma includes motor vehicle accidents and falls, resulting in pelvic ring injuries, occult fractures, or SIJ ligamentous strains. Inflammatory arthropathies should be considered in individuals presenting with systemic manifestations. Individuals without systemic manifestations often possess SIJ dysfunction from moderate exercise, such as lifting or jogging. Secondary conditions should also be considered, including prior spinal fixation, scoliosis, and leg length discrepancy [9]. Kiapour et al. demonstrate progressively increased stresses across the SIJ articular surfaces with increased leg length discrepancy [10]. Other causes of pain localized to the SIJ should be considered, including appendicitis, ovarian cysts or torsion, and pelvic inflammatory disease.
SIJ dysfunction: prevalence and risk factors
Low back pain (LBP) is an extremely common and disabling condition worldwide. Sembrano and Polly identify the relative frequencies of spine, SIJ, and hip joint as the primary pain generator in 289 of 368 (78.5%) patients with LBP. 65% had spine-only pathology, 14.5% had SIJ pathology, 12.5% of patients had hip pathology, and 10% had unidentified pain source after diagnostic workup [11]. Consequently, clinicians must be aware of non-spinal pain generators and pose alternative diagnoses for LBP.
With increasing prevalence up to 15–30%, primary LBP generation from SIJ dysfunction must be considered clinically. Both genders and all races are affected equally. SIJ dysfunction is a common cause of LBP in athletes, especially in sports with repetitive or asymmetric loading. Other risk factors include pregnancy, obesity, sedentary lifestyle, leg length discrepancy, hypermobility, direct trauma, systemic inflammatory conditions, and degenerative joint disease [12].
An emerging risk factor for the development of SIJ dysfunction is previous spinal fixation. Lumbar/lumbosacral fixation results in degenerative changes at the SIJ in 40–75% of patients after 5 years [13]. Such degenerative changes result from susceptibility to increased motion and stress at the articular surfaces following fixation. Nessim et al. demonstrates significantly lower pelvic tilt and L5 incidence among patients with degeneration of the SIJ following lumbosacral fixation. Lower pelvic tilt may be derived from weaker hamstring muscles, due to its anatomic proximity, predisposing to development of infra-adjacent segment degeneration and subsequent dysfunction [14]. DuPlissis et al. noted a minor correlation between SIJ dysfunction and decreased ipsilateral hamstring strength. No correlation was observed for hamstring length. Due to the low number of patients observed, further studies are needed to establish the role of hamstring musculature in SIJ stability and function [15]. Further studies are also necessary to establish the validity of fixation as a risk factor for the development of SIJ dysfunction, rather than SIJ dysfunction being treated as low back pain with spinal fixation.
Methods
A comprehensive literature review was performed on the clinical presentation, diagnostic modalities, and treatment options for SIJ dysfunction. The identification process of the articles collected is depicted in Fig. 1. Abstracts excluded included duplicate records, those with irrelevant titles, and those without full-text manuscripts. Full-text manuscripts were further assessed for relevance to the clinical presentation, diagnosis, and treatment options of SIJ dysfunction.
Results
SIJ dysfunction: clinical presentation
Identification of the primary pain generator in patients with LBP remains a significant challenge for spine surgeons. Compared with discogenic LBP, individuals with SIJ dysfunction often present with unilateral pain below L5. The pain is often localized distal and medial to the posterior superior iliac spine. It is described as sharp, dull, or shooting and is often misdiagnosed as radicular pain, as it can extend down the posterior thigh to the S1 dermatome [16]. If alterations in mobility or joint alignment are present, inappropriate stress loads on surrounding structures may result in widespread pain. Such structures include the low back, buttock, groin, posterolateral thigh, and abdomen [12, 13].
SIJ pain is typically worse while standing from a seated position, running, climbing, or lying on the ipsilateral side of the pain. In addition, most individuals report a specific inciting event. The most common SIJ injury results from sudden rotational and axial strain [12]. Most athletes will not present acutely following injury, but rather experience gradually progressive symptoms following repetitive microtrauma. As a result, they often complain of an aching LBP that prevents comfortable positioning. Insidious onset of pain that is worse at night and associated with weight loss and night sweats should be evaluated for malignant potential. Similarly, insidious onset of pain that improves with exercise, worse at night, and associated with morning stiffness should be evaluated for rheumatologic etiology. Symptoms associated with spinal levels above L5 should be evaluated for etiologies other than SIJ dysfunction.
SIJ dysfunction: diagnosis
SIJ dysfunction has traditionally been a clinical diagnosis utilizing physical exam findings. Due to its complex anatomy and broad pain differential, SIJ dysfunction clinical evaluation and diagnosis can be challenging. Presumptive diagnosis can be made through assessment of pain localization, patient posture and movement, and provocative manual testing. A comprehensive physical exam should be performed. Pain over the SIJs with direct palpation or tenderness at the sacral sulcus is often present. In contrast, neurologic and muscle strength testing should be normal. Complaints of bowel/bladder dysfunction with neurologic or muscle strength abnormalities should be evaluated in the emergency department for spinal cord pathology. Leg length should be measured, as discrepancies can contribute to the development of SIJ dysfunction. Similarly, dynamic examination including the Trendelenberg test and gait assessment should be performed to help identify the etiology [12].
Various provocation tests exist that may aid in the diagnosis of SIJ dysfunction, See Fig. 2. For most tests, the patient is placed in the supine position and a positive result occurs if the patient’s pain symptoms are reproduced or increased with the maneuver. Such tests include the FABER (flexion, abduction, and external rotation), Gaenslen’s, the distraction, the thigh thrust, and the compression tests. In the FABER, the patient’s leg is raised into flexion, abduction, and external rotation with stabilization of the contralateral anterior superior iliac spine with the opposite hand. In Gaenslen’s test, the affected leg and thigh hang over the edge of the table, while the contralateral hip is flexed. Pressure is applied to the hanging leg and flexed leg [12]. In the distraction test, the patient lies supine while the examiner applies a vertical posteriorly directed force to both anterior superior iliac spines. The test is presumed to “distract” the anterior aspect of the SIJ. In the thigh thrust test, the hip joint being tested is flexed to 90 degrees by the examiner. An anteroposterior force is applied to the SIJ through the femur. Finally, in the compression test, the patient is placed on their side while the examiner places their hands over the upper part of the iliac crest. The examiner places a downward force, causing forward pressure on the sacrum. No single provocation test has accurately identified SIJ dysfunction. However, there is evidence of good diagnostic validity utilizing at least three provocation tests. Broadhurst and Bond report a sensitivity of 77–87% for positive responses to three SIJ provocative maneuvers in identifying SIJ pain [17].
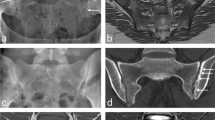
Laboratory testing provides no diagnostic benefit, unless acute sacroiliitis is considered. Acute sacroiliitis typically presents with acute SIJ pain and fever. If suspected, erythrocyte sedimentation rate and C-reactive protein should be ordered, along with joint aspiration for stain and culture. Magnetic resonance imaging (MRI) or computed tomography (CT) studies may be useful to rule out other causes of joint pain, including multiple myeloma, spinal stenosis, hip fracture, disk herniation, and trochanteric bursitis [9]. MRI is preferred if neurologic symptoms or radicular pain are present. MRI can detect edema and enhancement prior to bone changes evident on CT, as well as ligamentous and soft tissue injury. CT scans are more sensitive in identification of bone changes. CT scans may show evidence of SIJ degeneration, including presence of a gas shadow, erosions, osteophytes, joint space narrowing, and sclerosis. Radiographic imaging of the SIJ is often abnormal in asymptomatic patients older than 50 years of age. It is thus critical that imaging correlates with history and physical examination.
Another imaging modality that can be utilized in the diagnostic workup of lower back pain includes bone scintigraphy with single photon emission computed tomography (SPECT). Bone SPECT/CT combines a SPECT scan with a CT scan to identify and localize areas of abnormal metabolic activity. Active remodeling at the site of the defect is demonstrated by increased radiotracer uptake while CT images provide anatomical localization of the radiotracer [18]. Kato et al. utilized bone SPECT/CT to successfully identify the specific cause of LBP in five elderly patients and avoid inappropriate invasive spinal surgery [18]. In addition, bone SPECT/CT has been shown to be superior to MRI and CT in detecting spondylolysis [19].
Definitive evaluation of SIJ pathology is both diagnostic and therapeutic. It involves ultrasound-guided injection of steroid and anesthetic solutions into the joint. Image-guidance is crucial due to the complex anatomy of the SIJ and high likelihood of needle misplacement. The diagnosis is established if there is at least 75% acute symptom relief. However, relief may not occur if the pain is generated from the SIJ capsule or may be minimal in patients with a prior fixation. In addition, the individual response to two consecutive blocks is identical in only 60% of patients, as the anesthetic solution can diffuse out of the joint and come in contact with adjacent nerve sheaths [20]. The diagnostic yield of SIJ blocks is thus limited. Consequently, various authors advocate the use of image-guided injections only in patients presenting with at least three provocative maneuvers suggestive of SIJ dysfunction [21, 22].
SIJ dysfunction: treatment options
Initial treatment for SIJ dysfunction consists of conservative management, including physical therapy, chiropractic care, and medical therapy. NSAIDs are typically utilized for pain relief. Once pain relief is attained, return to ambulation utilizing assistive devices or physical therapy is crucial to prevent recurrence. If pelvic instability is noted, a sacroiliac belt may be temporarily utilized for support [9]. Posture should also be corrected and patients should be instructed on proper weight lifting. Patients must also be educated on lifestyle modifications, including healthy weight and exercise.
If conservative management fails to improve symptoms within 6 weeks, other treatment options include intra-articular injections, peri-articular injections, or nerve blocks. Radiofrequency treatment of the SIJ is also recommended [12]. Stelzer et al. demonstrate the benefit of cooled radiofrequency in the treatment of SIJ-mediated LBP at 4–6 months, 6–12 months, and > 12 months following treatment [23]. In contrast, Hensen et al. concluded that there was moderate evidence regarding the accuracy of SIJ injections and limited evidence regarding the therapeutic benefits of radiofrequency treatment [24]. The controlled anesthetic blocks consisted of 2% lidocaine injection, followed by 0.5% bupivacaine injection in patients with a positive response to lidocaine block. The initial lidocaine injection was utilized to screen for SIJ dysfunction, while the bupivacaine injection confirmed true SIJ dysfunction. A positive response was relief of pain [24].
When all therapeutic options fail to improve pain, surgical intervention may be considered. Open SIJ fixation (arthrodesis) has been performed since the 1920s. Several techniques for arthrodesis have been reported. Anterior arthrodesis has been shown to be effective in patients with severe SIJ pain refractory to conservative treatment [25]. The anterior approach avoids lateral cutaneous and ligamentous injury, while providing direct exposure of the ventral and cranial SIJ synovial components. Such exposure allows direct curettage and bone graft, with resultant good bone union. However, the incidence of complications associated with open SIJ fixation surgery is between 6 and 25% [26]. Consequently, the main surgical option is minimally invasive SIJ fixation.
Research has demonstrated positive minimally invasive lateral/transgluteal, posterior, and posterior-lateral SIJ fixation results in select patients, as compared to conservative management and radiofrequency treatment. (Fig. 3) Vanaclocha et al. demonstrate excellent long-term results assessed through pain scores and the Oswestry Disability Index, low opioid use, and improved work status in patients unresponsive to conservative management who underwent SIJ fixation. [27] In addition, Dengler et al. demonstrate LBP improvements 12 months following minimally invasive SIJ fixation in patients with chronic LBP originating from SIJ dysfunction. Polly et al. demonstrate improvements in pain, quality of life, and disability 24 months following minimally invasive SIJ fixation. Both studies utilized triangular titanium implants to achieve fixation. SIJ fixation with triangular titanium implants was safe and more effective than conservative management in pain relief, reduction of disability, and improvement in overall patient quality of life [28, 29]. A percutaneous procedure via a lateral approach has also been developed. The procedure utilizes hollow modular anchorage screws to achieve fixation without open-wound-related complications [30]. Spain and Holt report greater revision rates with screw fixation of the SIJ as compared to fixation with triangular titanium implants [31]. Furthermore, as SIJ hypermobility can be the source of pain generation, Dall et al. demonstrate significant reduction in SIJ range of motion utilizing fixation with six sacroiliac joint screws [32]. An alternative technique for pelvic fixation with comparable biomechanical properties to iliac screws includes the S2-alar-iliac (S2AI) screw fixation technique. S2AI screws can be placed percutaneously or by free-hand. Various advantages of utilizing S2AI screws include lower overall reoperation rates, longer time to reoperation, and decreased surgical site infections and wound dehiscence as compared to traditional iliac screw fixation [33, 34]. Furthermore, Cho and Bucklen demonstrate no statistical significance between right- and left-sided SIJ motion following unilateral SIJ 2- or 3-screw fixation. Treatment of unilateral SIJ dysfunction appears biomechanically equivalent to bilateral treatment in the immediate postoperative period. There is no evidence of contralateral hypermobility or instability [35]. Further long-term studies are needed to compare optimal treatments.
Conclusion
SIJ dysfunction is an under-recognized source of LBP worldwide. Dysfunction can result from various clinical conditions, as well as abnormal motion or malalignment of the joint. Various risk factors for development of SIJ dysfunction exist, including previous lumbar fixation surgery due to subsequent degenerative SIJ changes. The role of pelvic tilt and L5 incidence as risk factors for the development of SIJ dysfunction following lumbar fixation should be further investigated to help guide spine surgeons. As fixation can result in postoperative complications, other treatment options include conservative management, radiofrequency treatment, nerve blocks, and intra-articular or peri-articular injections. The open surgical approach is often reserved for refractory cases, due to 6–25% complication rate. Currently, percutaneous surgical techniques via a lateral approach are predominantly being used to avoid open-wound-related complications. Despite available treatment options, diagnosis and evaluation of SIJ dysfunction are difficult without image-guided anesthetic injection and physical maneuvers. A better understanding of the pathophysiology, risk factors, and associated clinical conditions will help guide diagnostic procedures and improve therapeutic outcomes.
References
Cohen SP (2005) Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg 101(5):1440–1453
Kampen W, Tillmann B (1998) Age-related changes in the articular cartilage of human sacroiliac joint. Anat Embryol 198:505–513
Bao H, Liabaud B, Varghese J et al (2016) Does pelvic incidence increase with age? An analysis of 1625 adults. Spine J 16:S356–S357
Bowen V, Cassidy JD (1981) Macroscopic and microscopic anatomy of the sacroiliac joint from embryonic life until the eighth decade. Spine (Phila Pa 1976) 6(6):620–628
Vleeming A, Schuenke MD, Masi AT et al (2012) The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat 221(6):537–567
Pool-Goudzwaard AL, Vleeming A, Stoeckart R et al (1998) Insufficient lumbopelvic stability: a clinical, anatomical and biomechanical approach to ‘a-specific’ low back pain. Man Ther 3(1):12–20
Capobianco R, Cher D, SIFI Study Group (2015) Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. Springerplus. 4:570
Dontigny RL (1979) Dysfunction of the sacroiliac joint and its treatment. J Orthop Sports Phys Ther 1(1):23–35
Raj MA, Ampat G, Varacallo M (2020) Sacroiliac Joint Pain. StatPearls Publishing
Kiapour A, Abdelgawad AA, Goel VK et al (2012) Relationship between limb length discrepancy and load distribution across the sacroiliac joint–a finite element study. J Orthop Res 30(10):1577–1580
Sembrano JN, Polly DW Jr (2009) How often is low back pain not coming from the back? Spine (Phila Pa 1976) 34(1):E27-32
Peebles R, Jonas CE (2017) Sacroiliac joint dysfunction in the athlete: diagnosis and management. Curr Sports Med Rep 16(5):336–342
Cohen SP, Chen Y, Neufeld NJ (2013) Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother 13(1):99–116
Nessim A, Cho W, Applebaum A et al (2019) Infradjacent segment disease after lumbar fusion: an analysis of pelvic parameters. E-POSTER 215: presented at 26th International Meeting on Advanced Spine Techniques 2019; Amsterdam
DuPlissis S, Hedden R, Manning N, et al (2016) The Effect of Hip and Hamstring Pathology on Sacroiliac Joint Dysfunction: A Case Series. Retrieved from Sophia, the St. Catherine University repository website: https://sophia.stkate.edu/dpt_papers/52
Buijs E, Visser L, Groen G (2007) Sciatica and the sacroiliac joint: a forgotten concept. BJA Br J Anaesth 99(5):713–716
Broadhurst NA, Bond MJ (1998) Pain provocation tests for the assessment of sacroiliac joint dysfunction. J Spinal Disord 11(4):341–345
Kato S, Demura S, Matsubara H et al (2019) Utility of bone SPECT/CT to identify the primary cause of pain in elderly patients with degenerative lumbar spine disease. J Orthop Surg Res 14(1):185. https://doi.org/10.1186/s13018-019-1236-4
Standaert CJ (2008) Low back pain in the adolescent athlete. Phys Med Rehabil Clin N Am 19(2):287–304. https://doi.org/10.1016/j.pmr.2008.01.002
Berthelot JM, Labat JJ, Le Goff B et al (2006) Provocative sacroiliac joint maneuvers and sacroiliac joint block are unreliable for diagnosing sacroiliac joint pain. Joint Bone Spine 73(1):17–23
Rashbaum RF, Ohnmeiss DD, Lindley EM et al (2016) Sacroiliac joint pain and its treatment. Clin Spine Surg 29(2):42–48
Thawrani DP, Agabegi SS, Asghar F (2019) Diagnosing sacroiliac joint pain. J Am Acad Orthop Surg 27(3):85–93
Stelzer W, Aiglesberger M, Stelzer D, Stelzer V (2013) Use of cooled radiofrequency lateral branch neurotomy for the treatment of sacroiliac joint-mediated low back pain: a large case series. Pain Med 14(1):29–35
Hansen HC, McKenzie-Brown AM, Cohen SP et al (2007) Sacroiliac joint interventions: a systematic review. Pain Phys 10(1):165–184
Murakami E, Kurosawa D, Aizawa T (2018) Sacroiliac joint arthrodesis for chronic sacroiliac joint pain: an anterior approach and clinical outcomes with a minimum 5-year follow up. J Neurosurg SPINE SPI 29(3):279–285
Yoshihara H (2012) Sacroiliac joint pain after lumbar/lumbosacral fusion: current knowledge. Eur Spine J 21(9):1788–1796
Vanaclocha V, Herrera JM, Sáiz-Sapena N et al (2018) Minimally invasive sacroiliac joint fusion, radiofrequency denervation, and conservative management for sacroiliac joint pain: 6-year comparative case series. Neurosurgery 82(1):48–55
Dengler JD, Kools D, Pflugmacher R et al (2017) 1-year results of a randomized controlled trial of conservative management vs. minimally invasive surgical treatment for sacroiliac joint pain. Physician. 20(6):537–550
Polly DW, Swofford J, Whang PG et al (2016) two-year outcomes from a randomized controlled trial of minimally invasive sacroiliac joint fusion vs non-surgical management for sacroiliac joint dysfunction. Int J Spine Surg. https://doi.org/10.14444/3028
Khurana A, Guha AR, Mohanty K, Ahuja S (2009) Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br 91(5):627–631
Spain K, Holt T (2017) Surgical revision after sacroiliac joint fixation or fusion. Int J Spine Surg 11(1):5
Dall BE, Eden SV, Cho W et al (2019) Biomechanical analysis of motion following sacroiliac joint fusion using lateral sacroiliac screws with or without lumbosacral instrumented fusion. Clin Biomech (Bristol, Avon) 68:182–189
Ishida W, Elder BD et al (2017) Comparison between S2-Alar-Iliac screw fixation and iliac screw fixation in adult deformity surgery: reoperation rates and spinopelvic parameters. Global Spine J 7(7):672–680
Wu AM, Chen D, Chen CH et al (2017) The technique of S2-alar-iliac screw fixation: a literature review. AME Med J 12(12):179
Cho W and Bucklen B (2017) An in vitro biomechanical analysis of contralateral sacroiliac joint motion following unilateral sacroiliac reconstruction. abstract presented at the annual NASS meeting; Orlando, Florida
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by AA, AN, and WC. The first draft of the manuscript was written by AA and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gartenberg, A., Nessim, A. & Cho, W. Sacroiliac joint dysfunction: pathophysiology, diagnosis, and treatment. Eur Spine J 30, 2936–2943 (2021). https://doi.org/10.1007/s00586-021-06927-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06927-9