Abstract
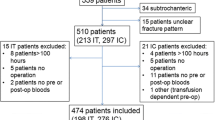
Significant blood loss in neck-of-femur (NOF) fracture surgery contributes to the high morbidity and mortality. Since the introduction of the European Working Time Directive, trainee surgeons are more junior and inexperienced. We assessed NOF surgical blood loss in relation to the surgeon grade and experience. We assessed a prospective consecutive cohort of 105 acute NOF fracture patients treated surgically. Blood loss was calculated as the difference between the pre- and post-operative haemoglobin levels. Warfarin was reversed pre-operatively where necessary. There were 32 male and 73 female patients, with mean age 83.8 years (range 48–98). One patient died peri-operatively and was excluded. There were 49 intra-capsular fractures and 55 extra-capsular fractures, with no significant difference in group characteristics. Mean haemoglobin drop was 2.8 g/dL [intra-capsular fractures, 2.5 g/dL; extra-capsular fractures, 3.1 g/dL (p = 0.019)]. The difference in blood loss between different surgeon grades was not significant: consultants 2.4 g/dL (21 cases), senior staff grades 2.7 g/dL (17 cases), junior staff grades 3.1 g/dL (15 cases) and registrars 2.9 g/dL (50 cases). Whilst mean haemoglobin drop was least for consultants, the mean for trainees was only marginally higher than for experienced staff grade surgeons and lower than for their junior counterparts. Mean blood loss for patients taking anti-platelet agents was not significantly different (aspirin 2.7 g/dL, clopidogrel 3.7 g/dL, 4.4 g/dL for those taking both) compared to patients taking neither agent (2.8 g/dL). We conclude that surgeon grade does not significantly impact peri-operative haemoglobin drop, regardless of pre-operative morbidity. It is safe for trainees to operate, with adequate supervision where appropriate, on all NOF fracture patients without compromising blood loss.








Similar content being viewed by others
References
Morritt DG, Morritt AN, Kelley SP, Stone MH (2005) Blood ordering protocol based on proposed surgical implant in fractured neck of femur patients. Ann R Coll Surg Engl 87(6):445–448
Foss NB, Kristensen MT, Kehlet H (2008) Anaemia impedes functional mobility after hip fracture surgery. Age Ageing 37(2):73–78
Kannus P, Parkkari J, Sievänen H, Heinonen A, Vuori I, Järvinen M (1996) Epidemiology of hip fractures. Bone 18(1 Suppl):57S–63S
Prasad N, Rajamani V, Hullin D, Murray JM (2009) Post-operative anaemia in femoral neck fracture patients: does it need treatment? A single blinded prospective randomised controlled trial. Injury 40(10):1073–1076
Dunne JR, Malone D, Tracy JK, Gannon C, Napolitano LM (2002) Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res 102(2):237–244
Su H, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ (2004) The relation between discharge hemoglobin and outcome after hip fracture. Am J Orthop 33(11):576–580
Kennedy MT, Roche S, Fleming SM, Lenehan B, Curtin W (2006) The association between aspirin and blood loss in hip fracture patients. Acta Orthop Belg 72(1):29–33
Jameson SS, Lamb A, Wallace WA, Sher JL, Marx C, Reed MR (2009) Orthopaedic training experience in the UK and Ireland: an analysis using the eLogbook. Surgeon 7(4):243–249
Bates T, Cecil E, Greene I (2007) The effect of the EWTD on training in general surgery: an analysis of electronic logbook records. Ann R Coll Surg Engl 89(Suppl):106–109
Heath RM, Gate TCS, Halloran CM, Callaghan M, Paraoan MT, Blair SD (2007) The EWTD ‘triple whammy’: hitting surgical trainees where it hurts. Ann R Coll Surg Engl 89(Suppl):26–28
Lemaire R (2008) Strategies for blood management in orthopaedic and trauma surgery. J Bone Joint Surg Br 90(9):1128–1136
Carson JL, Willet LR (1993) Is a hemoglobin of 10 g/dL required for surgery? Med Clin N Am 77:335–347
Owens WD, Felts JA, Spitznagel EL Jr (1978) ASA physical status classifications: a study of consistency of ratings. Anaesthesia 49:239–243
Gruson KI, Aharonoff GB, Egol KA, Zuckerman JD, Koval KJ (2002) The relationship between admission hemoglobin level and outcome after hip fracture. J Orthop Trauma 16(1):39–44
Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, Koval KJ, Siu AL (2004) The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture. J Orthop Trauma 18(6):369–374
Lawrence VA, Silverstein JH, Cornell JE et al (2003) Higher Hb level is associated with better early functional recovery after hip fracture repair. Transfusion 43:1717–1722
Odumala AO, Ayekoloye CI, Packer G (2002) Predictors of excessive blood loss during operative treatment of hip fractures. J R Coll Surg Edinb 47:552–556
Foss NB, Kehlet H (2006) Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br 88(8):1053–1059
Chassot P-G, Delabays A, Spahn DR (2007) Perioperative antiplatelet therapy: the case for continuing therapy in patients at risk of myocardial infarction. Br J Anaesth 99(3):316–328
Inman D, Michla Y, Partington PF (2007) Perioperative management of trauma patients admitted on clopidogrel (Plavix)–—a survey of orthopaedic departments across the UK. Injury 38:625–630
Johansen A, White J, Turk A (2008) Clopidogrel therapy—implications for hip fracture surgery. Injury 39(10):1188–1190
Harty JA, McKenna P, Moloney D, D’Souza L, Masterson E (2007) Anti-platelet agents and surgical delay in elderly patients with hip fractures. J Orthop Surg (Hong Kong) 15(3):270–272
Manning BJ, O’Brien N, Aravindan S, Cahill RA, McGreal G, Redmond HP (2004) The effect of aspirin on blood loss and transfusion requirements in patients with femoral neck fractures. Injury 35(2):121–124
Juelsgaard P, Larsen UT, Søorensen JV, Madsen F, Søballe K (2001) Hypotensive epidural anesthesia in total knee replacement without tourniquet: reduced blood loss and transfusion. Reg Anesth Pain Med 26:105–110
Carless PA, Henry DA, Moxey AJ, O’Connell D, Brown T, Fergusson DA (2006) Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 4:CD001888
Parker MJ, Livingstone V, Clifton R, McKee A (2007) Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syste Rev 3:CD001825
Rajesparan K, Biant LC, Ahmad M, Field RE (2009) The effect of an intravenous bolus of tranexamic acid on blood loss in total hip replacement. J Bone Joint Surg Br 91(6):776–783
Baskies MA, Ruchelsman DE, Capeci CM, Zuckerman JD, Egol KA (2008) Operative experience in an orthopaedic surgery residency program: the effect of work-hour restrictions. J Bone Joint Surg Am 90(4):924–927
Oakley JE, Clewer GJ, Cool WP, Ford DJ (2005) The Effect of the EWTD on orthopaedic specialist training. Ann R Coll Surg Engl 87(Suppl):320–321
Morrison CA, Wyatt MM, Carrick MM (2009) Impact of the 80-hour work week on mortality and morbidity in trauma patients: an analysis of the National Trauma Data Bank. J Surg Res 154(1):157–162
Mahaluxmivala J, Bankes MJ, Nicolai P, Aldam CH, Allen PW (2001) The effect of surgeon experience on component positioning in 673 press fit condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty 16(5):635–640
Palan J, Gulati A, Andrew JG, Murray DW, Beard DJ (2009) The trainer, the trainee and the surgeons’ assistant: clinical outcomes following total hip replacement. J Bone Joint Surg Br 91(7):928–934
Browne JA, Pietrobon R, Olson SA (2009) Hip fracture outcomes: does surgeon or hospital volume really matter? J Trauma 66(3):809–814
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rose, B., Sindali, K., Soueid, H. et al. The effect of the grade of surgeon on blood loss in fractured neck-of-femur surgery. Eur J Orthop Surg Traumatol 23, 449–456 (2013). https://doi.org/10.1007/s00590-012-1015-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-012-1015-y