Abstract
Background
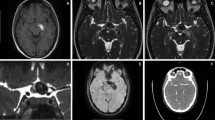
We describe 11 patients with hypertrophic olivary degeneration (HOD) after surgical resection or gamma knife radiosurgery for brainstem cavernous malformations. In addition, we statistically analyzed the predicting factors associated with the development of HOD.
Methods
From January 2001 to May 2011, a total of 73 patients (30 in the surgical group and 43 in the radiosurgery group) with brainstem cavernous malformations were treated in our institute. Of them, 11 patients (incidence: 15 %) developed HOD with high signal intensity on T2-weighted MRI during follow-up. The predicting factors (location, size, age, and treatment method) associated with the development of HOD were statistically analyzed.
Results
Among the 11 HOD patients, seven patients received surgical resection and four patients received gamma knife radiosurgery. Six patients had bilateral HOD and the remaining five patients had unilateral HOD. Overall HOD-associated symptoms presented in four patients, including three palatal tremors and one ataxia. In all four patients with symptoms, these symptoms disappeared incompletely within the clinical follow-up period. The size of the cavernous malformation, age of patient, and treatment methods were not significantly correlated with the development of HOD. A significantly higher incidence of HOD was associated with midbrain cavernous malformations than with pontine or medulla cavernous malformations.
Conclusions
HOD should be recognized as a non-infrequent complication of surgical resection or gamma knife radiosurgery within the brainstem, especially for midbrain cavernous malformations. In addition, to the best of our knowledge, this is the first report on HOD development after radiosurgery.



Similar content being viewed by others
References
Aberfeld DC (1966) The hypertrophic degeneration of the olives. Acta Neurol Scand 42:296–306
Akar S, Drappatz J, Hsu L, Blinder RA, Black PM, Kesari S (2008) Hypertrophic olivary degeneration after resection of a cerebellar tumor. J Neurooncol 87:341–345
Anderson JR, Treip CS (1973) Hypertrophic olivary degeneration and Purkinje cell degeneration in a case of long-standing head injury. J Neurol Neurosurg Psychiatry 36:826–832
Birbamer G, Buchberger W, Felber S, Aichner F (1992) MR appearance of hypertrophic olivary degeneration: temporal relationships. AJNR Am J Neuroradiol 13:1501–1503
Conforto AB, Smid J, Marie SK, Ciriaco JG, Santoro PP, CdaC L, Mansur LL, Scaff M (2005) Bilateral olivary hypertrophy after unilateral cerebellar infarction. Arq Neuropsiquiatr 63:321–323
Diehl GE, Wilmes E (1990) Etiology and clinical aspects of palatal myoclonus. Laryngorhinootologie 69:369–372
Gatlin JL, Wineman R, Schlakman B, Buciuc R, Khan M (2011) Hypertrophic olivary degeneration after resection of a pontine cavernous malformation: a case report. J Radiol Case Rep 5:24–29
Goto N, Kaneko M (1981) Olivary enlargement: chronological and morphometric analyses. Acta Neuropathol 54:275–282
Goyal M, Versnick E, Tuite P, Cyr JS, Kucharczyk W, Montanera W, Willinsky R, Mikulis D (2000) Hypertrophic olivary degeneration: metaanalysis of the temporal evolution of MR findings. AJNR Am J Neuroradiol 21:1073–1077
Guillain G, Mollaret P (1931) Deus de myoclonies synchrones et rhythmees velopharyngolaryngo-oculo-diaphragmatiques. Rev Neurol 12:545–546
Hanihara T, Amano N, Takahashi T, Itoh Y, Yagishita S (1998) Hypertrophy of the inferior olivary nucleus in patients with progressive supranuclear palsy. Eur Neurol 39:97–102
Harter DH, Davis A (2004) Hypertrophic olivary degeneration after resection of a pontine cavernoma. Case illustration. J Neurosurg 100:717
Hornyak M, Osborn AG, Couldwell WT (2008) Hypertrophic olivary degeneration after surgical removal of cavernous malformations of the brain stem: report of four cases and review of the literature. Acta Neurochir (Wien) 150:149–156, discussion 156
Horoupian DS, Wisniewski H (1971) Neurofilamentous hyperplasia in inferior olivary hypertrophy. J Neuropathol Exp Neurol 30:571–582
Macht S, Hanggi D, Turowski B (2009) Hypertrophic olivary degeneration following pontine cavernoma hemorrhage: a typical change accompanying lesions in the Guillain-Mollaret triangle. Klin Neuroradiol 19:235–237
Oppenheim H (1887) Über Olivendegeneration bei Atheromatese der basalen Hirnarterien. Berl Klin Wschr 34:638–639
Phatouros CC, McConachie NS (1998) Hypertrophic olivary degeneration: case report in a child. Pediatr Radiol 28:830–831
Robin JJ, Alcala H (1975) Olivary hypertrophy without palatal myoclonus associated with a metastatic lesion to the pontine tegmentum. Neurology 25:771–775
Samuel M, Torun N, Tuite PJ, Sharpe JA, Lang AE (2004) Progressive ataxia and palatal tremor (PAPT): clinical and MRI assessment with review of palatal tremors. Brain 127:1252–1268
Shepherd GM, Tauboll E, Bakke SJ, Nyberg-Hansen R (1997) Midbrain tremor and hypertrophic olivary degeneration after pontine hemorrhage. Mov Disord 12:432–437
Tsui EY, Cheung YK, Mok CK, Yuen MK, Chan JH (2000) Hypertrophic olivary degeneration following surgical excision of brainstem cavernous hemangioma: a case report. Clin Imaging 23:215–217
Uchino A, Hasuo K, Uchida K, Matsumoto S, Tsukamoto Y, Ohno M, Masuda K (1993) Olivary degeneration after cerebellar or brain stem haemorrhage: MRI. Neuroradiology 35:335–338
Vaidhyanath R, Thomas A, Messios N (2010) Bilateral hypertrophic olivary degeneration following surgical resection of a posterior fossa epidermoid cyst. Br J Radiol 83:e211–e215
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
This is a very interesting article. Brain stem lesions have been considered untouchable by many for a long time, but with advances in microsurgery and the development of less invasive radiosurgical tools, there is an increased willingness to enter this region and treat/operate upon different pathologies. Given the relatively benign course of cavernomas, post-surgical or radiosurgical effects are observable and their course possible to follow. It is of note that whichever is the intervention, the likelihood of development of hypertrophic olivary degeneration is the same, and it is reassuring to note that the changes are not always permanent.
Andras Kemeny
Sheffield, UK
Rights and permissions
About this article
Cite this article
Yun, JH., Ahn, J.S., Park, J.C. et al. Hypertrophic olivary degeneration following surgical resection or gamma knife radiosurgery of brainstem cavernous malformations: an 11-case series and a review of literature. Acta Neurochir 155, 469–476 (2013). https://doi.org/10.1007/s00701-012-1567-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1567-y