Abstract
Background
Cervical spondylotic myelopathy (CSM) may be caused by static and dynamic spinal cord compression, particularly during neck extension. Dynamic compression may be better evaluated with dynamic magnetic resonance (MR) images. We performed a retrospective study to determine the clinical indication for dynamic MR imaging, and conducted a survey regarding image interpretation by clinicians.
Method
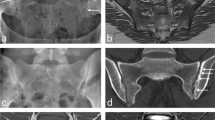
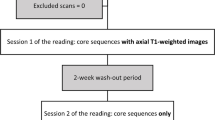
A total of 32 patients (M:F = 20:12, 60.1 ± 10.7 years) who had undergone neutral/extension cervical MR imaging were included. The study population consisted of 22 patients with signs of cervical myelopathy (M group) and 10 patients without signs of myelopathy (NM group). The number of compression levels (complete obliteration of the anterior and posterior subarachnoid space) was assessed at each level in mid-sagittal, T2-weighted, neutral and extension MR images. Reproduced images from 22 patients in the M group were randomly arranged, and four experienced spine surgeons at four different institutes interpreted them to reach a clinicians’ agreement. The agreements were then assessed with inter-rater correlation coefficients (ICC).
Results
Analysis with extension MR images found an increased number of compression levels in 23/32 (72 %) of patients; 20/22 in the M group and 3/10 in the NM group (p < 0.01, chi-squared test), as compared to findings of the neutral MR images. Clinical factors for increased compression levels in extension MR images were age (p < 0.01, 63.3 ± 10.0 years vs. 51.9 ± 8.1) and signs of myelopathy (p < 0.01, odds ratio, 23.33). Clinician agreement was improved with extension MR images; ICC was 0.67 with neutral and 0.81 with extension MR images.
Conclusions
The evaluation of CSM may be improved with dynamic MR images. Dynamic MR scanning may be considered for elderly patients with signs of myelopathy, but an interpretation for asymptomatic spinal compression based exclusively on extension MR image should be made with caution.





Similar content being viewed by others
References
Chen CJ, Hsu HL, Niu CC, Chen TY, Chen MC, Tseng YC, Wong YC, Wang LJ (2003) Cervical degenerative disease at flexion-extension MR imaging: prediction criteria. Radiology 227:136–142
Fujiwara K, Yonenobu K, Hiroshima K, Ebara S, Yamashita K, Ono K (1988) Morphometry of the cervical spinal cord and its relation to pathology in cases with compression myelopathy. Spine (Phila Pa 1976) 13:1212–1216
Glaser JA, Cure JK, Bailey KL, Morrow DL (2001) Cervical spinal cord compression and the Hoffmann sign. Iowa Orthop J 21:49–52
Guppy KH, Hawk M, Chakrabarti I, Banerjee A (2009) The use of flexion-extension magnetic resonance imaging for evaluating signal intensity changes of the cervical spinal cord. J Neurosurg Spine 10:366–373
Harada T, Tsuji Y, Mikami Y, Hatta Y, Sakamoto A, Ikeda T, Tamai K, Hase H, Kubo T (2010) The clinical usefulness of preoperative dynamic MRI to select decompression levels for cervical spondylotic myelopathy. Magn Reson Imaging 28:820–825
Kim CH, Chung CK, Hahn S (2013) Autologous Iliac Bone Graft with Anterior Plating is Advantageous Over the Stand-alone Cage for Segmental Lordosis in Single-level Cervical Disc Disease. Neurosurgery:257–266
Lebl DR, Hughes A, Cammisa FP Jr, O'Leary PF (2011) Cervical spondylotic myelopathy: pathophysiology, clinical presentation, and treatment. HSS J 7:170–178
Matsumoto M, Chiba K, Ishikawa M, Maruiwa H, Fujimura Y, Toyama Y (2001) Relationships between outcomes of conservative treatment and magnetic resonance imaging findings in patients with mild cervical myelopathy caused by soft disc herniations. Spine (Phila Pa 1976) 26:1592–1598
Muhle C, Weinert D, Falliner A, Wiskirchen J, Metzner J, Baumer M, Brinkmann G, Heller M (1998) Dynamic changes of the spinal canal in patients with cervical spondylosis at flexion and extension using magnetic resonance imaging. Invest Radiol 33:444–449
Nurick S (1972) The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain 95:87–100
Oshima Y, Seichi A, Takeshita K, Chikuda H, Ono T, Baba S, Morii J, Oka H, Kawaguchi H, Nakamura K, Tanaka S (2012) Natural course and prognostic factors in patients with mild cervical spondylotic myelopathy with increased signal intensity on t2-weighted magnetic resonance imaging. Spine (Phila Pa 1976) 37:1909–1913
Schlamann M, Reischke L, Klassen D, Maderwald S, Bohner V, Kollia K, Ladd ME, Forsting M, Wanke I (2007) Dynamic magnetic resonance imaging of the cervical spine using the NeuroSwing System. Spine (Phila Pa 1976) 32:2398–2401
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Yarbrough CK, Murphy RK, Ray WZ, Stewart TJ (2012) The natural history and clinical presentation of cervical spondylotic myelopathy. Adv Orthop 2012:480643
Zhang L, Zeitoun D, Rangel A, Lazennec JY, Catonne Y, Pascal-Moussellard H (2011) Preoperative evaluation of the cervical spondylotic myelopathy with flexion-extension magnetic resonance imaging: about a prospective study of fifty patients. Spine (Phila Pa 1976) 36:E1134–1139
Acknowledgement
The authors appreciate the statistical advice from the Medical Research Collaborating Center at the Seoul National University Hospital and the Seoul National University College of Medicine.
Conflict of Interest
This work was supported by a National Research Foundation of Korea (NRF) grant, funded by the Korean government (MSIP)(2010-0028631). The authors report no conflict of interest concerning the materials or methods used in this study or the findings described in this paper. No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, C.H., Chung, C.K., Kim, KJ. et al. Cervical extension magnetic resonance imaging in evaluating cervical spondylotic myelopathy. Acta Neurochir 156, 259–266 (2014). https://doi.org/10.1007/s00701-013-1951-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1951-2