Abstract
Background
For patients with single-level cervical radiculopathy, various types of motion preservation surgeries, such as total disc replacement (TDR), posterior cervical foraminotomy (PCF) and posterior percutaneous endoscopic foraminotomy and discectomy (PECF), are available. In addition to motion preservation, the quality of motion is an important issue. The aim of the present study was to evaluate the influence of these surgeries on cervical motion by comparing the instantaneous axis of rotation (IAR) among PECF, TDR and PCF at the index and superior/inferior adjacent segments.
Methods
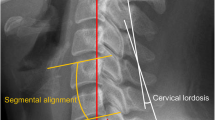
A retrospective review was performed of patients who underwent index surgery at C5–6 for cervical single-level foraminal disc herniation or foraminal stenosis. Patients with minimal degeneration at the index and other cervical spinal levels and flexion/extension cervical lateral radiographs both preoperatively and 6 months postoperatively were included (PECF, 11 patients; TDR, 11 patients; PCF, 12 patients). The IARs were calculated at the index segment and segments above and below the index segment from the flexion and extension cervical lateral radiographs, which were obtained preoperatively and 6 months postoperatively. A standardized cervical normogram was referenced to qualify shifts in the IAR.
Results
Postoperatively, neck pain was significantly decreased, with no difference among the surgical methods. The IARs were not significantly changed after the PECF. Although significant inferior shift occurred at C6–7 after TDR (p = 0.02), the shift occurred within the normal range in the cervical normogram. However, significant inferior shifts in the IARs occurred after PCF at C5–6 (p = 0.02) and C6–7 (p = 0.02), and the IARs moved out of the normal range.
Conclusions
The IARs were significantly changed after PCF at either the index segment or the adjacent segment below. The shifts in IAR at the index and adjacent segments were not significant after PECF and TDR. The sample size was too small to allow definitive conclusions, but the present study showed that PECF may be another alternative to motion preservation surgeries.



Similar content being viewed by others
References
Alvin MD, Qureshi S, Klineberg E, Riew KD, Fischer DJ, Norvell DC, Mroz TE (2014) Cervical degenerative disease: systematic review of economic analyses. Spine (Phila Pa 1976) 39:S53–S64
Amevo B, Aprill C, Bogduk N (1992) Abnormal instantaneous axes of rotation in patients with neck pain. Spine (Phila Pa 1976) 17:748–756
Amevo B, Macintosh JE, Worth D, Bogduk N (1991) Instantaneous axes of rotation of the typical cervical motion segments: I. An empirical study of technical errors. Clin Biomech (Bristol, Avon) 6:31–37
Amevo B, Worth D, Bogduk N (1991) Instantaneous axes of rotation of the typical cervical motion segments: a study in normal volunteers. Clin Biomech (Bristol, Avon) 6:111–117
Amevo B, Worth D, Bogduk N (1991) Instantaneous axes of rotation of the typical cervical motion segments: II. Optimization of technical errors. Clin Biomech (Bristol, Avon) 6:38–46
Anderst W, Baillargeon E, Donaldson W, Lee J, Kang J (2013) Motion path of the instant center of rotation in the cervical spine during in vivo dynamic flexion-extension: implications for artificial disc design and evaluation of motion quality after arthrodesis. Spine (Phila Pa 1976) 38:E594–E601
Barrey C, Champain S, Campana S, Ramadan A, Perrin G, Skalli W (2012) Sagittal alignment and kinematics at instrumented and adjacent levels after total disc replacement in the cervical spine. Eur Spine J 21:1648–1659
Bogduk N, Amevo B, Pearcy M (1995) A biological basis for instantaneous centres of rotation of the vertebral column. Proc Inst Mech Eng H 209:177–183
Bogduk N, Mercer S (2000) Biomechanics of the cervical spine. I: normal kinematics. Clin Biomech 15:633–648
Chin-See-Chong TC, Gadjradj PS, Boelen RJ, Harhangi BS (2017) Current practice of cervical disc arthroplasty: a survey among 383 AOSpine international members. Neurosurg Focus 42:E8
Harrod CC, Hilibrand AS, Fischer DJ, Skelly AC (2012) Adjacent segment pathology following cervical motion-sparing procedures or devices compared with fusion surgery: a systematic review. Spine (Phila Pa 1976) 37:S96–S112
Jagannathan J, Sherman JH, Szabo T, Shaffrey CI, Jane JA (2009) The posterior cervical foraminotomy in the treatment of cervical disc/osteophyte disease: a single-surgeon experience with a minimum of 5 years’ clinical and radiographic follow-up. J Neurosurg Spine 10:347–356
Jho HD, Kim WK, Kim MH (2002) Anterior microforaminotomy for treatment of cervical radiculopathy: part 1—disc-preserving “functional cervical disc surgery”. Neurosurgery 51:S46–S53
Kim CH, Kim KT, Chung CK, Park SB, Yang SH, Kim SM, Sung JK (2015) Minimally invasive cervical foraminotomy and diskectomy for laterally located soft disk herniation. Eur Spine J 24:3005–3012
Kim CH, Shin KH, Chung CK, Park SB, Kim JH (2015) Changes in cervical sagittal alignment after single-level posterior percutaneous endoscopic cervical diskectomy. Global Spine J 5:31–38
Kim HJ, Nemani VM, Piyaskulkaew C, Vargas SR, Riew KD (2016) Cervical Radiculopathy: incidence and treatment of 1,420 consecutive cases. Asian Spine J 10:231–237
Kim KT, Cho DC, Sung JK, Kim YB, Kim DH (2017) Comparative analysis between total disc replacement and posterior foraminotomy for posterolateral soft disc herniation with unilateral radiculopathy: clinical and biomechanical results of a minimum 5 years follow-up. J Korean Neurosurg Soc 60:30–39
Kong L, Ma Q, Meng F, Cao J, Yu K, Shen Y (2017) The prevalence of heterotopic ossification among patients after cervical artificial disc replacement: a systematic review and meta-analysis. Medicine (Baltimore) 96:e7163
Lee H, Nicholson LL, Adams RD, Maher CG, Halaki M, Bae SS (2006) Development and psychometric testing of Korean language versions of 4 neck pain and disability questionnaires. Spine (Phila Pa 1976) 31:1841–1845
Lee SE, Chung CK, Jahng TA (2012) Early development and progression of heterotopic ossification in cervical total disc replacement. J Neurosurg Spine 16:31–36
Lind B, Zoega B, Anderson PA (2007) A radiostereometric analysis of the Bryan cervical disc prosthesis. Spine (Phila Pa 1976) 32:885–890 discussion 891
Liu B, Liu Z, VanHoof T, Kalala J, Zeng Z, Lin X (2014) Kinematic study of the relation between the instantaneous center of rotation and degenerative changes in the cervical intervertebral disc. Eur Spine J 23:2307–2313
Liu B, Zeng Z, Hoof TV, Kalala JP, Liu Z, Wu B (2015) Comparison of hybrid constructs with 2-level artificial disc replacement and 2-level anterior cervical discectomy and fusion for surgical reconstruction of the cervical spine: a kinematic study in whole cadavers. Med Sci Monit 21:1031–1037
Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC (2008) Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech 21:288–292
Ohnmeiss DD, Guyer RD (2009) Twenty-four month follow-up for reporting results of spinal implant studies: is this guideline supported by the literature? SAS J 3:100–107
Park DK, Lin EL, Phillips FM (2011) Index and adjacent level kinematics after cervical disc replacement and anterior fusion: in vivo quantitative radiographic analysis. Spine (Phila Pa 1976) 36:721–730
Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD (2014) Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J 14:1228–1234
Park MS, Moon SH, Kim TH, Lee SY, Jo YG, Riew KD (2015) Relationship between modic changes and facet joint degeneration in the cervical spine. Eur Spine J 24:2999–3004
Park SB, Jahng TA, Chung CK (2012) Remodeling of adjacent spinal alignments following cervical arthroplasty and anterior discectomy and fusion. Eur Spine J 21:322–327
Penning L (1978) Normal movements of the cervical spine. AJR Am J Roentgenol 130:317–326
Powell JW, Sasso RC, Metcalf NH, Anderson PA, Hipp JA (2010) Quality of spinal motion with cervical disk arthroplasty: computer-aided radiographic analysis. J Spinal Disord Tech 23:89–95
Riew KD, Cheng I, Pimenta L, Taylor B (2007) Posterior cervical spine surgery for radiculopathy. Neurosurgery 60:S57–S63
Riew KD, Schenk-Kisser JM, Skelly AC (2012) Adjacent segment disease and C-ADR: promises fulfilled? Evid Based Spine Care J 3:39–46
Ruetten S, Komp M, Merk H, Godolias G (2007) A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9-mm endoscopes: prospective 2-year results of 87 patients. Minim Invasive Neurosurg 50:219–226
Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 33:940–948
Selvik G (1989) Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand Suppl 232:1–51
Singhatanadgige W, Kang DG, Luksanapruksa P, Peters C, Riew KD (2016) Correlation and reliability of cervical sagittal alignment parameters between lateral cervical radiograph and lateral whole-body EOS Stereoradiograph. Global Spine J 6:548–554
Skovrlj B, Gologorsky Y, Haque R, Fessler RG, Qureshi SA (2014) Complications, outcomes, and need for fusion after minimally invasive posterior cervical foraminotomy and microdiscectomy. Spine J 14:2405–2411
Woltring HJ, Long K, Osterbauer PJ, Fuhr AW (1994) Instantaneous helical axis estimation from 3-D video data in neck kinematics for whiplash diagnostics. J Biomech 27:1415–1432
Won S, Kim CH, Chung CK, Choi Y, Park SB, Moon JH, Heo W, Kim SM (2016) Clinical outcomes of single-level posterior percutaneous endoscopic cervical foraminotomy for patients with less cervical lordosis. J Minim Invasive Spine Surg Tech 1:11–17
Won S, Kim CH, Chung CK, Choi Y, Park SB, Moon JH, Heo W, Kim SM (2017) Comparison of cervical sagittal alignment and kinematics after posterior full-endoscopic cervical foraminotomy and discectomy according to preoperative cervical alignment. Pain Physician 20:77–87
Funding
Seoul National University Hospital provided financial support in the form of a research grant (Grant No. 0320160210; 2016–1062). The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Drs. C.H. Kim, K.T. Kim, C.K. Chung, Y. Choi, and T.H. Park had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Drs. C.H. Kim, K.T. Kim, T.H. Park and C.K. Chung designed the study protocol. Drs. C.H. Kim, and T.H. Park managed the literature searches and summaries of the previous related works and wrote the first draft of the manuscript. Drs. C.K. Chung, K.T. Kim and Y. Choi provided revisions for intellectual content and the final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
C.H. Kim is a consultant at Richard Wolf GmbH. All the other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the institutional review board of Seoul National University Hospital (H-1702-015-829).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kim, C.H., Park, T.H., Chung, C.K. et al. Changes in cervical motion after cervical spinal motion preservation surgery. Acta Neurochir 160, 397–404 (2018). https://doi.org/10.1007/s00701-017-3375-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3375-x