Abstract
Objectives
This preliminary randomized double-blind controlled trial was performed to test the efficacy of ultramicronized palmitoylethanolamide treatment in the burning mouth syndrome.
Materials and methods
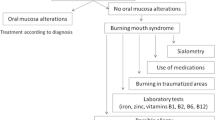
Patients with referred burning mouth intensity greater than 4, according to the Numeric Rating Scale, were included in the study according to established inclusion and exclusion criteria. Patients were randomized into two groups and received either placebo or ultramicronized palmitoylethanolamide 600 mg twice daily for 60 days. Patients were assessed at baseline, 30 and 60 days after treatment start, and 4 months after treatment discontinuation. In order to evaluate the change in the burning mouth sensation over time, the generalized linear mixed model was employed.
Results
A total of 35 patients were considered eligible, among which 6 withdrew prior to the end of treatment. A statistically significant reduction of burning mouth sensation (p < 0.0132) was registered at the end of the active treatment in the ultramicronized palmitoylethanolamide group compared to the placebo one. Any side effect related to the active treatment was neither observed nor reported both by patients and by physicians.
Conclusions
The significant decrease of burning sensation in the ultramicronized palmitoylethanolamide group compared to the placebo group suggests to consider this naturally occurring molecule as a viable therapy in the management of burning mouth syndrome.
Clinical relevance
The use of an effective compound to manage the burning mouth syndrome, devoid of adverse effects for the patient and that does not interfere with other pharmacological therapies, could find wide employability from clinicians.


Similar content being viewed by others
References
Gurvits GE, Tan A (2013) Burning mouth syndrome. World J Gastroenterol 19:665–672
Salerno C, Di Stasio D, Petruzzi M, Lauritano D, Gentile E, Guida A, Maio C, Tammaro M, Serpico R, Lucchese A (2016) An overview of burning mouth syndrome. Front Biosci (Elite Ed) 1 8:213–218
Fedele S, Fricchione G, Porter SR, Mignogna MD (2007) Burning mouth syndrome (stomatodynia). QJM 100:527–530
Vellappally S (2016) Burning mouth syndrome: a review of the etiopathologic factors and management. J Contemp Dent Pract 17(2):171–176
Lauria G, Majorana A, Borgna M, Lombardi R, Penza P, Padovani A, Sapelli P (2005) Trigeminal small-fiber sensory neuropathy causes burning mouth syndrome. Pain 115:332–337
Yilmaz Z, Renton T, Yiangou Y, Zakrzewska J, Chessell IP, Bountra C, Anand P (2007) Burning mouth syndrome as a trigeminal small fibre neuropathy: increased heat and capsaicin receptor TRPV1 in nerve fibres correlates with pain score. J Clin Neurosci 14:864–871
Borsani E, Majorana A, Cocchi MA, Conti G, Bonadeo S, Padovani A, Lauria G, Bardellini E, Rezzani R, Rodella LF (2014) Epithelial expression of vanilloid and cannabinoid receptors: a potential role in burning mouth syndrome pathogenesis. Histol Histopathol 29(4):523–533
Barry A, O'Halloran KD, McKenna JP, McCreary C, Harhen B, Kerr DM, Finn DP, Downer EJ (2018) Plasma N-acylethanolamine and endocannabinoid levels in burning mouth syndrome: potential role in disease pathogenesis. J Oral Pathol Med 47(4):440–442
Beneng K, Yilmaz Z, Yiangou Y, McParland H, Anand P, Renton T (2010) Sensory purinergic receptor P2X3 is elevated in burning mouth syndrome. Int J Oral Maxillofac Surg 39:815–819
Ueda N, Tsuboi K, Uyama T (2010) Enzymological studies on the biosynthesis of N-acylethanolamines. Biochim Biophys Acta 1801:1274–1285
Epps DE, Schmid PC, Natarajan V, Schmid HH (1979) N-Acylethanolamine accumulation in infarcted myocardium. Biochem Biophys Res Commun 90:628–633
Petrosino S, Di Marzo V (2017) The pharmacology of palmitoylethanolamide and first data on the therapeutic efficacy of some of its new formulations. Br J Pharmacol 174(11):1349–1365
Costa B, Comelli F, Bettoni I, Giagoni G (2008) The endogenous fatty acid amide, palmitoylethanolamide, reduces neuropathic pain after systemic administration in mice: involvement of CB1, TRPV1 and PPARgamma receptors and neurotrophic factors. Pain 139:541–550
Bettoni I, Comelli F, Colombo A, Bonfanti P, Costa B (2013) Non-neuronal cell modulation relieves neuropathic pain: efficacy of the endogenous lipid palmitoylethanolamide. CNS Neurol Disord Drug Targets 12:34–44
Luongo L, Guida F, Boccella S, Bellini G, Gatta L, Rossi F, de Novellis V, Maione S (2013) Palmitoylethanolamide reduces formalin-induced neuropathic-like behaviour through spinal gial/microglial phenotypical changes in mice. CNS Neurol Disord Drug Targets 12:45–54
Gatti A, Lazzari M, Gianfelice V, Di Paolo A, Sabato E, Sabato AF (2012) Palmitoylethanolamide in the treatment of chronic pain caused by different etiopathogeneses. Pain Med 13:1121–1130
Schifilliti C, Cucinotta L, Fedele V, Ingegnosi C, Luca S, Leotta C (2014) Micronized palmitoylethanolamide reduces the symptoms of neuropathic pain in diabetic patients. Pain Res Treat 2014:849623
Calabrò RS, Gervasi G, Marino S, Mondo PN, Bramanti P (2010) Misdiagnosed chronic pelvic pain: pudendal neuralgia responding to a novel use of palmitoylethanolamide. Pain Med 11:781–784
Paladini A, Fusco M, Cenacchi T, Schievano C, Piroli A, Varrassi G (2016) Palmitoylethanolamide, a special food for medical purposes, in the treatment of chronic pain: a pooled data meta-analysis. Pain Physician 19:11–24
Klasser GD, Gremillion HA (2012) Neuropathic orofacial pain patients in need of dental care. J Can Dent Assoc 78:c83
McDonough P, McKenna JP, McCreary C, Downer EJ (2014) Neuropathic orofacial pain: cannabinoids as a therapeutic avenue. Int J Biochem Cell Biol 55:72–78. https://doi.org/10.1016/j.biocel.2014.08.007
Barry A, O'Halloran KD, McKenna JP, McCreary C, Downer EJ (2018) Plasma IL-8 signature correlates with pain and depressive symptomatology in patients with burning mouth syndrome: results from a pilot study. J Oral Pathol Med 47(2):158–165
(2016) The International Classification of Headache Disorders, 3rd edition. International Headache Society
Lamey PJ, Lewis MA (1989) Oral medicine in practice: burning mouth syndrome. Br Dent J 167:197–200
Ahmed N, Bestall J, Payne S, Noble B, Ahmedzai S (2009) The use of cognitive interviewing methodology in the design and testing of a screening tool for supportive and palliative care needs. Support Care Cancer 17(6):665–673
Patton LL, Siegel MA, Benoliel R, De Laat A (2007) Management of burning mouth syndrome: systematic review and management recommendations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103 Suppl:S39.e1–13
Adamo D, Sardella A, Varoni E, Lajolo C, Biasotto M, Ottaviani G, Vescovi P, Simonazzi T, Pentenero M, Ardore M, Spadari F, Bombeccari G, Montebugnoli L, Gissi DB, Campisi G, Panzarella V, Carbone M, Valpreda L, Giuliani M, Aria M, Lo Muzio L, Mignogna MD (2018) The association between burning mouth syndrome and sleep disturbance: a case-control multicentre study. Oral Dis 24(4):638–649. https://doi.org/10.1111/odi.12807 Epub 2018 Mar 13
Jääskeläinen SK, Rinne JO, Forssell H, Tenovuo O, Kaasinen V, Sonninen P, Bergman J (2001) Role of the dopaminergic system in chronic pain—a fluorodopa PET study. Pain 90:257–260
Hagelberg N, Forssell H, Aalto S, Rinne JO, Scheinin H, Taiminen T, Någren K, Eskola O, Jääskeläinen SK (2003) Altered dopamine D2 receptor binding in atypical facial pain. Pain 106:43–48
Charleston L (2013) Burning mouth syndrome: a review of recent literature. Curr Pain Headache Rep 17:336. https://doi.org/10.1007/s11916-013-0336-9
Buchanan JA, Zakrzewska JM (2010) Burning mouth syndrome. BMJ Clin Evid 19;2010
White TL, Kent PF, Kurtz DB, Emko P (2004) Effectiveness of gabapentin for treatment of burning mouth syndrome. Arch Otolaryngol Head Neck Surg 130:786–788
Heckmann SM, Heckmann JG, Ungethüm A, Hujoel P, Hummel T (2006) Gabapentin has little or no effect in the treatment of burning mouth syndrome—results of an open-label pilot study. Eur J Neurol 13:e6–e7
López-D’alessandro E, Escovich L (2011) Combination of alpha lipoic acid and gabapentin, its efficacy in the treatment of burning mouth syndrome: a randomized, double-blind, placebo controlled trial. Med Oral Patol Oral Cir Bucal 16:e635–e640
Grushka M, Epstein JB, Gorsky M (2002) Burning mouth syndrome. Am Fam Physician 65:615–620
Skaper SD, Facci L, Giusti P (2013) Glia and mast cells as targets for palmitoylethanolamide, an anti-inflammatory and neuroprotective lipid mediator. Mol Neurobiol 48:340–352
Skaper SD, Facci L (2012) Mast cell – glia axis in neuroinflammation and therapeutic potential of the anandamide congener palmitoylethanolamide. Philos Trans R Soc Lond Ser B Biol Sci 367(1607):3312–3325
Muccioli GG, Stella N (2008) Microglia produce and hydrolyze palmitoylethanolamide. Neuropharmacology 54(1):16–22
De Filippis D, Luongo L, Cipriano M, Palazzo E, Cinelli MP, De Novellis V, Maione S, Iuvone T (2011) Palmitoylethanolamide reduces granuloma-induced hyperalgesia by modulation of mast cell activation in rats. Mol Pain 7:3
Iannotti FA, Di Marzo V, Petrosino S (2016) Endocannabinoids and endocannabinoid-related mediators: targets, metabolism and role in neurological disorders. Prog Lipid Res 62:107–128. https://doi.org/10.1016/j.plipres.2016.02.002
Di Cesare Mannelli L, D'Agostino G, Pacini A, Russo R, Zanardelli M, Ghelardini C, Calignano A (2013) Palmitoylethanolamide is a disease-modifying agent in peripheral neuropathy: pain relief and neuroprotection share a PPAR-alpha-mediated mechanism. Mediat Inflamm 2013:328797. https://doi.org/10.1155/2013/328797
Skaper SD, Facci L, Fusco M, Della Valle MF, Zusso M, Costa B, Giusti P (2014) Palmitoylethanolamide, a naturally occurring disease-modifying agent in neuropathic pain. Inflammopharmacology 22(2):79–94
Ambrosino P, Soldovieri MV, Russo C, Taglialatela M (2013) Activation and desensitization of TRPV1 channels in sensory neurons by the PPARα agonist palmitoylethanolamide. Br J Pharmacol 168(6):1430–1444. https://doi.org/10.1111/bph.12029
Esposito E, Cuzzocrea S (2013) Palmitoylethanolamide is a new possible pharmacological treatment for the inflammation associated with trauma. Mini Rev Med Chem 13(2):237–255
Stensson N, Ghafouri N, Ernberg M, Mannerkorpi K, Kosek E, Gerdle B, Ghafouri B (2018) The relationship of endocannabinoidome lipid mediators with pain and psychological stress in women with fibromyalgia—a case control study. J Pain pii S1526-5900(18):30197–30194. https://doi.org/10.1016/j.jpain.2018.05.008
Kuten-Shorrer M, Kelley JM, Sonis ST, Treister NS (2014) Placebo effect in burning mouth syndrome: a systematic review. Oral Dis 20:1–6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the University’s Ethic Committee of Trieste (registration number 405/69/2010).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ottaviani, G., Rupel, K., Gobbo, M. et al. Efficacy of ultramicronized palmitoylethanolamide in burning mouth syndrome-affected patients: a preliminary randomized double-blind controlled trial. Clin Oral Invest 23, 2743–2750 (2019). https://doi.org/10.1007/s00784-018-2720-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-018-2720-7