Abstract
Objectives
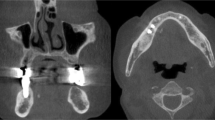
Sialolithiasis is the most common cause of chronic sialadenitis of the submandibular gland (SMG). Symptomatic superficial lobe stones are often treated by submandibulectomy. A gland preserving operation allows for transoral stone removal through endoscopically assisted sialolithotomy. Herein, we provide clinical and sonographical follow-up data in patients who underwent sialolithotomy under general anesthesia.
Materials and methods
Sixty patients treated at the Department of Oral and Maxillofacial Surgery at Düsseldorf University Hospital for superficial lobe sialolithiasis of SMG were included in this study. All received transoral sialolithotomy under general anesthesia. Follow-up was conducted via standardized patient questionnaires, clinical examination, and B-mode and color Doppler sonography.
Results
Mean patient age was 48.9 years. 56.6% of right and 43.4% of left SMG were affected. Mean follow-up was 45 months. Fifty-five of 59 detected stones could be removed. Mean operation time was 71 min. 3.3% of patients reported recurrent episodes of postoperative pain and 10% felt recurrent episodes of gland swelling. Persistent postoperative lingual nerve hypesthesia was described in one patient. No facial nerve damages occurred. Salivary flow rates remained reduced in most of the affected glands upon stone removal. Sonographical follow-up data of the previously affected SMG after intraoral endoscopy-assisted sialolithotomy showed a regular gland size in 70.8% of cases, a parenchyma free of inflammation in 93.8%, and without signs of fibrosis in 72.9% of cases. 68.7% of patients showed a regular structure of Wharton’s duct at time of follow-up. In total, 89.6% of patients were diagnosed stone-free within both glands on follow-up. No case required subsequent submandibulectomy.
Conclusions
Sialolithotomy of Wharton’s duct for removal of stones from the SMG’s superficial lobe is a promising alternative to submandibulectomy.
Clinical relevance
Reduction of postoperative morbidity through endoscopically assisted sialolithotomy for removal of superficial lobe stones from SMG.
Trial registration
Ethics Committee of Heinrich-Heine-University Düsseldorf (no. 5586)





Similar content being viewed by others
Abbreviations
- SMG:
-
Submandibular gland
- CBCT:
-
Cone-beam computed tomography
- dSGE:
-
Diagnostic sialendoscopy
- iSGE:
-
Interventional sialendoscopy
- ESWL:
-
Extracorporeal shock wave lithotripsy
References
Koch M, Zenk J, Iro H (2008) Diagnostic and interventional sialoscopy in obstructive diseases of the salivary glands. Hno 56(2):139–144
Capaccio P, Clemente IA, McGurk M, Bossi A, Pignataro L (2011) Transoral removal of hiloparenchymal submandibular calculi: a long-term clinical experience. Eur Arch Otorhinolaryngol 268(7):1081–1086
Fusconi M, Petrozza V, Schippa S, de Vincentiis M, Familiari G, Pantanella F, Cirenza M, Iebba V, Battaglione E, Greco A, Gallipoli C, Campo F, Gallo A (2016) Bacterial biofilm in salivary gland stones: cause or consequence? Otolaryngol Head Neck Surg 154(3):449–453
Escudier MP, Brown JE, Drage NA, McGurk M (2003) Extracorporeal shockwave lithotripsy in the management of salivary calculi. Br J Surg 90(4):482–485
Farnaud SJ et al (2010) Saliva: physiology and diagnostic potential in health and disease. ScientificWorldJournal 10:434–456
Levy DM, Remine WH, Devine KD (1962) Salivary gland calculi. Pain, swelling associated with eating. Jama 181:1115–1119
Shahoon H, Farhadi S, Hamedi R (2015) Giant sialoliths of Wharton duct: report of two rare cases and review of literature. Dent Res J (Isfahan) 12(5):494–497
Sigismund PE, Zenk J, Koch M, Schapher M, Rudes M, Iro H (2015) Nearly 3,000 salivary stones: some clinical and epidemiologic aspects. Laryngoscope 125(8):1879–1882
Vogl TJ, al-Nawas B, Beutner D, Geisthoff U, Gutinas-Lichius O, Naujoks C, Reich R, Schröder U, Sproll C, Teymoortash A, Ußmüller J, Wittekindt C, Zenk J, Fischer S (2014) Updated S2K AWMF guideline for the diagnosis and follow-up of obstructive sialadenitis--relevance for radiologic imaging. Rofo 186(9):843–846
Terraz S, Poletti PA, Dulguerov P, Dfouni N, Becker CD, Marchal F, Becker M (2013) How reliable is sonography in the assessment of sialolithiasis? AJR Am J Roentgenol 201(1):W104–W109
Nahlieli O, Shacham R, Zagury A, Bar T, Yoffe B (2007) The ductal stretching technique: an endoscopic-assisted technique for removal of submandibular stones. Laryngoscope 117(6):1031–1035
Angiero F, Benedicenti S, Romanos GE, Crippa R (2008) Sialolithiasis of the submandibular salivary gland treated with the 810- to 830-nm diode laser. Photomed Laser Surg 26(6):517–521
Lafont J, Graillon N, Hadj Saïd> M, Tardivo D, Foletti JM, Chossegros C (2018) Extracorporeal lithotripsy of salivary gland stone: a 55 patients study. J Stomatol Oral Maxillofac Surg 119(5):375–378
Kopec T et al (2013) Algorithm changes in treatment of submandibular gland sialolithiasis. Eur Arch Otorhinolaryngol 270(7):2089–2093
Makdissi J et al (2004) Glandular function after intraoral removal of salivary calculi from the hilum of the submandibular gland. Br J Oral Maxillofac Surg 42(6):538–541
Marchal F, Becker M, Kurt AM, Oedman M, Dulguerov P, Lehmann W (2001) Histopathology of submandibular glands removed for sialolithiasis. Ann Otol Rhinol Laryngol 110(5 Pt 1):464–469
McGurk M, Makdissi J, Brown JE (2004) Intra-oral removal of stones from the hilum of the submandibular gland: report of technique and morbidity. Int J Oral Maxillofac Surg 33(7):683–686
Eun YG, Chung DH, Kwon KH (2010) Advantages of intraoral removal over submandibular gland resection for proximal submandibular stones: a prospective randomized study. Laryngoscope 120(11):2189–2192
Schapher M, Mantsopoulos K, Messbacher ME, Iro H, Koch M (2017) Transoral submandibulotomy for deep hilar submandibular gland sialolithiasis. Laryngoscope 127:2038–2044
Moreland LW (2004) Schirmer’s tear test, in Rheumatology and Immunology Therapy. Springer, Berlin, Heidelberg, pp 781–782
Schwarz D, Kabbasch C, Scheer M, Mikolajczak S, Beutner D, Luers JC (2015) Comparative analysis of sialendoscopy, sonography, and CBCT in the detection of sialolithiasis. Laryngoscope 125(5):1098–1101
Koch M et al (2017) Multimodal treatment in difficult sialolithiasis: role of extracorporeal shock-wave lithotripsy and intraductal pneumatic lithotripsy. Laryngoscope 128(10):E332–E338
Koch M, Zenk J, Iro H (2009) Algorithms for treatment of salivary gland obstructions. Otolaryngol Clin N Am 42(6):1173–1192 Table of Contents
Capaccio P, Bottero A, Pompilio M, Ottaviani F (2005) Conservative transoral removal of hilar submandibular salivary calculi. Laryngoscope 115(4):750–752
Bates D, O’Brien CJ, Tikaram K, Painter DM (1998) Parotid and submandibular sialadenitis treated by salivary gland excision. Aust N Z J Surg 68(2):120–124
Kennedy PJ, Poole AG (1989) Excision of the submandibular gland: minimizing the risk of nerve damage. Aust N Z J Surg 59(5):411–414
Winkel R et al (2000) Surgical results of submandibular gland excision. Ugeskr Laeger 162(40):5354–5357
Hald J, Andreassen UK (1994) Submandibular gland excision: short- and long-term complications. ORL J Otorhinolaryngol Relat Spec 56(2):87–91
Kukuckova B, Svec M (2011) Surgical management of submandibulary gland diseases: ten years of experience. Bratisl Lek Listy 112(5):264–268
Jokela J, Haapaniemi A, Mäkitie A, Saarinen R (2017) Sialendoscopy under local anaesthesia. Acta Otolaryngol 137(3):310–314
Koch M, Künzel J, Iro H, Psychogios G, Zenk J (2014) Long-term results and subjective outcome after gland-preserving treatment in parotid duct stenosis. Laryngoscope 124(8):1813–1818
Nahlieli O, Baruchin AM (2000) Long-term experience with endoscopic diagnosis and treatment of salivary gland inflammatory diseases. Laryngoscope 110(6):988–993
Nahlieli O et al (2001) Diagnosis and treatment of strictures and kinks in salivary gland ducts. J Oral Maxillofac Surg 59(5):484–490 discussion, 490–2
Nahlieli O (2015) Complications of sialendoscopy: personal experience, literature analysis, and suggestions. J Oral Maxillofac Surg 73(1):75–80
Kim JK, Park JS (2007) Ultrasound-guided transoral removal of impalpable hilar submandibular salivary stones. Laryngoscope 117(8):1373–1375
Ardekian L, Klein HH, Araydy S, Marchal F (2014) The use of sialendoscopy for the treatment of multiple salivary gland stones. J Oral Maxillofac Surg 72(1):89–95
Zhang L, Escudier M, Brown J, Capaccio P, Pignataro L, McGurk M (2010) Long-term outcome after intraoral removal of large submandibular gland calculi. Laryngoscope 120(5):964–966
Roh JL, Park CI (2008) Transoral removal of submandibular hilar stone and sialodochoplasty. Otolaryngol Head Neck Surg 139(2):235–239
Author information
Authors and Affiliations
Contributions
CS and JL worked out the concept and wrote the manuscript. JL carried out the follow-up examinations. JL and CS conducted follow-up sonographies. CS, CN, and DS carried out the operational procedures. JL assisted the operations. NK, HH, MR, and CN gave critical scientific input for the study design and engaged in manuscript creation.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethics approval was granted by the Ethics Committee of the Heinrich-Heine-University of Düsseldorf and given the reference number 5586.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients gave their written consent to take part in the study. The forms can be obtained from the corresponding author in German language..
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sproll, C., Naujoks, C., Holtmann, H. et al. Removal of stones from the superficial lobe of the submandibular gland (SMG) via an intraoral endoscopy-assisted sialolithotomy. Clin Oral Invest 23, 4145–4156 (2019). https://doi.org/10.1007/s00784-019-02853-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02853-9