Abstract
Background
Surgical repair is recommended for all children with inguinal hernia due to fear of incarceration. The aim of this study was to assess the risk of incarceration and strangulation of inguinal hernias in children treated with delayed surgery or no surgery.
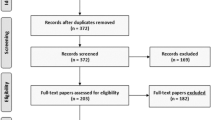
Methods
Systematic searches were conducted in three databases. We included studies reporting on children with inguinal hernia, with the majority ≤ 10 years old. The interventions were non-acute inguinal hernia surgery or no surgery. The main outcomes were incarceration and strangulation. Secondary outcomes were postoperative complications. Randomized controlled trials, non-randomized controlled trials, and observational studies were included.
Results
We included 22 studies with 14,959 children. All studies reported on elective repairs. None of the studies specifically reported on watchful waiting. Of the studies reporting wait time as mean or median, the median wait time was 46 days (range 1–552). The crude incarceration rate across the included studies was 7% for all children and 11% for preterm children. The testicular atrophy rate was 1% and the recurrence rate was 1%.
Conclusions
The risk of incarceration in children awaiting inguinal hernia surgery is substantial. In general, we cannot support delaying surgery unnecessarily. However, there may be benefits of delaying surgery in individual cases. In such cases, the surgeon should assess if the benefits may overrule the risk of incarceration.

Similar content being viewed by others
References
Somme S, Bronsert M, Morrato E, Ziegler M (2013) Frequency and variety of inpatient pediatric surgical procedures in the United States. Pediatrics 132:1466–1472. https://doi.org/10.1542/peds.2013-1243
Chang S, Chen J, Hsu C, Chuang F, Yang S (2016) The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia 20:559–563. https://doi.org/10.1007/s10029-015-1450-x
Burcharth J, Pedersen M, Bisgaard T, Pedersen C, Rosenberg J (2013) Nationwide prevalence of groin hernia repair. PLoS One 8:e54367. https://doi.org/10.1371/journal.pone.0054367
International Pediatric Endosurgery Group (2010) IPEG guidelines for inguinal hernia and hydrocele. J Laparoendosc Adv Surg Tech 20:10–14. https://doi.org/10.1089/lap.2010.9998
Ein SH, Njere I, Ein A (2006) Six thousand three hundred sixty-one pediatric inguinal hernias: a 35-year review. J Pediatr Surg 41:980–986. https://doi.org/10.1016/j.jpedsurg.2006.01.020
Bronsther B, Abrams MW, Elboim C (1972) Inguinal hernias in children—a study of 1,000 cases and a review of the literature. J Am Med Womens Assoc 27:522–525
Watson DS, Sharp KW, Vasquez JM, Richards WO (1994) Incidence of inguinal hernias diagnosed during laparoscopy. South Med J 87:23–25
Weaver KL, Poola AS, Gould JL, Sharp SW, St. Peter SD, Holcomb GW (2017) The risk of developing a symptomatic inguinal hernia in children with an asymptomatic patent processus vaginalis. J Pediatr Surg 52:60–64. https://doi.org/10.1016/j.jpedsurg.2016.10.018
Centeno-Wolf N, Mircea L, Sanchez O, Genin B, Lironi A, Chardot C, Birraux J, Wildhaber BE (2015) Long-term outcome of children with patent processus vaginalis incidentally diagnosed by laparoscopy. J Pediatr Surg 50:1898–1902. https://doi.org/10.1016/j.jpedsurg.2015.07.001
Öberg S, Andresen K, Rosenberg J (2017) Etiology of inguinal hernias: a comprehensive review. Front Surg 4:52. https://doi.org/10.3389/fsurg.2017.00052
Skandalakis J, Colborn G, Androulakis J, Skandalakis L, Pemberton L (1993) Embryologic and anatomic basis of inguinal herniorrhaphy. Surg Clin N Am 73:799–836
Fitzgibbons RJ, Giobbie-Hurder A, Gibbs JO, Dunlop DD, Reda DJ, McCarthy M, Neumayer LA, Barkun JST, Hoehn JL, Murphy JT, Sarosi GA, Syme WC, Thompson JS, Wang J, Jonasson O (2006) Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA 295:285–292. https://doi.org/10.1001/jama.295.3.285
The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Gong W, Li J (2018) Operation versus watchful waiting in asymptomatic or minimally symptomatic inguinal hernias: the meta-analysis results of randomized controlled trials. Int J Surg 52:120–125. https://doi.org/10.1016/j.ijsu.2018.02.030
Rosenberg J (2008) Pediatric inguinal hernia repair—a critical appraisal. Hernia 12:113–115. https://doi.org/10.1007/s10029-007-0316-2
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Higgins J, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Cochrane Collab. http://handbook.cochrane.org/. Accessed 3 May 2018
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 3 May 2018
Skoog S, Conlin M (1995) Pediatric hernias and hydroceles. The urologist’s perspective. Urol Clin N Am 22:119–130
Hirabayashi T, Ueno S, Hirakawa H, Tei E, Mori M (2017) Surgical treatment of inguinal hernia with prolapsed ovary in young girls: emergency surgery or elective surgery. Tokai J Exp Clin Med 42:89–95
Ellison JS, Shnorhavorian M, Merguerian PA, Grady R (2016) Impact of concomitant hernia repair at the time of complete primary repair of bladder exstrophy. J Pediatr Urol 12:211.e1–211.e5. https://doi.org/10.1016/j.jpurol.2016.04.028
Crankson S, Al Tawil K, Al Namshan M, Baylon B, Gieballa M, Al Jadaan S, Ahmed I (2015) Management of inguinal hernia in premature infants: 10-year experience. J Indian Assoc Pediatr Surg 20:21–24. https://doi.org/10.4103/0971-9261.145440
Chan IHY, Lau CT, Chung PHY, Chan KL, Lan LCL, Wong KKY, Tam PKH (2013) Laparoscopic inguinal hernia repair in premature neonates: is it safe? Pediatr Surg Int 29:327–330. https://doi.org/10.1007/s00383-012-3240-1
Old O, Rogers T (2012) Restructuring services to reduce waiting times and prevent complications: neonatal inguinal hernias at Bristol Children’s Hospital. Clin Gov 17:39–44. https://doi.org/10.1108/14777271211200738
Nah SA, Giacomello L, Eaton S, de Coppi P, Curry JI, Drake DP, Kiely EM, Pierro A (2011) Surgical repair of incarcerated inguinal hernia in children: laparoscopic or open? Eur J Pediatr Surg 21:8–11. https://doi.org/10.1055/s-0030-1262793
Chen LE, Zamakhshary M, Foglia RP, Coplen DE, Langer JC (2009) Impact of wait time on outcome for inguinal hernia repair in infants. Pediatr Surg Int 25:223–227. https://doi.org/10.1007/s00383-008-2306-6
Koivusalo A, Pakarinen MP, Rintala RJ (2007) Laparoscopic herniorrhaphy after manual reduction of incarcerated inguinal hernia. Surg Endosc 21:2147–2149. https://doi.org/10.1007/s00464-007-9318-5
Gahukamble DB, Khamage AS (1996) Early versus delayed repair of reduced incarcerated inguinal hernias in the pediatric population. J Pediatr Surg 31:1218–1220
Gyrtrup HJ, Mejdahl S, Kvist E, Skeie E (1990) Emergency presentation of inguinal hernia in childhood—treatment strategy. A follow-up study. Ann Chir Gynaecol 79:97–100
Puri P, Guiney EJ, O’Donnell B (1984) Inguinal hernia in infants: the fate of the testis following incarceration. J Pediatr Surg 19:44–46
Sulkowski JP, Cooper JN, Duggan EM, Balci O, Anandalwar SP, Blakely ML, Heiss K, Rangel S, Minneci PC, Deans KJ (2015) Does timing of neonatal inguinal hernia repair affect outcomes? J Pediatr Surg 50:171–176. https://doi.org/10.1016/j.jpedsurg.2014.10.035
Takahashi A, Toki F, Yamamoto H, Otake S, Oki Y, Kuwano H (2012) Outcomes of herniotomy in premature infants: recent 10 year experience. Pediatr Int 54:491–495. https://doi.org/10.1111/j.1442-200X.2012.03607.x
Vaos G, Gardikis S, Kambouri K, Sigalas I, Kourakis G, Petoussis G (2010) Optimal timing for repair of an inguinal hernia in premature infants. Pediatr Surg Int 26:379–385. https://doi.org/10.1007/s00383-010-2573-x
González Santacruz M, Mira Navarro J, Encinas Goenechea A, García Ceballos A, Sánchez Zaplana H, Jiménez Cobo B (2004) Low prevalence of complications of delayed herniotomy in the extremely premature infant. Acta Paediatr 93:94–98
Uemura S, Woodward AA, Amerena R, Drew J (1999) Early repair of inguinal hernia in premature babies. Pediatr Surg Int 15:36–39. https://doi.org/10.1007/s003830050507
Chang S-J, Chen JY-C, Hsu C-K, Chuang F-C, Yang SS-D (2016) The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia 20:559–563. https://doi.org/10.1007/s10029-015-1450-x
Kurobe M, Baba Y, Otsuka M (2016) Inguinal hernia in very low-birthweight infants: follow up to adolescence. Pediatr Int 58:1322–1327. https://doi.org/10.1111/ped.13060
de Goede B, Verhelst J, van Kempen BJ, Baartmans MG, Langeveld HR, Halm JA, Kazemier G, Lange JF, Wijnen RMH (2015) Very low birth weight is an independent risk factor for emergency surgery in premature infants with inguinal hernia. J Am Coll Surg 220:347–352. https://doi.org/10.1016/j.jamcollsurg.2014.11.023
Lautz TB, Raval MV, Reynolds M (2011) Does timing matter? A national perspective on the risk of incarceration in premature neonates with inguinal hernia. J Pediatr 158:573–577. https://doi.org/10.1016/j.jpeds.2010.09.047
Lee SL, Gleason JM, Sydorak RM (2011) A critical review of premature infants with inguinal hernias: optimal timing of repair, incarceration risk, and postoperative apnea. J Pediatr Surg 46:217–220. https://doi.org/10.1016/j.jpedsurg.2010.09.094
Seo S, Takahashi T, Marusasa T, Kusafuka J, Koga H, Halibieke A, Lane GJ, Okazaki T, Yamataka A (2012) Management of inguinal hernia in children can be enhanced by closer follow-up by consultant pediatric surgeons. Pediatr Surg Int 28:33–36. https://doi.org/10.1007/s00383-011-3005-2
Gholoum S, Baird R, Laberge J-M, Puligandla PS (2010) Incarceration rates in pediatric inguinal hernia: do not trust the coding. J Pediatr Surg 45:1007–1011. https://doi.org/10.1016/j.jpedsurg.2010.02.033
Turial S, Enders J, Krause K (2010) Laparoscopic inguinal herniorrhaphy in premature infants. Eur J Pediatr Surg 20:371–374. https://doi.org/10.1055/s-0030-1261932
Zamakhshary M, To T, Guan J, Langer JC (2008) Risk of incarceration of inguinal hernia among infants and young children awaiting elective surgery. CMAJ 179:1001–1005. https://doi.org/10.1503/cmaj.070923
Koivusalo AI, Korpela R, Wirtavuori K, Piiparinen S, Rintala RJ, Pakarinen MP (2009) A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics 123:332–337. https://doi.org/10.1542/peds.2007-3752
Niedzielski J, Król R, Gawłowska A (2003) Could incarceration of inguinal hernia in children be prevented? Med Sci Monit 9:16–18
Stephens BJ, Rice WT, Koucky CJ, Gruenberg JC (1992) Optimal timing of elective indirect inguinal hernia repair in healthy children: clinical considerations for improved outcome. World J Surg 16:952–957
Stylianos S, Jacir NN, Harris BH (1993) Incarceration of inguinal hernia in infants prior to elective repair. J Pediatr Surg 28:582–583
Habre W, Disma N, Virag K, Becke K, Hansen TG, Johr M, Leva B, Morton NS, Vermeulen PM, Zielinska M, Boda K, Veyckemans F (2017) Incidence of severe critical events in paediatric anaesthesia (APRICOT): a prospective multicentre observational study in 261 hospitals in Europe. Lancet Respir Med 5:412–425. https://doi.org/10.1016/S2213-2600(17)30116-9
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This study received no financial support from extramural sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Olesen reports no potential conflicts of interest. Mortensen reports no potential conflicts of interest. Öberg reports no potential conflicts of interest. Rosenberg reports personal fees from Bard and Merck, outside the submitted work.
Ethical standards
This kind of study does not need ethical approval.
Human and animal rights
This article does not contain any studies directly involving human participants, as it is a review of data already collected in a hernia database.
Informed consent
For this type of study informed consent was not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Olesen, C.S., Mortensen, L.Q., Öberg, S. et al. Risk of incarceration in children with inguinal hernia: a systematic review. Hernia 23, 245–254 (2019). https://doi.org/10.1007/s10029-019-01877-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-019-01877-0