Abstract
Background
Elderly patients (EPs) suffering from retroperitoneal rhabdomyosarcoma (RRMS) carry a considerably poorer prognosis compared to younger patients (YPs). We hypothesized that EPs received less aggressive and comprehensive treatment than YPs, resulting in poorer survival outcomes.
Materials and methods
All patients diagnosed with RRMS since 1998 in the National Cancer Data Base (NCDB) were reviewed for patient demographics, tumor characteristics, treatment modalities and survival outcomes.
Results
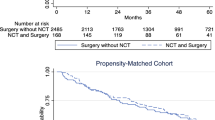
Of the 100 patients identified, 35 % were ≥65 years of age. EPs (aged ≥65 years), when compared to YPs (aged <65), were less likely to receive systemic chemotherapy (20 % EPs vs 71 % YPs, p < 0.001) and treatment at an academic center (34 % EPs vs 60 % YPs, p = 0.05), although the frequency of radiation (23 % EPs vs 31 % YPs, p = 0.40) and radical surgery (26 % EPs vs 22 % YPs, p = 0.55) were similar. EPs received treatment more frequently at comprehensive community cancer programs (57 %) and had a shorter median distance of travel for care (6.4 vs 13 miles, p = 0.009). After adjusting for gender and tumor size, EPs had a hazard ratio of 3.6 (95 % CI 1.8–7.2, p < 0.001), with a median survival of 2 months (interquartile range [IQR] 1–8 months) versus 17 months for YPs (IQR 8–43 months).
Conclusion
Altered practice patterns exist for EPs and include reduced use of systemic chemotherapy which may contribute to poorer outcomes for RRMS patients. Although regionalization of care poses challenges, this may offer benefit to the EP group.

Similar content being viewed by others
References
Ries LAG, Smith MA, Gurney JG, Linet M, Tamra T, Young JL, Bunin GR (1999) Cancer incidence and survival among children and adolescents: USA SEER program 1975-1995. National Cancer Institute, SEER Program. NIH Pub, Bethesda
Ferrari A, Dileo P, Casanova M, Bertulli R, Meazza C, Gandola L, Navarria P, Collini P, Gronchi A, Olmi P, Fossati-Bellani F, Casali PG (2003) Rhabdomyosarcoma in adults. A retrospective analysis of 171 patients treated at a single institution. Cancer 98(3):571–580. doi:10.1002/cncr.11550
Sultan I, Qaddoumi I, Yaser S, Rodriguez-Galindo C, Ferrari A (2009) Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973–2005: an analysis of 2600 patients. J Clin Oncol 27(20):3391–3397. doi:10.1200/JCO.2008.19.7483
Raney RB, Maurer HM, Anderson JR, Andrassy RJ, Donaldson SS, Qualman SJ, Wharam MD, Wiener ES, Crist WM, The Intergroup Rhabdomyosarcoma Study Group (IRSG) (2001) Major lessons from the IRS-I through IRS-IV studies as background for the current IRS-V treatment protocols. Sarcoma 5(1):9–15. doi:10.1080/13577140120048890
Dumont SN, Lazar AJ, Bridge JA, Benjamin RS, Trent JC (2012) PAX3/7-FOXO1 fusion status in older rhabdomyosarcoma patient population by fluorescent in situ hybridization. J Cancer Res Clin Oncol 138(2):213–220. doi:10.1007/s00432-011-1089-7
Dumont SN, Araujo DM, Munsell MF, Salganick JA, Dumont AG, Raymond KA, Linassier C, Patel S, Benjamin RS, Trent JC (2013) Management and outcome of 239 adolescent and adult rhabdomyosarcoma patients. Cancer Med 2(4):553–563. doi:10.1002/cam4.92
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 40(5):373–383
Gutierrez JC, Perez EA, Moffat FL, Livingstone AS, Franceschi D, Koniaris LG (2007) Should soft tissue sarcomas be treated at high-volume centers? An analysis of 4205 patients. Ann Surg 245(6):952–958. doi:10.1097/01.sla.0000250438.04393.a8
Rossi CR, Vecchiato A, Mastrangelo G, Montesco MC, Russano F, Mocellin S, Pasquali S, Scarzello G, Basso U, Frasson A, Pilati P, Nitti D, Lurkin A, Ray-Coquard I (2013) Adherence to treatment guidelines for primary sarcomas affects patient survival: a side study of the European connective tissue cancer network (CONTICANET). Ann Oncol 24(6):1685–1691. doi:10.1093/annonc/mdt031
Kojima Y, Hashimoto K, Ando M, Yonemori K, Hirakawa A, Kodaira M, Yunokawa M, Shimizu C, Tamura K, Katsumata N, Hosono A, Makimoto A, Fujiwara Y (2012) Clinical outcomes of adult and childhood rhabdomyosarcoma treated with vincristine, d-actinomycin, and cyclophosphamide chemotherapy. J Cancer Res Clin Oncol 138(7):1249–1257. doi:10.1007/s00432-012-1199-x
Wu Y, Li C, Zhong Y, Guo W, Ren G (2014) Head and neck rhabdomyosarcoma in adults. J Craniofac Surg 25(3):922–925. doi:10.1097/SCS.0000000000000704
Donaldson SS (1985) The value of adjuvant chemotherapy in the management of sarcomas in children. Cancer 55(9 Suppl):2184–2197
Rehman S, Crane A, Din R, Raza SJ, Shi Y, Wilding G, Levine EG, George S, Pili R, Trump DL, Guru KA (2013) Understanding avoidance, refusal, and abandonment of chemotherapy before and after cystectomy for bladder cancer. Urology 82(6):1370–1375. doi:10.1016/j.urology.2013.07.055
Aizer AA, Chen MH, Parekh A, Choueiri TK, Hoffman KE, Kim SP, Martin NE, Hu JC, Trinh QD, Nguyen PL (2014) Refusal of curative radiation therapy and surgery among patients with cancer. Int J Radiat Oncol 89(4):756–764. doi:10.1016/j.ijrobp.2014.03.024
Acknowledgments
This research was funded by the Wadina Sarcoma Research Fund. The NCDB is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society. The data used in the study are derived from a de-identified NCDB file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed, or the conclusions drawn from these data by the investigator.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JC received research funding from Threshold and CytRx. KT received honoraria from Caris Biosciences and Ethicon and is the Sharon K. Wadina Chair in Sarcoma Research.
About this article
Cite this article
Kashtan, M.A., Jayakrishnan, T.T., Rajeev, R. et al. Age-based disparities in treatment and outcomes of retroperitoneal rhabdomyosarcoma. Int J Clin Oncol 21, 602–608 (2016). https://doi.org/10.1007/s10147-015-0918-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-015-0918-0