Abstract
Biologic treatment withdrawal in inflammatory bowel disease patients with prolonged remission may lead to benefits but also increases the risk of getting a relapse. The risk of relapse after biologic withdrawal according to the Dutch STOP-criteria is still unknown. The aim of this study was to compare the cumulative incidence of relapse in inflammatory bowel disease patients that discontinued biologic therapy after applying the STOP-criteria with patients who maintained biologic therapy. We performed a mono-centre, observational, retrospective study by evaluating relapse risk of patients treated with biologic agents who discontinued this treatment according to the STOP-criteria (STOP-group) compared to patients who were in remission for more than 3 years before withdrawal (LATERSTOP-group) and patients who continued their biologic (MAINTAIN-group). The cumulative risk was calculated at 12 and 36 months using the log-rank test to compare Kaplan–Meier curves. Eighty-three of 398 patients that used biologics between 1 January 2010 and 1 January 2020 were included. The cumulative relapse incidences in the STOP-group and the LATERSTOP-group were, respectively, 29% and 42% at 12 months and 47% versus 58% at 36 months. Patients in the MAINTAIN-group showed a lower (p = 0.03) cumulative relapse incidence of 10% at 12 months and 18% at 36 months. Patients who discontinued their biologic therapy according to the STOP-criteria had significantly more relapses at 12 and 36 months than patients who maintained biologic treatment.
Similar content being viewed by others
Introduction
Inflammatory bowel disease (IBD), including Crohn’s disease (CD), ulcerative colitis (UC) and IBD-unspecified (IBD-U), refers to conditions which are characterized by chronic inflammation of the gastrointestinal tract. Since 2001, biologic therapy has been registered for patients with moderate to severe IBD. Biologics are immunosuppressant agents which are effective in both inducing and maintaining remission [1,2,3]. However, the use of biologics may lead to potential serious side effects [4,5,6,7]. Furthermore, biologics have a substantial impact on healthcare costs [8]. On the other hand, biologics withdrawal may lead to relapse of disease activity with unfavourable effects on patients’ quality of life, ability to work and possible hospitalization, which also results in higher costs. Consensus on the timing of discontinuation of biologics is lacking.
Until recently, a wide range of relapse rates from 19 to 41% after the first year of discontinuation was reported [9,10,11]. Furthermore, concerns about the possible decrease in effectiveness after reintroduction of biologics in case of a relapse have risen [12].
In 2018, the European Crohn’s and Colitis Organisation (ECCO) presented considerations regarding the timing of biologics withdrawal [13]. Furthermore, in 2009, the Dutch national research group named Initiative on Crohn’s and Colitis (ICC) suggested to stop biologic therapy when certain criteria were met [14]. These STOP-criteria stated that discontinuation of biologic therapy may be considered in case of prolonged remission. The decision should be based on objectified clinical remission and also on the wish of both the patient and treating physician to discontinue the therapy. However, up to now, no data have been published on the relapse risk after applying these ICC STOP-criteria.
Therefore, the aim of this study was to compare the cumulative incidence of relapse in IBD patients that discontinued biologic therapy after applying the ICC STOP-criteria with patients who maintained biologic therapy.
Methods
Study design and setting
This mono-centre, observational, retrospective cohort study was conducted in Catharina Hospital Eindhoven (CHE), which is a teaching hospital in the Netherlands.
Study population
The study population comprised adult IBD patients from the CHE IBD cohort (previously described by Gilissen et al. [14]) treated with a biologic agent between 1 January 2010 and 1 January 2020. Biologic therapy consisted of one of the following agents: infliximab, adalimumab, golimumab, vedolizumab or ustekinumab. Patients were included in the study in one of three different groups based on the duration of biologic treatment: the STOP-group, the LATERSTOP-group and the MAINTAIN-group.
Patients were included in the STOP-group if biologic therapy was discontinued after 2–3 years of remission according to the STOP-criteria. Patients were included in the LATERSTOP-group if their IBD had been in remission with biologic therapy for a consecutive period of more than 3 years at the time of discontinuation. Patients were included in the MAINTAIN-group if their IBD had been in remission with biologic therapy for 3 years and this therapy was maintained after this period. All patients from these three groups complied with a follow-up of at least 1 year after discontinuation or prolonged biologic therapy.
In the Netherlands, biologic therapy is always registered and supplied by the Department of Pharmacy and Clinical Pharmacology in the hospital. Therefore, no patients were missed in the screening for eligibility.
Outcomes and definitions
The primary outcome was to assess the cumulative incidence of relapse after discontinuation of biologic therapy, compared to patients who continued their biologic agent. The STOP-criteria were applied as defined by the ICC: discontinuation of biologic therapy was considered after a period of prolonged clinical remission for at least 2 to 3 years, the physician as well as the patient should support the decision to stop, patients were informed about the potential consequences of discontinuation, and after withdrawal, a watchful waiting strategy was guaranteed [15]. In the current study, clinical remission was defined by the physician’s global assessment (PGA). The PGA is an element of the partial Mayo score and classifies IBD activity in four levels as either remission, partial remission (mild disease), moderate or severe activity. This assessment acknowledges the record of abdominal discomfort and functional assessment, but also other observations such as physical, biochemical, radiological, endoscopic and histologic findings are taken into account [16]. Furthermore, relapse was defined as clinical, biochemical, and/or endoscopic disease activity that required a medical intervention, such as hospitalization, administering oral or intravenous corticosteroids, immunotherapy (e.g. immunomodulator, methotrexate or restart or use of another biologic agent) or surgery.
Data collection
Data from patients eligible for inclusion were distracted from the electronical medical records. For each patient, demographic, clinical, endoscopic, radiological and histological data were collected at time of diagnosis and before discontinuing biologic therapy. Additionally, in the case of a relapse, data was collected. When a relapse occurred, time from discontinuation until relapse was expressed in months. Maximum follow-up in this study was 3 years after discontinuation or maintaining therapy.
Statistical analysis
All data were managed and analysed using IBM® SPSS® Statistics for Windows version 25.0., Armonk, New York. Depending on the normality of their distribution, quantitative variables were summarized by either a mean and standard deviation (SD) or the median with an interquartile range. Comparisons between numeric variables were performed using the t-test for independent samples. Comparisons between categorical variables were performed using the Chi-square test and the Fisher’s exact test, depending on the distribution of data. Statistical significance was set at p < 0.05. To analyse the primary outcome, a Kaplan–Meier analysis was conducted. The cumulative risk was calculated at 12 and 36 months after discontinuation of biologic therapy. Kaplan–Meier curves were compared using the log-rank test for assessing the impact of several variables, e.g. disease type, gender, years of remission before discontinuation.
Due to the large variety in relapse risk rates that were previously published, our power analysis showed a wide range of 42 to 398 patients which should be included to reach statistical power for the current study.
Ethical aspects
The study was approved by the Medical Ethical Committee United (MEC-U), reference number W21.067. This study was performed in line with the principles of the Declaration of Helsinki. Due to the retrospective study design and the fact that only anonymous data were collected, no patients’ informed consent was required.
Results
Study population
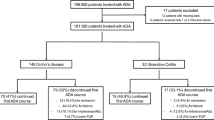
According to the Department of Pharmacy and Clinical Pharmacology, 389 patients had been treated with biologic therapy between 1 January 2010 and 1 January 2020. Of these 398 patients, 35 patients were excluded because they used biologics for less than 2 years. Another 102 patients were excluded because biologics were discontinued due to different reasons than appliance of the STOP-criteria (e.g. pregnancy, therapy failure or death). Finally, 145 patients were excluded because they did not met the criteria of prolonged remission for at least 2 years. Of the remaining 116 patients eligible for the study, 33 were excluded due to incomplete follow-up. Thus, eventually 83 patients were included in the analysis (Fig. 1).
The baseline characteristics of the study population are summarized in Table 1. The majority of patients (68.7%) was treated with biologic therapy for Crohn’s disease. The ratio of male and female patients was balanced. The majority of patients had no extraintestinal manifestations.
Before treatment with biologics, all patients were treated with other IBD medication. The majority of patients had used 5-aminosalicylic acid (5-ASA) preparations (61.4%), thiopurines (86.7%) and/or oral corticosteroids (65.1%).
The most commonly used biologics to achieve and maintain remission were TNF alpha inhibitors (anti-TNF). Of all 80 patients that were treated with anti-TNF, the majority achieved remission with infliximab (61.5%), followed by adalimumab (33.7%) and golimumab (1.2%). Most patients (74.7%) achieved remission on the first biologic treatment. A minority of patients (21.7%) did not reach remission with their first anti-TNF agent but with another anti-TNF agent. Only three patients (3.6%) did not achieve and maintain remission when treated with anti-TNF. However, they did reach and maintain remission when treated with vedolizumab. In the current study, no patients used ustekinumab or januskinase (JAK)-inhibitors.
Before discontinuation of the biologic therapy, fourteen patients (50.0%) in the STOP-group and fifteen patients (62.5%) in the LATERSTOP-group underwent a colonoscopy. All of these patients showed endoscopic remission. Biopsies were taken in three (21.4%) of the performed colonoscopies in the STOP-group and in five (21.0%) of the performed colonoscopies in the LATERSTOP-group. All biopsies showed histological remission. Following withdrawal of the biologic therapy, 46.4% of the STOP-population was treated with thiopurines versus 25.0% of the LATERSTOP-group.
Disease evolution after withdrawal versus maintaining biologic therapy
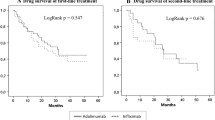
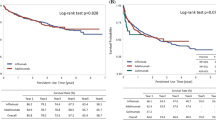
Patients in the STOP-group showed a significantly higher relapse rate compared to patients in the MAINTAIN-group (p value 0.034), as shown in Fig. 2. During the study period of 36 months, 57% of the patients in the STOP-group experienced a relapse. The mean time between withdrawal and the occurrence of a relapse was 25 months (95% CI [19, 30]).
Patients in the LATERSTOP-group also showed a statistically significant higher relapse rate compared to patients in the MAINTAIN-group (p = 0.002). In the LATERSTOP-group, 54.0% of the patients experienced a relapse within 36 months with occurrence of this relapse at a mean time of 22 months (95% CI [16, 28]).
In the MAINTAIN-group, 16% of the patients experienced a relapse within 36 months after prolonged remission of 3 years during biologic treatment. These relapses occurred at a mean time of 31 months after reaching 3 years of prolonged remission (95% CI [28, 35]).
No statistical differences in relapse rates were seen between the STOP-group and the LATERSTOP-group (p = 0.34).
Calculated cumulative incidence
The cumulative risk of getting a relapse was calculated at 12 and 36 months for the different groups.
In the STOP-group, the risk was 29% and 47%, respectively. In the LATERSTOP-group, we found incidence rates of 42% at 12 months and 58% at 36 months. In the MAINTAIN-group, the calculation showed a cumulative incidence of 10% and 18% at 12 and 36 months respectively.
Relapse characteristics
The characteristics of all patients who experienced a relapse are summarized in Table 2. Between the three different study groups, no statistical significant differences in clinical characteristics were seen (e.g. IBD classification, consequences of relapse, reintroduction or switch of biologic agent after relapse and remission after either reintroduction or switch of biologic therapy). Furthermore, within the STOP-group, no statistically significant differences in relevant clinical factors were seen between patients with maintained remission versus relapse: classification of IBD (p = 0.84), duration of remission under biologic therapy before withdrawal (p = 0.71) and use of immunomodulators (IMM) (p = 0.11).
When experienced a relapse after withdrawal of biologic therapy, the vast majority of patients in both the STOP-group (83.3%) and LATERSTOP-group (92.3%) were again treated with a biologic agent. Clinical remission was achieved again after reintroduction of a biologic in 75% of the patients in the STOP-group and 69% of the patients in the LATERSTOP-group.
Discussion
This mono-centre retrospective study aimed to compare the cumulative incidence of relapse between patients that discontinued biologic therapy after applying the STOP-criteria (STOP-group) and those who maintained their biologic agent (MAINTAIN-group). Our study shows that the STOP-group had significantly more relapses after 1 and 3 years of follow-up than the MAINTAIN-group. Notably, a third group of patients that had prolonged remission for more than 3 years before biologics were discontinued (LATERSTOP-group), also showed high cumulative release rates. No significant differences were found between the baseline characteristics of the three different groups, e.g. disease type, Montreal classification, type of biologic agent and use of immunomodulators. Furthermore, no differences in relevant clinical factors were found between patients who relapsed versus patients who maintained remission within each group.
Our findings are in line with expert opinions stating that relapses often occur after discontinuation of biologic therapy [9]. The cumulative relapse risk of 29% at 12 months accords with previously found incidences [9,10,11, 17,18,19,20,21,22,23,24], although some studies report higher incidences of up to almost 50% after 1 year [25,26,27,28,29,30,31]. The higher relapse risk of 47% at 36 months is also in line with previous studies [9].
However, to our knowledge, no studies have investigated the cumulative incidence of relapse after discontinuation of biologic therapy specifically according to the STOP-criteria. These criteria, which were formulated before less expensive biosimilars were available, seem to be more economically and not scientifically driven. Prior to our study, cumulative incidence rates have been evaluated with different criteria for stopping biologic therapy. There is a substantial heterogeneity among these studies. The majority of these studies examined relapse rates in patients with clinical remission [9, 10, 17, 18, 20, 25,26,27]. However, the applied definitions of clinical remission vary strongly. Some studies assessed clinical remission using scoring lists (e.g. Crohn’s Disease Activity Index (CDAI), Harvey-Bradshaw Index (HBI) or Mayo score), whereas others used biologic markers or endoscopy to define remission [10, 20, 23, 25,26,27]. Only a few studies described a combination of clinical, biochemical, endoscopic and/or histological factors [11, 19, 23, 30, 31].
The findings of our study may suggest that biologics should be continued, even after prolonged remission, in order to ensure the smallest risk of getting a relapse. Nevertheless, some other considerations should be taken into account when discussing discontinuation versus maintaining biologic therapy. For instance, the high costs of maintained biologic agents, hospital visits for infusions and outpatient clinic consultations including laboratory tests are important to bear in mind. A recently published model shows that continuation of anti-TNF in patients with remission is not cost-effective compared with withdrawal [32].
Furthermore, maintained biologic therapy may cause a burden for patients considering time spent on infusions, resulting in absenteeism from work, school and/or social events. A drug free period may be of high value for individual patients and may lower the costs of medication and healthcare providers. Considering all these factors, it cannot be stated on beforehand that one of both strategies (discontinuation versus maintaining biologic therapy) is superior. Therefore, we believe biologic discontinuation after prolonged remission should be discussed with each individual patient and all pros and cons (including the relapse risk) should be mentioned.
Our study also shows that prolonged remission for more than 3 years before treatment withdrawal seems to have no superiority compared with remission of 2 to 3 years. These effects together with cost effectiveness and patient value should be studied in future research using a comparative and prospective design. Accordingly, future studies should focus on the identification of (clinical) factors associated with the risk of a relapse.
The limitation of this study lies in the retrospective mono-centre study design. A retrospective study design is susceptible to confounding, meaning that other risk factors may be present that were not measured. However, by collecting and comparing extensive baseline characteristics of each group, we attempted to limit this risk of confounding. Secondly, the sample size for this study just reached the number of patients needed for achieving statistical power, which is of course associated with the single-centre design. Also, not all gastroenterologists applied the STOP-criteria, possibly because of the lack of robust scientific evidence for these criteria. Furthermore, some patients did not want to discontinue their biologic treatment because of concerns about relapse, resulting in a relatively small group that discontinued according to the STOP-criteria. Another limitation is the fact that the majority of patients used anti-TNF resulting in a remaining lack of insight in the cumulative incidence of relapse in patients with other biologic agents, such as anti-integrin or interleukin-antagonist agents.
Larger and prospective studies are needed to examine STOP-like criteria for biologic therapy in patients with prolonged clinical remission. Optimal treatment duration is important from a medical, economic, social and above all patient perspective. Future studies should be focusing on factors associated with a higher relapse risk after treatment with biologic agents of all classes. For now, the decision whether to (dis)continue biologics should be based on shared decision making with each individual patient.
Conclusion
IBD patients who discontinued their biologic therapy according to the STOP-criteria had significantly more relapses at 12 and 36 months than patients who maintained biologic treatment. Further research is recommended to identify factors associated with a higher relapse risk in individual patients.
References
Caviglia F, Ribolsi M, Rizzi M, Emerenziani S, Annunziata ML, Cicala M. Maintenance of remission with infliximab in inflammatory bowel disease: efficacy and safety long-term follow-up. World J Gastroenterol. 2007;13:5238–44.
Kitayama M, Akazawa Y, Yoshikawa D, et al. Comparative efficacy of antitumor necrosis factor agents and tacrolimus in naïve steroid-refractory ulcerative colitis patients. Sci Rep. 2020;10:12546.
D’Haens G, Baert F, Van Assche G, et al. Early combined immunosuppression or conventional management in patients with newly diagnosed Crohn’s disease: an open randomised trial. Lancet. 2008;371:660–7.
Shivaji UN, Sharratt CL, Thomas T, et al. Review article: managing the adverse events caused by anti-TNF therapy in inflammatory bowel disease. Aliment Pharmacol Ther. 2019;49:664–80.
Hoentjen F, Van Bodegraven A. Safety of anti-tumor necrosis factor therapy in inflammatory bowel disease. World J Gastroenterol. 2009;15:2067–73.
Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362:1383–95.
Feagan BG, McDonald JWD, Panaccione R, et al. Methotrexate in combination with infliximab is no more effective than infliximab alone in patients with Crohn’s disease. Gastroenterology. 2014;146:681–8.
Van Linschoten RCA, Visser E, Niehot CD, et al. Systematic review: societal cost of illness of inflammatory bowel disease is increasing due to biologics and varies between continents. Aliment Pharmacol Ther. 2021;54:234–48.
Gisbert JP, Marin AC, Chaparro M. The risk of relapse after anti-TNF discontinuation in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2016;111:632–47.
Casanova MJ, Chaparro M, García-Sánchez V, et al. Evolution after anti-TNF discontinuation in patients with inflammatory bowel disease: a multicenter long-term follow-up study. Am J Gastroenterol. 2017;112:120–31.
Bortlik M, Duricova D, Machkova N, et al. Discontinuation of anti-tumor necrosis factor therapy in inflammatory bowel disease patients: a prospective observation. Scand J Gastroenterol. 2016;51:196–202.
Doherty G, Katsanos KH, Burisch J, et al. European Crohn’s and colitis organisation topical review on treatment withdrawal [‘Exit Strategies’] in inflammatory bowel disease. J Crohns Colitis. 2018;12:17–31.
Torres J, Bonovas S, Doherty G. ECCO guidelines on therapeutics in Crohn’s disease: medical treatment. J Crohns Colitis. 2020;14:4–22.
Gilissen LPL, Heinen GH, Rijpma-Jacobs L, et al. Neither inflammatory bowel disease nor immunosuppressants are associated with an increased risk of severe COVID-19: an observational Dutch cohort study. Clin Exp Med. 2022;22:465–76.
Dutch Association of Gastroenterologists. Biologicals: starting and stopping. 2009. https://www.mdl.nl/sites/www.mdl.nl/files/richlijnen/Start_Stop_BIOLOGICALS.pdf. Accessed 22 Dec 2022
Lewis JD, Chuai S, Nessel L, et al. Use of the non-invasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008;14:1660–6.
Lee JM, Kim YJ, Lee KM, et al. Long-term clinical outcome after infliximab discontinuation in patients with inflammatory bowel disease. Scand J Gastroenterol. 2018;53:1280–5.
Torres J, Boyapati RK, Kennedy NA, Louis E, Colombel JF, Satsangi J. Systematic review of effects of withdrawal of immunomodulators or biologic agents from patients with inflammatory bowel disease. Gastroenterology. 2015;149:1716–30.
Domènech E, Hinojosa J, Nos P, et al. Clinical evolution of luminal and perianal Crohn’s disease after inducing remission with infliximab: How long should patients be treated? Aliment Pharmacol Ther. 2005;22:1107–13.
Casanova MJ, Chaparro M, Nantes O, et al. Clinical outcome after anti-tumour necrosis factor therapy discontinuation in 1000 patients with inflammatory bowel disease: the EVODIS long-term study. Aliment Pharmacol Ther. 2021;53:1277–88.
Chauvin A, Le Thuaut A, Belhassan M, et al. Infliximab as a bridge to remission maintained by antimetabolite therapy in Crohn’s disease: a retrospective study. Dig Liver Dis. 2014;46:695–700.
Steenholdt C, Molazahi A, Ainsworth MA, Brynskov J, Thomsen OO, Seidelin JB. Outcome after discontinuation of infliximab in patients with inflammatory bowel disease in clinical remission: an observational Danish single center study. Scand J Gastroenterol. 2012;47:517–27.
Molander P, Färkkilä M, Salminen K, et al. Outcome after discontinuation of TNFα-blocking therapy in patients with inflammatory bowel disease in deep remission. Inflamm Bowel Dis. 2014;20:1021–8.
Bots SJ, Kuin S, Ponsioen CY, et al. Relapse rates and predictors for relapse in a real life cohort of IBD patients after discontinuation of anti-TNF therapy. Scand J Gastroenterol. 2019;54:281–8.
Molnár T, Lakatos PL, Farkas K, et al. Predictors of relapse in patients with Crohn’s disease in remission after 1 year of biological therapy. Aliment Pharmacol Ther. 2013;37:225–33.
Louis E, Mary JY, Vernier-Masouille G, et al. Maintenance of remission among patients with Crohn’s disease on antimetabolite therapy after infliximab therapy is stopped. Gastroenterology. 2012;142:63–70.
Waugh AWG, Garg S, Matic K, et al. Maintenance of clinical benefit in Crohn’s disease patients after discontinuation of infliximab: long-term follow-up of a single centre cohort. Aliment Pharmacol Ther. 2010;32:1129–34.
Sahu P, Vuyyuru SK, Kante B, et al. Relapse rate following withdrawal of anti-TNF therapy in patients with inflammatory bowel disease: a real-life cohort from northern India. Indian J Gastroenterol. 2020;39:388–97.
Kennedy NA, Warner B, Johnston EL, et al. Relapse after withdrawal from anti-TNF therapy for inflammatory bowel disease: an observational study, plus systematic review and meta-analysis. Aliment Pharmacol Ther. 2016;43:910–23.
Brooks AJ, Sebastian S, Cross SS, et al. Outcome of elective withdrawal of anti-tumour necrosis factor-α therapy in patients with Crohn’s disease in established remission. J Crohns Colitis. 2017;11:1456–62.
Kobayashi T, Motoya S, Nakamura S, et al. Discontinuation of infliximab in patients with ulcerative colitis in remission (HAYABUSA): a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol. 2021;6:429–37.
Mahmoud R, Van Lieshout C, Frederix GW, Jharap B, Oldenburg B. Continuation of anti-TNF in patients with ulcerative colitis is not cost-effective compared with treatment withdrawal: a Markov model. J Crohns Colitis. 2021;15:709–178.
Acknowledgements
The authors of this article would like to thank the staff of the Department of Gastroenterology and Hepatology from the Catharina Hospital Eindhoven for the possibility to conduct this research during extraordinary circumstances during the COVID-19 pandemic. We also would like to thank the staff of the statistical department for their advice.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
A. Stoker and L. Logghe are the main authors and wrote the main manuscript. L Logghe was in control of the study design, data collection and analysis. L. Gilissen was principal investigator, in control of patient recruitment, design of study and analysing results. M. van der Ende - van Loon, R. Schreuder, A. Stronkhorst and E. Schoon were responsible for patient recruitment as well as critical review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stoker, A.M.H., Logghe, L., van der Ende-van Loon, M.C.M. et al. Relapse rates after withdrawal versus maintaining biologic therapy in IBD patients with prolonged remission. Clin Exp Med 23, 2789–2797 (2023). https://doi.org/10.1007/s10238-023-00994-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-00994-6