Abstract
Purpose
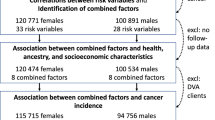
Although previous research has identified factors that may determine willingness to participate in research, relatively few studies have attempted to quantify the impact non-participation may have on exposure–disease associations. The aims of this study were to (a) investigate the associations between smoking, alcohol, diabetes, obesity, and socioeconomic status and the risk of colorectal cancer in a case–control study (59.7 and 47.2 % response fractions among cases and controls, respectively); and (b) perform sensitivity analyses to examine the possible influence of non-participation.
Methods
Logistic regression was used to estimate the exposure–disease associations. We then investigated the associations between various demographic and health factors and the likelihood that an individual would participate in the case–control study and then performed two sensitivity analyses (sampling weights and multiple imputation) to examine whether non-participation bias may have influenced the exposure–disease associations.
Results
The exposures alcohol, smoking, and diabetes were associated with an increased risk of colorectal cancer. We found some differences between cases and controls when examining the factors associated with the participation in the study, and in the sensitivity analyses, the exposure–disease associations were slightly attenuated when compared with those from the original analysis.
Conclusion
Non-participation may have biased the risk estimates away from the null, but generally not enough to change the conclusions of the study.
Similar content being viewed by others
Abbreviations
- AOR:
-
Adjusted odds ratio
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CRC:
-
Colorectal cancer
- OR:
-
Odds ratio
- RR:
-
Relative risk
- WA:
-
Western Australia
- WABOHS:
-
Western Australian Bowel Health Study
References
Galea S, Tracy M (2007) Participation rates in epidemiologic studies. Ann Epidemiol 17:643–653
Hartge P (2006) Participation in population studies. Epidemiology 17:252–254
Morton LM, Cahill J, Hartge P (2006) Reporting participation in epidemiologic studies: a survey of practice. Am J Epidemiol 163:197–203
Keeble C, Barber S, Law GR, Baxter PD (2013) Participation bias assessment in three high-impact journals. SAGE Open 3:1–5
Pandeya N, Williams GM, Green AC, Webb PM, Whiteman DC (2009) Do low control response rates always affect the findings? Assessments of smoking and obesity in two Australian case–control studies of cancer. Aust N Z J Public Health 33:312–319
Larsson SC, Orsini N, Wolk A (2005) Diabetes mellitus and risk of colorectal cancer: a meta-analysis. J Natl Cancer Inst 97:1679–1687
World Cancer Research Fund/American Institute for Cancer Research (2007) Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR, Washington
Cho E, Smith-Warner SA, Ritz J et al (2004) Alcohol intake and colorectal cancer: a pooled analysis of 8 cohort studies. Ann Intern Med 140:603–613
Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M (2009) The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer 125:171–180
Moskal A, Norat T, Ferrari P, Riboli E (2006) Alcohol intake and colorectal cancer risk: a dose-response meta-analysis of published cohort studies. Int J Cancer 120:664–671
Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P (2008) Smoking and colorectal cancer: a meta-analysis. JAMA 300:2765–2778
Liang PS, Chen TY, Giovannucci E (2009) Cigarette smoking and colorectal cancer incidence and mortality: systematic review and meta-analysis. Int J Cancer 124:2406–2415
Aarts MJ, Lemmens VEPP, Louwman MWJ, Kunst AE, Coebergh JWW (2010) Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer 46:2681–2695
Boyle T, Heyworth J, Bull F, McKerracher S, Platell C, Fritschi L (2011) Timing and intensity of recreational physical activity and the risk of subsite-specific colorectal cancer. Cancer Causes Control 22:1647–1658
Clapin HF, Fritschi L, Iacopetta B, Heyworth JS (2012) Dietary and supplemental folate and the risk of left- and right-sided colorectal cancer. Nutr Cancer 64:937–945
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G (2000) The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health 24:576–583
Holman CDAJ, Bass AJ, Rouse IL, Hobbs MST (1999) Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Public Health 23:453–459
Australian Bureau of Statistics (2008) Census of population and housing: socio-economic indexes for areas (SEIFA), Australia. Catalogue Number 2033.0.55.001. Australian Bureau of Statistics, Canberra, Australia
Department of Health and Aged Care and the University of Adelaide (1999) Measuring remoteness: accessibility/remoteness index of Australia (ARIA). Occasional Papers: New Series No 6. Commonwealth of Australia, Canberra
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Royston P, White IR (2011) Multiple imputation by chained equations (MICE): implementation in Stata. J Stat Softw 45:1–20
Zou G (2004) A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–706
Sterne JAC, White IR, Carlin JB et al (2009) Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338
The University of Wisconsin–Madison Social Science Computing Cooperative (2013) Multiple imputation in Stata. http://www.ssc.wisc.edu/sscc/pubs/stata_mi_intro.htm. Accessed 14 Sept 2013
Azur MJ, Stuart EA, Frangakis C, Leaf PJ (2011) Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 20:40–49
Willett WC (1998) Nutritional epidemiology, 2nd edn. Oxford University Press, New York
Fedirko V, Tramacere I, Bagnardi V et al (2011) Alcohol drinking and colorectal cancer risk: an overall and dose–response meta-analysis of published studies. Ann Oncol 22:1958–1972
Krämer HU, Schöttker B, Raum E, Brenner H (2012) Type 2 diabetes mellitus and colorectal cancer: meta-analysis on sex-specific differences. Eur J Cancer 48:1269–1282
Ma Y, Yang Y, Wang F et al (2013) Obesity and risk of colorectal cancer: a systematic review of prospective studies. PLoS One 8:e53916
Colt JS, Schwartz K, Graubard BI et al (2011) Hypertension and risk of renal cell carcinoma among white and black Americans. Epidemiology 22:797–804
Kreiger N, Nishri ED (1997) The effect of nonresponse on estimation of relative risk in a case–control study. Ann Epidemiol 7:194–199
Wigertz A, Lönn S, Hall P, Feychting M (2010) Non-participant characteristics and the association between socioeconomic factors and brain tumour risk. J Epidemiol Community Health 64:736–743
López R, Frydenberg M, Baelum V (2008) Non-participation and adjustment for bias in case–control studies of periodontitis. Eur J Oral Sci 116:405–411
Hatch EE, Kleinerman RA, Linet MS et al (2000) Do confounding or selection factors of residential wiring codes and magnetic fields distort findings of electromagnetic fields studies? Epidemiology 11:189–198
Ramos E, Lopes C, Barros H (2004) Investigating the effect of nonparticipation using a population-based case–control study on myocardial infarction. Ann Epidemiol 14:437–441
Madigan MP, Troisi R, Potischman N et al (2000) Characteristics of respondents and non-respondents from a case–control study of breast cancer in younger women. Int J Epidemiol 29:793–798
Vrijheid M, Richardson L, Armstrong BK et al (2009) Quantifying the impact of selection bias caused by nonparticipation in a case–control study of mobile phone use. Ann Epidemiol 19(33–41):e31
Hall AE, Sanson-Fisher RW, Lynagh MC, Threlfall T, D’Este CA (2013) Format and readability of an enhanced invitation letter did not affect participation rates in a cancer registry-based study: a randomized controlled trial. J Clin Epidemiol 66:85–94
Mols F, Aaronson NK, Vingerhoets AJJM et al (2007) Quality of life among long-term non-Hodgkin lymphoma survivors. Cancer 109:1659–1667
Richiardi L, Boffetta P, Merletti F (2002) Analysis of nonresponse bias in a population-based case–control study on lung cancer. J Clin Epidemiol 55:1033–1040
Smith T, Stein KD, Mehta CC et al (2007) The rationale, design, and implementation of the American Cancer Society’s studies of cancer survivors. Cancer 109:1–12
Geller B, Mace J, Vacek P, Johnson A, Lamer C, Cranmer D (2011) Are cancer survivors willing to participate in research? J Community Health 36:772–778
Mols F, Oerlemans S, Denollet J, Roukema J-A, van de Poll-Franse LV (2012) Type D personality is associated with increased comorbidity burden and health care utilization among 3080 cancer survivors. Gen Hosp Psychiatry 34:352–359
Kelly B, Fraze T, Hornik R (2010) Response rates to a mailed survey of a representative sample of cancer patients randomly drawn from the Pennsylvania Cancer Registry: a randomized trial of incentive and length effects. BMC Med Res Methodol 10:65
Morabia A, Bemstein M, Héritier S, Khatchatrian N (1996) Relation of breast cancer with passive and active exposure to tobacco smoke. Am J Epidemiol 143:918–928
Wingo PA, Ory HW, Layde PM, Lee NC (1988) The evaluation of the data collection process for a multicenter, population-based, case–control design. Am J Epidemiol 128:206–217
Girgis A, Boyes A, Sanson-Fisher RW, Burrows S (2000) Perceived needs of women diagnosed with breast cancer: rural versus urban location. Aust N Z J Public Health 24:166–173
Maclure M, Hankinson S (1990) Analysis of selection bias in a case–control study of renal adenocarcinoma. Epidemiology 1:441–447
Acknowledgments
The authors gratefully acknowledge Kieran McCaul for statistical advice, the people who generously gave their time to participate in this research, the clinicians who gave permissions to approach their patients, the WA Cancer Registry staff (Timothy Threlfall in particular) for assistance with case ascertainment and recruitment, and members of the WABOHS team (Cameron Platell, Kieran McCaul, David Crawford, Cassandra Clayforth, Clare Tran, Jenny Landrigan, Beatriz Cuesta-Briand) for study management and collection of data used in this study. This work was supported by the Australian National Health and Medical Research Council (Project Grant #353568, Fellowship #1072266 to TB, and Fellowship 37614900 to LF), the Canadian Institutes of Health Research (Fellowship #300068 to TB), the Michael Smith Foundation for Health Research (Fellowship #5553 to TB), and the Izaak Walton Killam Memorial Fund for Advanced Studies (Honorary UBC Killam Postdoctoral Research Fellowship to TB).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Boyle, T., Fritschi, L., Tabatabaei, S.M. et al. Smoking, alcohol, diabetes, obesity, socioeconomic status, and the risk of colorectal cancer in a population-based case–control study. Cancer Causes Control 25, 1659–1668 (2014). https://doi.org/10.1007/s10552-014-0470-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-014-0470-7