Abstract
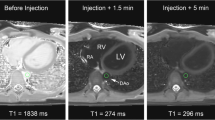
This study was performed to determine the best concentration of gadofosveset at 1.5 and 3 T MRI for quantitative myocardial perfusion analysis. 18 healthy volunteers have been examined at a 1.5 and a 3 T MRI system assigned to one of three dose groups: low dose (0.00375 mmol/kg), medium dose (0.0075 mmol/kg), high dose (0.0150 mmol/kg). A T1-weighted saturation recovery turboFLASH sequence with parallel imaging was used. Two perfusion scans were performed for each field strength and volunteer. Peak signal-to-noise-ratio, maximum contrast-enhancement-ratio and myocardial blood flow (MBF) were calculated. MBF values were significantly higher at 1.5 T in the medium and the high dose groups than in the low dose group (p < 0.001). Higher MBF values could be found at 3 T for the second perfusion scan in the medium and both perfusion scans in the high dose group compared to the low dose group. Optimal dose of gadofosveset for quantitative perfusion analysis at 1.5 T is 0.00375 mmol/kg as higher doses caused overestimation of the MBF. At 3 T 0.0075 mmol/kg seems to be the best dose for a single perfusion scan, while for a second perfusion scan MBF may be overestimated.







Similar content being viewed by others
References
Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O’Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y (2009) Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 119(3):e21–e181. doi:10.1161/CIRCULATIONAHA.108.191261
Bodi V, Sanchis J, Lopez-Lereu MP, Nunez J, Mainar L, Monmeneu JV, Husser O, Dominguez E, Chorro FJ, Llacer A (2007) Prognostic value of dipyridamole stress cardiovascular magnetic resonance imaging in patients with known or suspected coronary artery disease. J Am Coll Cardiol 50(12):1174–1179. doi:10.1016/j.jacc.2007.06.016
Jahnke C, Nagel E, Gebker R, Kokocinski T, Kelle S, Manka R, Fleck E, Paetsch I (2007) Prognostic value of cardiac magnetic resonance stress tests: adenosine stress perfusion and dobutamine stress wall motion imaging. Circulation 115(13):1769–1776. doi:10.1161/CIRCULATIONAHA.106.652016
Chiribiri A, Bettencourt N, Nagel E (2009) Cardiac magnetic resonance stress testing: results and prognosis. Curr Cardiol Rep 11(1):54–60
Jerosch-Herold M, Kwong RY (2008) Optimal imaging strategies to assess coronary blood flow and risk for patients with coronary artery disease. Curr Opin Cardiol 23(6):599–606. doi:10.1097/HCO.0b013e328312c2f5
Ritter CO, Wilke A, Wichmann T, Beer M, Hahn D, Kostler H (2011) Comparison of intravascular and extracellular contrast media for absolute quantification of myocardial rest-perfusion using high-resolution MRI. J Magn Reson Imaging 33(5):1047–1051. doi:10.1002/jmri.22557
Rohrer M, Bauer H, Mintorovitch J, Requardt M, Weinmann HJ (2005) Comparison of magnetic properties of MRI contrast media solutions at different magnetic field strengths. Invest Radiol 40(11):715–724
Lauffer RB, Parmelee DJ, Dunham SU, Ouellet HS, Dolan RP, Witte S, McMurry TJ, Walovitch RC (1998) MS-325: albumin-targeted contrast agent for MR angiography. Radiology 207(2):529–538
Breitschaft A, Stahlmann R (2009) Nephrogenic systemic fibrosis. Med Monatsschr Pharm 32(10):377–382
Shamsi K, Yucel EK, Chamberlin P (2006) A summary of safety of gadofosveset (MS-325) at 0.03 mmol/kg body weight dose: phase II and phase III clinical trials data. Invest Radiol 41(11):822–830. doi:10.1097/01.rli.0000242836.25299.8f
Naehle CP, Muller A, Willinek WA, Meyer C, Hestermann T, Gieseke J, Schild H, Thomas D (2009) First-pass and steady-state magnetic resonance angiography of the thoracic vasculature using gadofosveset trisodium. J Magn Reson Imaging 30(4):809–816. doi:10.1002/jmri.21919
Bonel HM, Saar B, Hoppe H, Keo HH, Husmann M, Nikolaou K, Ludwig K, Szucs-Farkas Z, Srivastav S, Kickuth R (2009) MR angiography of infrapopliteal arteries in patients with peripheral arterial occlusive disease by using Gadofosveset at 3.0 T: diagnostic accuracy compared with selective DSA. Radiology 253(3):879–890. doi:10.1148/radiol.2533081627
Kraitchman DL, Chin BB, Heldman AW, Solaiyappan M, Bluemke DA (2002) MRI detection of myocardial perfusion defects due to coronary artery stenosis with MS-325. J Magn Reson Imaging 15(2):149–158. doi:10.1002/jmri.10051
Prompona M, Cyran C, Nikolaou K, Bauner K, Reiser M, Huber A (2009) Contrast-enhanced whole-heart MR coronary angiography at 3.0 T using the intravascular contrast agent gadofosveset. Invest Radiol 44(7):369–374
Sourbron S, Dujardin M, Makkat S, Luypaert R (2007) Pixel-by-pixel deconvolution of bolus-tracking data: optimization and implementation. Phys Med Biol 52(2):429–447. doi:10.1088/0031-9155/52/2/009
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105(4):539–542
Reeder SB, Wintersperger BJ, Dietrich O, Lanz T, Lanz T, Greiser A, Reiser MF, Glazer GM, Schoenberg SO (2005) Practical approaches to the evaluation of signal-to-noise ratio performance with parallel imaging: application with cardiac imaging and a 32-channel cardiac coil. Magn Reson Med 54(3):748–754. doi:10.1002/mrm.20636
Jerosch-Herold M, Swingen C, Seethamraju RT (2002) Myocardial blood flow quantification with MRI by model-independent deconvolution. Med Phys 29(5):886–897
Nesto RW, Kowalchuk GJ (1987) The ischemic cascade: temporal sequence of hemodynamic, electrocardiographic and symptomatic expressions of ischemia. Am J Cardiol 59(7):23C–30C
Wagner A, Mahrholdt H, Holly TA, Elliott MD, Regenfus M, Parker M, Klocke FJ, Bonow RO, Kim RJ, Judd RM (2003) Contrast-enhanced MRI and routine single photon emission computed tomography (SPECT) perfusion imaging for detection of subendocardial myocardial infarcts: an imaging study. Lancet 361(9355):374–379. doi:10.1016/S0140-6736(03)12389-6
Barkhausen J, Hunold P, Jochims M, Debatin JF (2004) Imaging of myocardial perfusion with magnetic resonance. J Magn Reson Imaging 19(6):750–757. doi:10.1002/jmri.20073
Nelson KL, Runge VM (1995) Basic principles of MR contrast. Top Magn Reson Imaging 7(3):124–136
Puderbach M, Risse F, Biederer J, Ley-Zaporozhan J, Ley S, Szabo G, Semmler W, Kauczor HU (2008) In vivo Gd-DTPA concentration for MR lung perfusion measurements: assessment with computed tomography in a porcine model. Eur Radiol 18(10):2102–2107. doi:10.1007/s00330-008-0974-1
Gerber BL, Raman SV, Nayak K, Epstein FH, Ferreira P, Axel L, Kraitchman DL (2008) Myocardial first-pass perfusion cardiovascular magnetic resonance: history, theory, and current state of the art. J Cardiovasc Magn Reson 10(1):18. doi:10.1186/1532-429X-10-18
Wang Y, Moin K, Akinboboye O, Reichek N (2005) Myocardial first pass perfusion: steady-state free precession versus spoiled gradient echo and segmented echo planar imaging. Magn Reson Med 54(5):1123–1129. doi:10.1002/mrm.20700
Christian TF, Aletras AH, Arai AE (2008) Estimation of absolute myocardial blood flow during first-pass MR perfusion imaging using a dual-bolus injection technique: comparison to single-bolus injection method. J Magn Reson Imaging 27(6):1271–1277. doi:10.1002/jmri.21383
Wyss CA, Koepfli P, Fretz G, Seebauer M, Schirlo C, Kaufmann PA (2003) Influence of altitude exposure on coronary flow reserve. Circulation 108(10):1202–1207. doi:10.1161/01.CIR.0000087432.63671.2E
Jerosch-Herold M, Hu X, Murthy NS, Rickers C, Stillman AE (2003) Magnetic resonance imaging of myocardial contrast enhancement with MS-325 and its relation to myocardial blood flow and the perfusion reserve. J Magn Reson Imaging 18(5):544–554. doi:10.1002/jmri.10384
Acknowledgments
Parts of the research will be used for the doctor thesis of Sebastian Niedermayer at the Ludwig-Maximilians University of Munich.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Niedermayer, S., Sourbron, S., Prompona, M. et al. Dose response of the intravascular contrast agent gadofosveset trisodium in MR perfusion imaging of the myocardium using a quantitative evaluation. Int J Cardiovasc Imaging 29, 1527–1536 (2013). https://doi.org/10.1007/s10554-013-0250-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-013-0250-6