Abstract
The first objective of this study was to determine and quantify variations in diabetes mortality by migrant status in different European countries. The second objective was to investigate the hypothesis that diabetes mortality is higher in migrant groups for whom the country of residence (COR) is more affluent than the country of birth (COB). We obtained mortality data from 7 European countries. To assess migrant diabetes mortality, we used direct standardization and Poisson regression. First, migrant mortality was estimated for each country separately. Then, we merged the data from all mortality registers. Subsequently, to examine the second hypothesis, we introduced gross domestic product (GDP) per capita of COB in the models, as an indicator of socio-economic circumstances. The overall pattern shows higher diabetes mortality in migrant populations compared to local-born populations. Mortality rate ratios (MRRs) were highest in migrants originating from either the Caribbean or South Asia. MRRs for the migrant population as a whole were 1.9 (95% CI 1.8–2.0) and 2.2 (95% CI 2.1–2.3) for men and women respectively. We furthermore found a consistently inverse association between GDP of COB and diabetes mortality. Most migrant groups have higher diabetes mortality rates than the local-born populations. Mortality rates are particularly high in migrants from North Africa, the Caribbean, South Asia or low-GDP countries. The inverse association between GDP of COB and diabetes mortality suggests that socio-economic change may be one of the key aetiological factors.
Similar content being viewed by others
Introduction
The global burden of diabetes has been estimated at 285 million patients in 2010. By 2030, this disease is expected to affect 438 million persons, especially in developing countries. Socio-economic development, including urbanization and a sedentary lifestyle, are mainly held responsible for this increase [1–3].
A rapid change in societal context is experienced by migrants who migrate from less to more economically developed countries [3]. They end up in a macro environment that is different from that of their country of birth (COB), in terms of social, economic and cultural characteristics. Moreover, compared with the country of residence (COR) their COBs are often going through an earlier phase of the epidemiologic transition. Hence, the disease environment of the CORs is different from that of their COBs. For example while risk factors for infectious diseases are generally highly prevalent in the respective COBs, risk factors for non-communicable diseases are in general ubiquitous in the CORs [4–6]. Consequently, we may expect most migrant groups moving from less to more economically developed countries to experience a decline in infectious disease rates following migration to the COR and an increase in the level of non-communicable diseases, such as type 2 diabetes [7, 8].
Type 2 diabetes mellitus is highly prevalent among migrants and indigenous populations throughout the world [9–12]. Many migrant groups have higher rates of diabetes prevalence compared to both the non-migrants in the COR and the local-born population in the COB [13–15]. While data on diabetes mortality among migrant populations are relatively scarce, some studies have reported higher diabetes mortality among women of Moroccan descent compared to the local-born populations [7, 8]. An 11-year follow-up of the Southall Diabetes Survey furthermore indicates that South Asian diabetic patients in the United Kingdom have excess diabetes mortality compared to European diabetic patients, especially at younger ages [16]. Findings on differences in diabetes care between migrants and local-born populations have been inconsistent. A review of US studies indicates worse diabetes care among migrant populations [17]; whereas recent European studies show equity in many aspects of diabetes care [18, 19], despite differences in metabolic control and complications [20, 21]. The higher prevalence of diabetes as well as the higher severity of the disease in migrant populations might be responsible for their excess diabetes mortality.
The first objective of this paper is to present an overview of variations according to migrant status in mortality from diabetes mellitus in 7 European countries (Belgium, Denmark, England & Wales, France, the Netherlands, Scotland and Spain). To our knowledge, this study is the first to analyze the relationship between migrant origin and diabetes mortality in several European countries at the same time. Mapping out differences in diabetes mortality by COB across different European countries enables us to discern country-specific as well as general patterns in migrant diabetes mortality. The second objective focuses on one possible explanation for the relatively high diabetes mortality among migrant populations, namely the importance of socio-economic change. We hypothesize that diabetes mortality is higher in migrant groups for whom the socio-economic level of the COR is higher than that of the COB, since migrants who migrate from less to more economically developed countries are likely to undergo the largest shift in environment and lifestyle. These migrants are expected to become exposed to more sedentary activities and energy-dense diets high in salt and fat. The evidence on the acculturation of lifestyles is still sparse. While some studies suggest the adoption of rather unhealthy lifestyles [6, 22], others suggest that the pace may differ between migrant groups and by age and generation [23, 24]. To examine this second hypothesis, we used the evidence across Europe to examine diabetes mortality among migrants from COBs with widely different socio-economic levels.
Methods
Design and study population
Data on diabetes mortality were available for 7 European countries. Table 1 describes the characteristics of the mortality studies included in the analyses. The age-standardized mortality rates presented in this table are based on all available ages, whereas for the calculation of the mortality rate ratios a selected age range was used (cf. Table 3). All studies covered the entire national territory and included all subgroups of the population. Data have preferably been obtained from record linkage studies (Belgium, Denmark, The Netherlands). In these studies, people enumerated at the population census were followed through a linkage between the census and the mortality register. For Belgium, the cohort was semi-closed. Nobody could enter the population during the follow-up period, but people could leave the population by emigration or death. For Denmark and the Netherlands, an open cohort design was used in which people could enter or exit the study at any point in time during the follow-up period. For countries that couldn’t provide data based on record linkage (England & Wales, France, Scotland and Spain), unlinked data were used. The number of deaths according to COB provided by this type of study was derived from the respective national mortality registers; whereas the person-years at risk (PY) was based on census information. Data were centred around the latest population census.
Variables
To determine mortality from diabetes mellitus, the International Classification of Diseases (ICD) has been employed. Depending on the country and years of the studies, either the 8th, 9th or 10th revision of the ICD has been used. The relevant codes were ICD-8 and ICD-9:250 and ICD-10:E10–E14.
The variable COB was used to indicate migrant origin. All people who migrated to a country other than their COB were included. An additional criterion was that migrants should usually be resident in the respective CORs. Some specific groups, such as asylum seekers, were excluded from the analyses. Moreover, the definition of migrants used in the French data omits those born outside France but with French nationality. COB was classified into COB groups based on the following criteria: (1) focus on mainly non-western COBs; (2) sufficient numbers of deaths and PY in different COB groups in each country-specific data set, and (3) correspondence, where possible, between countries in the classification of COB.
Age was classified into 5-year age bands. With regard to mortality, the age recorded corresponded to age at time of the population census in the linked studies and to age at death in the unlinked studies. Consequently, persons from the census linked studies are generally older than persons from the unlinked studies classified into the same age group. To enhance comparability between countries, we therefore restricted our analyses to ages 20–74 for the linked studies and to ages 25–79 for the unlinked studies.
To examine the second hypothesis, we divided the migrant populations into four categories according to GDP per capita of their respective COBs. In a first step, each migrant group was assigned the GDP per capita estimate of their COB. When information was not available on country level, the population-weighted average of the GDP of the region was allocated. Secondly, we classified COB into GDP quartiles (Q): (1Q) GDP < $ 2,400; (2Q) $ 2,400 ≤ GDP < $ 5,300; (3Q) $ 5,300 ≤ GDP < $ 9,500; (4Q) GDP ≥ $ 9,500. Thirdly, a variable with 5 categories was constructed: (0) CORs (reference category), (1) 1Q, (2) 2Q, (3) 3Q and (4) 4Q. For an overview of the quartiles and their respective COB groups, we refer to Table 2. GDP estimates were derived from purchasing power parity calculations and mainly cover the period 1998–2002 [26].
Data analysis
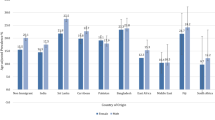
To obtain an overview of migrant differences in diabetes mortality, age-standardized mortality rates (ASMRs) were computed for each country and COB, directly standardized using the WHO World Standard Population [25]. To examine relative differences in diabetes mortality between migrant groups, country-specific Poisson regression models were fitted using mortality rates as the dependent variable, and COB as the independent variable. All analyses were adjusted for age and performed using Stata 11.
In subsequent steps, a pooled data set of all countries was created to estimate diabetes mortality among different aggregates of COB, as some migrant groups are represented in several European countries. To this pooled data set, we applied regression analyses. To account for between-country differences in diabetes mortality registration, we included the overall diabetes mortality level of each COR as an independent variable in our Poisson regression models. To examine the second hypothesis, the variable ‘GDP of COB’ classified into five categories—4 quartiles and the CORs—was included in the regression model, CORs as reference. Furthermore, several sensitivity analyses were performed. First, we repeatedly carried out the GDP mortality analyses, while excluding a different COB group each time. Second, we restricted these analyses to a narrower age range (25–64 years).
As mentioned earlier, for the analyses per country we restricted our study population to men and women aged 20–74 for the linked studies and aged 25–79 for the unlinked studies. For the pooled analyses on the other hand, the study population consisted of 25- to 79-year-olds. All analyses were gender specific.
Results
Migrant diabetes mortality
Country-specific differences in diabetes mortality by COB
Table 3 presents the country-specific diabetes MRRs by COB adjusted for age. The overall tendency is one of higher diabetes mortality among migrant groups compared to the local-born populations. Yet, there are large differences according to COR and COB.
Migrants from North Africa generally have a higher diabetes mortality compared to the respective local-born populations. The highest MRRs are observed for North African women in Spain (2.2; 95% CI 1.8–2.8) and North African men in Scotland (6.2; 95% CI 2.0–19.3), although the confidence interval of the MRR is quite large for Scotland. Diabetes MRRs were non-significantly lower than 1 for North African men in Belgium and for North African women in England & Wales. Among Turkish migrants, the MRRs range from 0.9 to 5.2, but are mostly centred around 2. The highest diabetes MRRs are observed in migrants from South Asia (Bangladesh, India, Sri Lanka and Pakistan). MRRs around 5 are no exception. For Pakistani men in England & Wales, the diabetes MRR even amounts to 8.5 (95% CI 7.2–10.1). Higher diabetes mortality among migrants is, however, not limited to these groups.
Cross-country differences in diabetes mortality by COB
Table 4 shows the gender specific diabetes MRRs for different aggregates of COB, adjusted for age and overall diabetes mortality level of the CORs. In model 1 MRRs for the migrant population as a whole are presented. Model 2 presents the MRRs for different COB groups, namely for migrants from North Africa, Turkey and South Asia. For the migrant population as a whole (model 1), MRRs are 1.9 (95% CI 1.8–2.0) and 2.2 (95% CI 2.1–2.3) for men and women respectively. With regard to the different aggregates of COB (model 2), diabetes MRRs are highest for migrants from South Asia. More specifically MRRs are 3.7 (95% CI 3.4–4.0) for men and 4.4 (95% CI 4.0–4.9) for women.
Diabetes mortality and GDP
The association between diabetes mortality and GDP per capita of COB is also shown in Table 4 (model 3). As GDP quartile of COB increases, the diabetes MRRs (adjusted for age and overall mortality level of CORs) decrease. In both men and women, a gradient is discerned. Migrants originating from countries where GDP is lower than $ 2,400 have the highest MRR, followed by migrants from countries where GDP is between $ 2,400 and $ 5,300 etc. The MRR for migrants from countries in the 4Q of GDP is comparable to that of the CORs.
To examine the robustness of these estimates, we performed several sensitivity analyses. First, we repeatedly carried out the GDP mortality analyses, while excluding a different COB group each time. Second, we restricted our analyses to a narrower age range (25–64 years). The results of these sensitivity analyses indicate that the diabetes MRRs for the different GDP quartiles are fairly robust. For example, when we leave North African migrants out of the analyses, MRRs for men were 4.0 (95% CI 3.6–4.4), 3.6 (95% CI 3.6–3.9), 1.8 (95% CI 1.7–2.0) and 1.1 (95% CI 0.9–1.2) for the 1st, 2nd, 3rd and 4th quartile respectively. For women, MRRs were 4.1 (95% CI 3.6–4.6) for the 1st quartile, 4.3 (95% CI 3.9–4.6) for the 2nd, 2.2 (95% CI 2.0–2.5) for the 3rd and 0.9 (95% CI 0.8–1.1) for the 4th quartile (results not shown).
Discussion
Summary of findings
This study indicates that there are important differences in diabetes mortality by COB in Europe. The overall pattern is one of higher diabetes mortality among migrant groups. The highest diabetes mortality is observed for migrants from South Asia. High diabetes MRRs are furthermore observed in migrants from North Africa, the Caribbean and in Turkish women. Finally, we found an inverse association between GDP per capita of COB and diabetes mortality.
Methodological considerations
Registration issues
Data from Belgium, Denmark and the Netherlands were obtained from census linked mortality follow-up studies, while data from all other countries were unlinked. Unlinked data are more susceptible to numerator-denominator biases [8]. For example differences between measurement of COB in the mortality register (numerator) and in the population census (denominator) might occur [28].
Another possible source of error may be under-registration of residents from migrant groups either in the population census or in the death register. We expect census under-registration of migrants to be rather small. Under-registration of deaths of migrant groups may be more substantial due to return migration at older ages, as found by Ringbäck-Weitoft et al. for Sweden [29] and might have led to an underestimation of (diabetes) mortality for (some) migrant groups.
The analysis of cause-specific mortality data at a European level inevitably raises several questions concerning the comparability of death registration. Discrepancies between European countries may exist in models of death certificates, nature and amount of information entered, application of the rules for selection of the underlying and contributing causes of death, coding practices, implementation of ICD and of automated coding systems [30, 31]. As can be derived from the age-adjusted diabetes mortality rates in Table 1, it is likely that there exist differential registration practices between the European countries. Considering these between-country differences, we decided not to compare ASMRs between countries. In addition, to control for confounding by differential registration, we included the overall COR diabetes mortality level as an independent variable in our pooled Poisson analyses.
As diabetes mellitus is often part of a complex clinical picture, in which the disease is frequently considered to be of secondary importance, diabetes mortality registration problems may be particularly pronounced. Diabetes is often not registered as the underlying cause of death but as one of the contributing causes. Due to the widely accepted practice of using the underlying cause of death as the reference, this leads to a severe under-estimation of the burden of diabetes-related deaths [31–34]. In France the use of multiple rather than contributing causes of death more than doubled diabetes-related mortality rates for the period 2000–2002 [33]. Taking into account both diabetes as underlying and as contributing cause, the burden of diabetes related mortality in the Brussels-Capital region for the period 2001–2005 more than quadrupled. To the extent that the use of diabetes as an underlying/contributing cause differs between countries, cross-country comparisons of diabetes mortality are difficult to establish. Moreover, differential use of these concepts between COB groups within countries may bias our results. However, in the Brussels-Capital Region, differences in the use of diabetes as an underlying/contributing cause between different COB groups appear to be rather minor. The ratio ‘diabetes underlying:contributing cause’ was 4.7 (95% CI 4.2–5.3), 4.8 (95% CI 3.0–8.1) and 4.8 (95% CI 1.8–16.1) for the local-born population and migrants from North Africa and Turkey respectively (H. Vandenheede, P. Deboosere, unpublished data).
Despite these registration issues, the fact that the MRRs for different COBs echo findings from prevalence data—showing a high burden of diabetes in many migrant groups in Europe, especially in migrants from South Asia and North Africa—indicate that differences in diabetes mortality by COB are not only due to differential registration practices, but also reflect actual differences in diabetes prevalence [9, 11–13] (cf. infra).
Other methodological issues
During our analyses, we were confronted with the problem of small migrant groups and hence few diabetes deaths among these groups. We mainly dealt with this problem by grouping migrant populations (for example migrants from Algeria, Egypt, Libya, Morocco, Sudan and Tunisia have been regrouped into “North Africans”). With these regroupings, we generally managed to get sufficiently precise MRR estimates. A disadvantage of this method may be that it obscures differences within the aggregate of COB.
To examine the second hypothesis that diabetes mortality is higher in migrants who originate from less economically developed countries, we introduced purchasing power parity estimates of GDP per capita in our analyses. To estimate the degree of (socio-)economic change experienced by migrants, we created a ‘scale’ of economic development of COBs by dividing the COBs into quartiles of GDP. In this way we were able to take the extent of socio-economic change experienced by different migrant groups into account. Although GDP per capita is a controversial measure in the realm of economic statistics, most authors agree that it is acceptable as a measure of economic development. Moreover, GDP is strongly inversely related to the percentage of employment in the primary sector. Consequently, reverse patterns would be observed by applying the latter measure [35–37].
A final methodological consideration worthy of mention is that we were not able to take current socio-economic status into account. Consequently, we have no idea to what extent differences in diabetes mortality by COB can be explained by current socio-economic differences between (some) migrant groups and the local-born population. As socio-economic status and both diabetes morbidity and mortality are often inversely related [38] and as migrant groups frequently have a lower socio-economic position [39], we may assume that the mortality differences observed in our study could partially be explained when taking this indicator into consideration. On the other hand, the observed ethnic differences in diabetes mortality are so large that it is highly improbable that they can be entirely explained by socio-economic differences [40]. In Belgium we found that differences in income and educational attainment between the Turkish and Moroccan communities and the local-born population only explain about one third of the differences in diabetes prevalence between these groups [41].
Theoretical considerations
To our knowledge, this is the first time migrant diabetes mortality has been explored across different European countries. Our results indicate that there are substantial differences in mortality from diabetes mellitus by COB in all seven European countries. For Belgium, England & Wales, France and the Netherlands, by and large our results are in line with previously published data on migrant diabetes mortality [7, 8, 21, 40]. By contrast, for the other countries in our study—i.e. Denmark, Scotland and Spain—little previous research has been conducted on cause-specific and diabetes mortality among migrants. We reported, possibly for the first time, higher diabetes mortality rates for several migrant groups, including Turkish, Sri Lankan and Pakistani migrants in Denmark, South Asian migrants in England & Wales and Scotland and North African women in Spain.
Analogous to explanations for excess migrant diabetes prevalence, the observed excess migrant diabetes mortality may to a large extent be explained by differences between migrants and local-born populations in diabetes incidence [42]. Differences between migrant and local-born groups in case fatality may furthermore play a part; the latter being strongly associated with differences in access to and quality of diabetes care, metabolic control and complications [16–21, 42].
Although the overall picture is one of excess migrant diabetes mortality, substantial variation still exists depending on the respective CORs and COBs. There are large differences in COB-specific MRRs between different CORs. Though difficult to compare because of differential registration practices between European countries, it is unlikely that these between-country differences in diabetes mortality by COB can be entirely attributed to differences in registration, as differences between age-adjusted diabetes mortality rates among the local-born populations are rather small (cf. Table 1). Considerable differences by COB group also exist. These findings suggest that although most migrant groups are at a higher risk of dying from diabetes mellitus, there is some heterogeneity in risk factors, such as diabetes prevalence and diabetes-related complications. In addition, between-country differences in the same COB groups suggest that the host environment also plays a key role.
A partial explanation: the importance of (a sweeping) socio-economic change
In this study an inverse association between GDP per capita of COB and diabetes mortality among migrants was found.
This association suggests that a sweeping change to an affluent environment may play an important role in explaining excess migrant diabetes mortality. This hypothesis is underpinned by the recent diabetes prevalence estimates of the International Diabetes Federation. In the near future, the increase in diabetes prevalence is expected to be largest in countries and regions that are undergoing rapid economic growth [2, 43]. The relationship between (rapid) socio-economic growth and diabetes morbidity and mortality is likely to be mediated by an increasing urbanization and drastic lifestyle changes, such as a decrease in physical activity and a high-fat, energy-dense diet [4, 5, 37]. However, genetic differences between countries and regions with different GDP per capita may also play a part. Moreover, migrants (and other populations undergoing sweeping economic growth) may be frequently faced with difficulties of adaptation to their new environments, which may result, among other things, in (psycho)social stress and a (maladaptive) ‘obesogenic’ lifestyle, both risk factors for type 2 diabetes mellitus [4, 44]. Further research is needed to corroborate or falsify this hypothesis. Research focusing on diabetes prevalence and mortality among children of migrants could provide useful insights about the stability (rather than change) of environmental exposures in host countries. If migration from less to more developed countries is a key determinant of migrant diabetes prevalence and mortality, diabetes prevalence and mortality rates could be lower among children of migrants compared to their parents, as they gradually adapt to their new environment [45]. On the other hand, persisting adverse risks might be expected given that children are more likely than their parents to be exposed to pressures that promote faster acculturation to generally ‘obesogenic’ lifestyles.
However, rapid socio-economic change only provides us with a partial explanation for excess migrant diabetes mortality. The mechanisms underlying population variability in type 2 diabetes are much more complex and varied. Physiological, lifestyle and environmental factors are all likely to contribute to the high diabetes mortality rates among migrant groups. A recent study on diabetes in Asia [46] showed that many factors (e.g. lifestyle, genetics and the intrauterine environment) influence the high diabetes prevalence in Asian populations. High insulin resistance and a diabetes-prone body composition appear to be particularly important contributors to the increased diabetes risk in these populations.
Conclusions and recommendations
This study indicates that migrant groups in Europe generally have higher diabetes mortality rates than the local-born populations and that this tendency appears to be more pronounced in migrants coming from less developed countries. This study thus showed that diabetes is an important public health problem in many European migrant populations, which should be taken into account both in health education and medical care.
The substantial variation in diabetes mortality according to COB suggests that there is some heterogeneity in risk factors between different migrant groups. It would be interesting to undertake (within-country) studies that focus on differences in diabetes risk factors by COB. Furthermore, we found large differences in COB-specific diabetes mortality rates according to COR. Research focusing on country contextual variables to determine how country characteristics affect diabetes (mortality) in general and diabetes (mortality) by COB in particular could provide additional insights necessary for the development of policies to reduce inequalities in diabetes (mortality).
Abbreviations
- ASMR:
-
Age-standardized mortality rates
- COB:
-
Country of birth
- COR:
-
County of residence
- GDP:
-
Gross domestic product
- ICD:
-
International classification of diseases
- MRR:
-
Mortality rate ratio
- PY:
-
Person-years at risk
- Q (1Q–4Q):
-
Quartile (first–fourth quartile)
References
Gorus FK, Weets I, Couck P, Pipeleers DG. The Belgian Diabetes Registry. Epidemiology of type 1 and type 2 diabetes. The added value of diabetes registries for conducting clinical studies: the Belgian paradigm. Acta Clin Belg. 2004;59:1–13.
International Diabetes Federation. The diabetes atlas. 4th edn. Brussels: IDF; 2009.
Patel KCR, Bhopal R. Diabetes epidemic in the South Asian Diaspora: action before desperation. J R Soc Med. 2007;100:115–6.
Razum O, Twardella D. Time travel with Oliver Twist—towards an explanation for a paradoxically low mortality among recent immigrants. Trop Med Int Health. 2002;7:4–10.
Swedlund AC, Armelagos GJ, editors. Disease in populations in transition. Anthropological and epidemiological perspectives. New York: Bergin & Garvey; 1990.
Nicolaou M. Diet and overweight perception. An explorative study among Turkish, Moroccan and Surinamese migrants living in the Netherlands [Dissertation]. Amsterdam: Amsterdam Medical Centre; 2009. p 164.
Khlat M, Courbage Y. Mortality and causes of death of Moroccans in France, 1979–91. Population. 1996;8:59–94.
Deboosere P, Gadeyne S. Adult migrant mortality advantage in Belgium: evidence using census and register data. Population. 2005;60:655–98.
Greenhalgh PM. Diabetes in British South Asians: nature, nurture, and culture. Diabet Med. 1997;14:10–18.
Carter JS, Pugh JA, Monterrosa A. Non-insulin dependent diabetes mellitus and ethnic minorities. Ann Intern Med. 1996;125:221–32.
Middelkoop BJC, Kesarlal-Sadhoeram SM, Ramsaransing GN, Struben HWA. Diabetes mellitus among South Asian inhabitants of The Hague: high prevalence and an age-specific socioeconomic gradient. Int J Epidemiol. 1999;28:1119–23.
Uitewaal PJM, Manna DR, Bruijnzeels MA, Hoes AW, Thomas S. Prevalence of type 2 diabetes mellitus, other cardiovascular risk factors and cardiovascular disease in Turkish and Moroccan immigrants in North West Europe: a systematic review. Prev Med. 2004;39:1068–76.
Kriegsman D, van Langen J, Valk G, Stalman W, Boeke J. Hoge prevalentie van diabetes mellitus type 2 bij Turken en Marokkanen. Huisarts Wet. 2003;46:363–368.
Misra A, Ganda OP. Migration and its impact on adiposity and type 2 diabetes. Nutrition. 2007;23:696–708.
Middelkoop BJC. Diabetes: a true trouble. Studies on cardiovascular risk, ethnicity, socioeconomic position and intervention possibilities. [Dissertation]. Amsterdam: Vrije Universiteit Amsterdam; 2001. p 133.
Mather HM, Chaturvedi N, Fuller JH. Mortality and morbidity from diabetes in South Asians and Europeans: 11-year follow-up of the Southall diabetes survey, London, UK. Diabet Med. 1998;15:53–9.
Lanting LC, Joung IM, Mackenbach JP, Lamberts SW, Bootsma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review. Diabetes Care. 2005;28:2280–8.
Kristensen JK, Bak JF, Wittrup I, Lauritzen T. Diabetes prevalence and quality of diabetes care among Lebanese or Turkish immigrants compared to a native Danish population. Prim Care Diabetes. 2007;1:159–65.
Fischbacher CM, Bhopal R, Steiner M, Morris AD, Chalmers J. Is there equity of service delivery and intermediate outcomes in South Asians with type 2 diabetes? Analysis of DARTS database and summary of UK publications. J Publ Health. 2009;31:239–49.
Roca Vilalta M, Castaño Perez A, López Moya C, López Olivares M. Diabetes in a primary care center among Spaniards and immigrants. Pharm Pract. 2006;4:79–82.
Munoko TN, Hermans MP. Phenotypic characterization of first generation Maghrebian migrants with type 2 diabetes. A gender-based comparison with a reference North-Caucasian Belgian cohort. Diabetes Metabol Syndr. 2008;2:115–24.
Landman J, Cruickshank JK. A review of ethnicity, health and nutrition-related diseases in relation to migration in the United Kingdom. Public Health Nutr. 2001;4:647–57.
Harding S. Mortality of migrants from the Caribbean to England and Wales: effect of duration of residence. Int J Epidemiol. 2004;33:382–6.
Harding S, Teyhan A, Maynard MJ, Cruickshank JK. Ethnic differences in overweight and obesity in early adolescence in the MRC DASH study: the role of adolescent and parental lifestyle. Int J Epidemiol. 2008;37:162–72.
Ahmad O, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva: WHO; 2001. p 14.
World Factbook. Country comparison: GDP per capita (PPP); 2003 [cited 9 Oct 2009]. Available from: https://www.cia.gov/library/publications/the-world-factbook.
United Nations Statistics Division. Composition of macro geographical (continental regions), geographical sub-regions, and selected economic and other groupings; 2010 [cited 10 Mar 2010]. Available from: http://unstats.un.org/unsd/methods/m49/m49regin.htm.
Stronks K, Kulu-Glasgow I, Agyemang C. The utility of ‘country of birth’ for the classification of ethnic groups in health research: the Dutch experience. Ethnic Health. 2008;14:3.
Ringbäck-Weitoft G, Gullberg A, Hjern A, Rosén M. Mortality statistics in immigrant research: method for adjusting underestimation of mortality. Int J Epidemiol. 1999;28:756–63.
Meslé F. The registration of causes of death: problems of comparability. In: Wunsch G, Mouchart M, Duchêne J, editors. The life table. Modelling survival and death. Dordrecht: Kluwer; 2002. p. 171–90.
Vauzelle-Kervroëdan F, Delcourt C, Forhan A, Jougla E, Hatton F, Papoz L. Analysis of mortality in French diabetic patients from death certificates: a comparative study. Diabetes Metab. 1999;25:404–11.
Mackenbach JP, Snels IAK, Friden-Kill LM. Diabetes mellitus als doodsoorzaak. Ned Tijdschr Geneeskd. 1991;135:1492–6.
Romon I, Jougla E, Balkau B, Fagot-Campagna A. The burden of diabetes-related mortality in France in 2002: an analysis using both underlying and multiple causes of death. Eur J Epidemiol. 2008;23:327–34.
Mackenbach JP, Kunst AE, Lautenbach H, Oei YB, Bijlsma F. Competing causes of death: a death certificate study. J Clin Epidemiol. 1997;50:1069–77.
Cypher JM, Dietz JL. Measuring economic growth and development. In: Idem, editor. The process of economic development. 2nd ed. Abingdon: Routledge; 2004. p. 28–65.
Malpezzi S. Cross-country patterns of urban development. In: Arnott R, McMillen D, editors. A companion to urban economics. Oxford: Blackwell Publishing; 2006. p. 55–71.
Popkin BM. Urbanization, lifestyle changes and the nutrition transition. World Dev. 1999;27:1905–16.
Espelt A, Borrell C, Roskam AJ. Socioeconomic inequalities in diabetes mellitus across Europe at the beginning of the 21st century. Diabetologia. 2008;51:1971–9.
Nazroo JY. Genetic, cultural or socio-economic vulnerability? Explaining ethnic inequalities in health. Sociol Health Illn. 1998;20:710–30.
Stirbu I, Kunst AE, Bos V, Mackenbach JP. Differences in avoidable mortality between migrants and the native Dutch in the Netherlands. BMC Public Health. 2006;6:78.
Vandenheede H, Deboosere P. Type 2 diabetes in Belgians of Turkish and Moroccan origin. Arch Public Health. 2009;67:62–87.
McBean AM, Li S, Gilbertson DT, Collins AJ. Differences in diabetes prevalence, incidence, and mortality among the elderly of four racial/ethnic groups: Whites, Blacks, Hispanics, and Asians. Diabetes Care. 2004;27:2317–24.
International Diabetes Federation. Prevalence estimates of diabetes mellitus (DM), 2010; 2009 [cited 23 Oct 2009]. Available from: http://www.diabetesatlas.org/content/prevalence-estimates-diabetes-mellitus-dm-2010.
Shkolnikov VM, Cornia GA, Leon DA, Meslé F. Causes of the Russian mortality crisis: evidence and interpretations. World Dev. 1998;26:1995–2011.
Ho L, Bos V, Kunst AE. Differences in cause-of-death patterns between the native Dutch and persons of Indonesian Descent in the Netherlands. Am J Public Health. 2007;97:1616–8.
Ramachandran A, Wan Ma RC, Snehalatha C. Diabetes in Asia. Lancet. 2010;375:408–18.
Acknowledgments
This paper is a product of the EU-funded project Migrant and Ethnic Minority Health Observatory (MEHO) (http://www.meho.eu.com). This research was funded by a PhD grant of the Research Foundation Flanders and by the VUB research council (Geconcerteerde OnderzoeksActie (GOA) 2008 ‘The migration factor. The impact of international migration on migrant communities and on demographic processes and structures in the receiving country’). We are also grateful for the helpful comments of Professor Raj Bhopal and Professor Karien Stronks.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vandenheede, H., Deboosere, P., Stirbu, I. et al. Migrant mortality from diabetes mellitus across Europe: the importance of socio-economic change. Eur J Epidemiol 27, 109–117 (2012). https://doi.org/10.1007/s10654-011-9638-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-011-9638-6