Abstract
Purpose
To assess the frequency and types of chromosomal abnormalities in 204 Ukrainian patients with non-obstructive azoospermia and oligozoospermia and 87 men with normozoospermia.
Methods
Cytogenetic studies were performed on peripheral blood lymphocyte samples of 164 men with oligozoospermia, 40 men with non-obstructive azoospermia and 87 men with normozoospermia attending infertility clinic.
Results
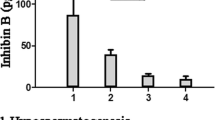
Chromosomal abnormalities were detected in 17 % of patients with sperm disorders: in 35 % of men with azoospermia and in 12.7 % of men with oligozoospermia. The frequency of chromosomal abnormalities in patients with sperm disorders was significantly higher, than in patients with normozoospermia (P = 0.0001). An increase in the incidence of chromosomal abnormalities with the decrease of sperm count was observed. Chromosomal abnormalities were detected in 1.1 % of patients with normozoospermia, 6.5 % of patients with mild oligozoospermia (sperm count 5–15 × 106/ml), 18.4 % of patients with severe oligozoospermia (sperm count <5 × 106/ml) and 35 % of patients with azoospermia. A significant increase in the frequency of chromosomal abnormalities in patients with severe oligozoospermia was observed when compared to mild oligozoospermia (P = 0.01). A statistically significant association (P = 0.02) of chromosomal abnormalities and sex chromosome abnormalities (P = 0.0001) with azoospermia when compared to oligozoospermia was observed.
Conclusions
Our results highlight the importance of cytogenetic studies in patients with oligozoospermia (both mild and severe) and non-obstructive azoospermia. The presence of chromosomal abnormalities influences significantly the fertility treatment protocols, as well as provides a definite diagnosis to couples suffering from infertility.
Similar content being viewed by others
References
World Health Organisation. WHO manual for the standardized investigation and diagnosis of the infertile couple. Cambridge: UK, Cambridge University Press; 2000.
Ferlin A, Raicu F, Gatta V, Zuccarello D, Palka G, Foresta C. Male infertility: role of genetic background. Reprod Biomed Online. 2007;14:734–45.
deKretser DM. Male infertility. Lancet. 1997;349:787–90.
Huynh T, Mollard R, Trounson A. Selected genetic factors associated with male infertility. Hum Reprod Update. 2002;8:183–98.
Baschat AA, Kupker W, al Hasani S, Diedrich K, Schwinger E. Results of cytogenetic analysis in men with severe subfertility prior to intracytoplasmic sperm injection. Hum Reprod. 1996;11:330–3.
Elghezal H, Hidar S, Braham R, Denguezli W, Ajina M, Saad A. Chromosome abnormalities in one thousand infertile males with nonobstructive sperm disorders. Fertil Steril. 2006;86:1792–5.
Gekas J, Thépot F, Turleau C, Siffroi JP, Dadoune JP, Briault S, et al. Chromosomal factors of infertility in candidate couples for ICSI: an equal risk of constitutional aberrations in women and men. Hum Reprod. 2001;16:82–90.
Nielsen J, Wohlert M. Chromosome abnormalities found among 34910 newborn children: results from a 13-year incidence study in Arhus, Denmark. Hum Genet. 1991;87:81–3.
Foresta C, Garolla A, Bartoloni L, Bettella A, Ferlin A. Genetic abnormalities among severely oligospermic men who are candidates for intracytoplasmic sperm injection. J Clin Endocrinol Metab. 2005;90:152–6.
O’Flynn, O’Brien KL, Varghese AC, Agarwal A. The genetic causes of male factor infertility: a review. Fertil Steril. 2010;93:1–12.
Clementini E, Palka C, Iezzi I, Stuppia L, Guanciali-Franchi P, Tiboni GM. Prevalence of chromosomal abnormalities in 2078 infertile couples referred for assisted reproductive techniques. Hum Reprod. 2005;20:437–42.
Georgiou I, Syrrou M, Pardalidis N, Karakitsios K, Mantzavinos T, Giotitsas N, et al. Genetic and epigenetic risks of intracytoplasmic sperm injection method. Asian J Androl. 2006;8:643–73.
World Health Organisation (2010) WHO laboratory manual for the examination and processing of human semen. ed. 5. Geneva, Switzerland.
Kleiman SE, Yogev L, Gamzu R, Hauser R, Botchan A, Lessing JB. Genetic evaluation of infertile men. Hum Reprod. 1999;14:33–8.
Kumtepe E, Beyazyurek C, Cinar C, Ozbey I, Ozkan S, Cetinkaya K, et al. A genetic survey of 1935 Turkish men with severe male factor infertility. Reprod Biomed Online. 2009;18:465–74.
Wang RX, Fu C, Yang YP, Han RR, Dong Y, Dai RL, et al. Male infertility in China: laboratory finding for AZF microdeletions and chromosomal abnormalities in infertile men from Northeastern China. J Assist Reprod Genet. 2010;27:391–6.
Rao KL, Babu KA, Kanakawalli NK, Padmalatha VV, Deenadayal M, Singh L. Prevalence of chromosome defects in azoospermic and oligoastheno-teratozoospermic South Indian infertile men attending an infertility clinic. Reprod Biomed Online. 2006;10:467–72.
Akgul M, Ozkinay F, Ercal D, Cogulu O, Dogan O, Altay B, et al. Cytogenetic abnormalities in 179 cases with male infertility in Western Region of Turkey: report and review. J Assist Reprod Genet. 2009;26:119–22.
Chantot-Bastaraud S, Ravel C, Siffori JP. Underlying karyotype abnormalities in IVF/ICSI patients. Reprod Biomed Online. 2008;16:514–22.
Dul EC, van Ravenswaaij-Arts CMA, Groen H, van Echten-Arends J, Land JA. Who should be screened for chromosomal abnormalities before ICSI treatment? Hum Reprod. 2010;25:2673–7.
Ferlin A, Arredi B, Foresta C. Genetic causes of male infertility. ReprodToxicol. 2006;22:133–41.
Lessing JB. Genetic evaluation of infertile men. Hum Reprod. 1999;14:33–8.
Martin RH. Cytogenetic determinants of male fertility. Hum Reprod Update. 2008;14:379–90.
Yatsenko AN, Yatsenko SA, Weedin JW, Lawrence AE, Patel A, Peacock S, et al. Comprehensive 5-year study of cytogenetic abberations in 668 infertile men. J Urol. 2010;183:1636–42.
Dohle GR, Halley DJ, Van Hemel JO, van den Ouwel AM, Pieters MH, Weber RF, et al. Genetic risk factors in infertile men with severe oligozoospermia and azoospermia. Hum Reprod. 2002;17:13–6.
Dul EC, Groen H, van Ravenswaaij-Arts CMA, Dijkhuizen T, van Echten-Arends LJA. The prevalence of chromosomal abnormalities in subgroups of infertile men. Hum Reprod. 2012;27:36–43.
Van Assche E, Bonduelle M, Tournaye H. Cytogenetics of infertile men. Hum Reprod. 1996;11:1–24.
Maiburg M, Repping S, Giltay J. The genetic origin of Klinefelter syndrome and its effect on spermatogenesis. Fertil Steril. 2012;98:253–60.
Oates RD. The natural history of endocrine function and spermatogenesis in Klinefelter syndrome: what the data show. Fertil Steril. 2012;98:266–73.
Stephenson M, Sierra S. Reproductive outcomes in recurrent pregnancy loss associated with a parental carrier of a structural chromosome rearrangement. Hum Reprod. 2006;21:1076–82.
Anton E, Vidal F, Blanco J. Role of sperm FISH studies in the genetic reproductive advice of structural reorganization carriers. Hum Reprod. 2007;22:2088–92.
Ferfouri F, Selva J, Boitrelle F, Gomes DM, Torre A, Albert M, et al. The chromosomal risk in sperm from heterozygous Robertsonian translocation carriers is related to the sperm count and the translocation type. Fertil Steril. 2011;96:1337–43.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
Results of cytogenetic studies of Ukrainian men with infertility are presented. Increased incidence of chromosomal abnormalities was detected in patients with oligospermia and azoospermia warranting cytogenetic testing for these groups of patients.
Rights and permissions
About this article
Cite this article
Pylyp, L.Y., Spinenko, L.O., Verhoglyad, N.V. et al. Chromosomal abnormalities in patients with oligozoospermia and non-obstructive azoospermia. J Assist Reprod Genet 30, 729–732 (2013). https://doi.org/10.1007/s10815-013-9990-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-013-9990-4