Abstract
Electrocardiogram (ECG) is a standard type of monitoring in intensive care medicine. Several studies suggest that changes in ECG morphology may reflect changes in volume status. The “Brody effect”, a theoretical analysis of left ventricular (LV) chamber size influence on QRS-wave amplitude, is the key element of this phenomenon. It is characterised by an increase in QRS-wave amplitude that is induced by an increase in ventricular preload. This study investigated the influence of changes in intravascular volume status on respiratory variations of QRS-wave amplitudes (ΔECG) compared with respiratory pulse pressure variations (ΔPP), considered as a reference standard. In 17 pigs, ECG and arterial pressure were recorded. QRS-wave amplitude was measured from the Biopac recording to ensure that in all animals ECG electrodes were always at the same location. Maximal QRS amplitude (ECGmax) and minimal QRS amplitude (ECGmin) were determined over one respiratory cycle. ΔECG was calculated as 100 × [(ECGmax − ECGmin)/(ECGmax + ECGmin)/2]. ΔECG and ΔPP were simultaneously recorded. Measurements were performed at different time points: during normovolemic conditions, after haemorrhage (25 mL/kg), and following re-transfusion (25 mL/kg) with constant tidal volume (10 mL/kg) and respiration rate (15 breath/min). At baseline, ΔPP and ΔECG were both <12 %. ΔPP were significantly correlated with ΔECG (r2 = 0.89, p < 0.001). Volume loss induced by haemorrhage increased significantly ΔPP and ΔECG. Moreover, during this state, ΔPP were significantly correlated with ΔECG (r2 = 0.86, p < 0.001). Re-transfusion significantly decreased ΔPP and ΔECG, and ΔPP were significantly correlated with ΔECG (r2 = 0.90, p < 0.001). The observed correlations between ΔPP and ΔECG at each time point of the study suggest that ΔECG is a reliable parameter to estimate the changes in intravascular volume status and provide experimental confirmation of the “Brody effect.”
Similar content being viewed by others
1 Introduction
Electrocardiogram (ECG) is a common type of monitoring in the operating room and in intensive care units. Many studies suggest that changes in ECG morphology could reflect changes in intravascular volume status [1]. The key element of this phenomenon is the ‘‘Brody effect’’, a theoretical analysis of left ventricular (LV) chamber size influence on QRS-wave amplitude. It is characterised by an increase in QRS-wave amplitude that is induced by an increase in ventricular preload [2]. These results in changes in QRS amplitude with mechanical ventilation should be similar to the changes observed with arterial pulse pressure. Clinical studies yielded various results, which may be influenced by various degree of transcutaneous electrical transmission. To validate the concept, we wanted to investigate whether the use of subcutaneous ECG electrodes would result in a high correlation with respiratory pulse pressure variations (ΔPP). This study investigated the influence of changes in intravascular volume status on respiratory variations of QRS-wave amplitude (ΔECG) compared with ΔPP in a haemorrhagic shock pig model.
2 Methods
The experiment has been described in details previously [3]. The results presented here consist of new and unpublished analysis of data from this previous study. For this analysis, we examined data from 17 domestic pigs (mean weight 31.4 ± 3.1 kg) of the 24 animals included in the initial study. Seven pigs were excluded because of technical and measurement issues and two because of the death of the animals. The initial study was approved by the Ethics Committee for Animal Research at the University Medical Centre and by the Cantonal Veterinary Office of Geneva, Switzerland. Animals received respectful care that conferred to the guidelines laid out in the Guide for the Care and Use of Laboratory Animals (Institute of Laboratory Animal Resources, 1996).
Preparation: Animals were premedicated with an intramuscular injection of azaperon 6 mg·kg−1, midazolam 0.5 mg·kg−1, and atropine 0.5 mg. Anesthesia was induced by isoflurane and then maintained by fentanyl 20 μg·kg−1·h−1, isoflurane 1.5–2.0 % and pancuronium 0.4 mg·kg−1·h−1. Ringer’s lactate was administered at 5 mL·kg−1·h−1 to compensate for basal fluid loss. Animals were intubated and mechanically ventilated using a constant-volume respirator (Servo Ventilator 900, Siemens-Elema, Sweden). The fraction of inspired oxygen (FiO2) was set at 0.4. The tidal volume (Vt) was 10 mL·kg−1 with a 2 cm H2O positive end-expiratory pressure (PEEP), and the respiratory rate (RR) was 15 breaths per minute with a fixed inspiratory to expiratory time ratio (I:E = of 1:2). A left carotid arterial catheter advanced into the descending aorta permitted the recording of arterial pressure (AP). The right femoral artery was cannulated for bleeding and the right internal jugular vein was used for re-transfusion. Heart rate and rhythm were recorded with a standard 3-lead electrocardiogram with transcutaneous electrodes. A flow-directed Swan-Ganz catheter (CCOmboV, 7.5F, Edwards Lifesciences™, Irvine, CA) was introduced through the right internal jugular vein and advanced into the pulmonary artery to measure central venous pressure, mean pulmonary artery pressure, pulmonary capillary wedge pressure, continuous cardiac output (CO) and continuous mixed venous saturation.
Experimental protocol: Measurements were performed at baseline under normovolemic conditions. Haemorrhage was then induced by removal of 40 % of the total blood volume (estimated at 7 mL·kg−1 body weight) over a short period of time (5–10 min). The removed blood was kept at body temperature with continuous agitation in blood bags containing citrate–phosphate-dextrose (Baxter AG, Volketswil, Switzerland) and then re-transfused back into the animal during the re-transfusion period. The mean time from the start of bleeding until complete re-transfusion was 49 ± 11 min.
Measurements and calculations: All measurements were made offline from signals stored at a sampling rate of 500 Hz (AcqKnowledge software; Biopac Systems, Santa Barbara, CA) through the analog/digital interface converter (MP100; Biopac Systems, Santa Barbara, CA). All circulatory data were averaged over five breaths. Systolic and diastolic pressures were measured on a beat-by-beat basis, allowing for calculation of pulse pressure. Maximal and minimal pulse pressures within one mechanical breath were determined, and ΔPP was calculated as the difference between the maximal and minimal values over one ventilatory cycle divided by the mean of the two values (expiratory and inspiratory values) [4]. The ΔPP value used for statistical analysis was the average measurement of five consecutive respiratory cycles during the defined circulatory state.
A standard 3-lead electrocardiogram (ECG) was continuously displayed on a Hewlett-Packard monitor (Hewlett-Packard, Andover, MA) with a digital readout of heart rate by trans-cutaneous electrodes. Pin ECG electrodes were stabbed into the skin of the chest wall. In all animals, ECG electrodes were always at the same location. AP and ECG signals were continuously recorded and stored at a sampling rate of 500 Hz (AcqKnowledge software 4.0; Biopac Systems, Santa Barbara, CA). Maximal QRS amplitude (ECGmax) and minimal QRS amplitude (ECGmin) were determined over one respiratory cycle. ΔECG was calculated as 100 × [(ECGmax − ECGmin)/(ECGmax + ECGmin)/2] over one respiratory cycle [5]. The ΔECG value used for statistical analysis was the average measurement of five consecutive respiratory cycles during the defined circulatory state.
2.1 Statistical analysis
To compare haemodynamic parameters at the three time points of the protocol (baseline [B]), after haemorrhage [H], and after re-transfusion [R]), the Wilcoxon signed-rank test was used. A two-tailed unpaired t test with Welch correction was used to compare ΔPP and ΔECG values at each time point of the protocol (B, after H, and after R). Pearson’s correlation coefficient was used to assess correlations between the variation of ΔPP and ΔECG at the three time points of the study. Pearson’s correlation coefficient was also used to assess correlations between CO changes after blood removal and blood removal-induced changes in ΔPP and ΔECG. All values are expressed as mean ± SD or box plots with quartile information. p < 0.05 was considered statistically significant. Analyses were performed using SPSS 18.0 (SPSS, Chicago, IL).
3 Results
Seventeen paralysed, anesthetised pigs were investigated and analysed in this study. Haemodynamic parameters are summarised in the Table 1. At baseline, under normovolemic conditions, ΔPP and ΔECG were both <12 %. ΔPP were significantly correlated with ΔECG (r2 = 0.89, p < 0.001). Volume loss induced by haemorrhage significantly increased ΔPP and ΔECG. Moreover, during this hypovolemic state, ΔPP were significantly correlated with ΔECG (r2 = 0.86, p < 0.001). Re-transfusion permitted a return to a normovolemic state where ΔPP and ΔECG both significantly decreased and ΔPP were significantly correlated with ΔECG (r2 = 0.90, p < 0.001) (Figs. 1, 2a and b).
Simultaneous recording of Airway Pressure (AwP), ECG, and arterial pressure (AP) waveforms in PIG 9. a A recording in a normovolemic state with small parallel respiratory variations of AP and QRS-wave amplitude. b A recording after haemorrhage with large parallel respiratory variations in AP and in QRS-wave amplitude
4 Discussion
The main results of the present study showed available correlations between ΔPP and ΔECG under normovolemic and hypovolemic conditions, meaning that ΔECG is a reliable parameter to estimate the changes in intravascular volume status.
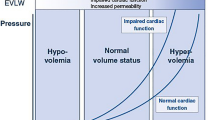
The present analysis suggest that respiratory QRS-wave amplitude variations are highly correlated to respiratory variations in arterial pulse pressure. This new index may have potential applications for fluid responsiveness monitoring in mechanically ventilated patients as cardiopulmonary interactions are habitually used to assess the effects of fluid challenge on stroke volume [6]. Indeed, positive pressure ventilation induces cyclic changes in vena cava blood flow [7], pulmonary artery flow, and aortic blood flow [8]. Since pulse pressure is related to stroke volume and arterial compliance, respiratory variations in pulse pressure reflect respiratory variations in left ventricular stroke volume, if arterial compliance remains stable during a single respiratory cycle [9]. The challenge is now to obtain these dynamic parameters non-invasively [3, 10, 11]; and ΔECG seems to be able to assume this goal and function.
In this sense, the chief contention of this work is to confirm an electrophysiology theory that dates back over 50 years [2]. Our results are in agreement with Brody’s conclusions, which suggest a relation between intra-ventricular blood volume and QRS amplitude [2]. The Brody effect is linked to the heterogeneous composition of the thorax contents. Effectively, the transmission of myocardial depolarisation to the body surface depends on the nature of tissues and corporal fluids interposing between the heart and surface electrodes. In fact, from a biophysical point of view, blood resistivity is lower than myocardial tissue resistivity and even more than lungs one. The more blood stays in the heart, the lower is the global heart resistivity and as a consequence the higher is the heart electric field. Therefore, since the resistivity of the intra-cardiac blood is less than the resistivity of the tissues surrounding the heart, there is an enhancement of the radial and a diminution of the tangential electrical forces that are transmitted to the body surface [5]. Accordingly, a decrease in intra-cardiac volume will lead to a decrease in QRS potentials, while an increase in the volume will increase QRS amplitudes [5].
Thus, respiratory variations in left ventricular preload and stroke volume are the key elements of respiratory QRS-wave amplitude variations because left ventricular chamber size (preload) influences QRS-wave amplitude [2]. However, the present and previous observations [5, 12] highlight that during inspiration, even if there is more air in the thorax, QRS amplitude increases while air should decrease thoracic electric conductivity. This phenomenon is due to fact that during mechanical ventilation before the systole the left ventricle is overfull of blood and then conducts better electricity with an increase of R-wave amplitude. Moreover, based on an anatomical point of view, during inspiration the heart lifts up and the distance between the left ventricle and the chest wall decreases with less air surrounding the cardiac fossa in comparison with the lateral sides of thorax. These facts explain why the magnitude of ΔQRS R-wave on ECG is obviously seen on frontal leads LII and not on V5–V6.
Similarly, the present analysis shows that ΔPP values variations due to changes in volemia were greater than in ΔECG, highlighting by the way that for a same change in volume status, changes in ΔECG are less noticeable than changes in ΔPP. However, this situation is also related to our animal model studied with a severe hemorrhagic shock-induced catecholamine secretion. In this setting, arterial elastance slope increases and magnifies pulse pressure amplitude [9]. In contrary, the heart electric field is unaffected by catecholamine discharge as ΔQRS R-wave on ECG is related to the global heart resistivity which depend from blood resistivity, myocardial tissue resistivity and lungs one and the more blood stays in the heart, higher is amplitude of the QRS wave [13].
Some limitations of this study need to be mentioned. First, many significant influences on the amplitude of the electrocardiographic QRS complex have been described. Changes in the amplitude have been noted in pericardial effusion [14], during myocardial ischemia [15, 16] with QRS axis shifts [17], and changes in intra-myocardial conduction [18]. Conditions causing changes in left ventricular chamber size cause alterations in electrocardiographic waveform amplitude in humans [19]. Second, the authors have not analysed the relationship between QRS amplitude and T wave amplitude as already performed by Pinsky et al. [20]. However, because respiratory cycles induce motion of the heart inside the thoracic cavity, the T wave which is more sensitive to heart position than R wave, may change with movement of heart separately than the Brody effect. Third, haemorrhagic shock produced in our animal study led to a severe hypovolemia [21] that induced a significant increase in the ΔPP, well beyond the usual cut-off level of 13 %. In this sense, as ΔPP changes due to changes in volemia were greater than in ΔECG, we can expect that changes in ΔECG should be less visible if hypovolemia is less important. Fourth, in patients with cardiac arrhythmia, the beat-to-beat variation in stroke volume, and hence in blood pressure, may no longer reflect the effects of mechanical ventilation, making the ΔPP unusable. This is particularly true in patients with atrial fibrillation or frequent extrasystoles [22]. This can be extrapolated to ECG respiratory variations, as QRS-wave amplitude would not be interpretable when arrhythmias occur. Fifth, the method of ECG capture was different in the present animal study. Indeed, we used transcutaneous electrodes while the classical measure of the continuous ECG in patients is performed using epicutaneous electrodes. Finally, this study was not designed to test if ΔECG can predict fluid responsiveness as all animals were fluid responsive between haemorrhage and retransfusion. However, others authors showed that respiratory R-wave variations in lead II (ΔRII) were correlated with respiratory aortic velocity time integral variations (ΔVTI) values in mechanically ventilated patients. Because ΔRII, as ΔPP, can predict ΔVTI >15 %, ΔRII may be useful to predict fluid responsiveness. Further studies testing the ability of ΔECG to predict fluid responsiveness are necessary to validate this new noninvasive dynamic index [12].
5 Conclusion
The observed correlations between ΔPP and ΔECG at each time point of the study suggest that ΔECG is a reliable parameter to estimate the changes in intravascular volume status and provide experimental confirmation of the “Brody effect”. ECG is a non-invasive monitoring universally used in intensive care units and operating rooms. Therefore, more work on the clinical application of this technique merits to be done.
References
Young D, Griffiths J. Clinical trials of monitoring in anaesthesia, critical care and acute ward care: a review. Br J Anaesth. 2006;97(1):39–45. doi:10.1093/bja/ael107.
Brody DA. A theoretical analysis of intracavitary blood mass influence on the heart-lead relationship. Circ Res. 1956;4(6):731–8.
Giraud R, Siegenthaler N, Morel DR, Bendjelid K. Pre-ejection period to estimate cardiac preload dependency in mechanically ventilated pigs submitted to severe hemorrhagic shock. J Trauma. 2011;71(3):702–7. doi:10.1097/TA.0b013e3181f96823.
Michard F, Chemla D, Richard C, Wysocki M, Pinsky MR, Lecarpentier Y, Teboul JL. Clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP. Am J Respir Crit Care Med. 1999;159(3):935–9.
Cannesson M, Keller G, Desebbe O, Lehot JJ. Relations between respiratory changes in R-wave amplitude and arterial pulse pressure in mechanically ventilated patients. J Clin Monit Comput. 2010;24(3):203–7. doi:10.1007/s10877-010-9235-3.
Bendjelid K, Romand JA. Fluid responsiveness in mechanically ventilated patients: a review of indices used in intensive care. Intensive Care Med. 2003;29(3):352–60.
Feissel M, Michard F, Faller JP, Teboul JL. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med. 2004;30(9):1834–7.
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL. Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest. 2001;119(3):867–73.
Giraud R, Siegenthaler N, Bendjelid K. Pulse pressure variation, stroke volume variation and dynamic arterial elastance. Crit Care. 2011;15(2):414. doi:10.1186/cc10088.
Feissel M, Teboul JL, Merlani P, Badie J, Faller JP, Bendjelid K. Plethysmographic dynamic indices predict fluid responsiveness in septic ventilated patients. Intensive Care Med. 2007;33(6):993–9. doi:10.1007/s00134-007-0602-6.
Bendjelid K. The pulse oximetry plethysmographic curve revisited. Curr Opin Crit Care. 2008;14(3):348–53. doi:10.1097/MCC.0b013e3282fb2dc9.
Lorne E, Mahjoub Y, Guinot PG, Fournier Y, Detave M, Pila C, Ben Ammar A, Labont B, Zogheib E, Dupont H. Respiratory variations of R-wave amplitude in lead II are correlated with stroke volume variations evaluated by transesophageal Doppler echocardiography. J Cardiothorac Vasc Anesth. 2012;26(3):381–6. doi:10.1053/j.jvca.2012.01.048.
Soltner C, Dantec R, Lebreton F, Huntzinger J, Beydon L. Changes in R-Wave amplitude in DII lead is less sensitive than pulse pressure variation to detect changes in stroke volume after fluid challenge in ICU patients postoperatively to cardiac surgery. J Clin Monit Comput. 2010;24(2):133–9. doi:10.1007/s10877-010-9221-9.
Eisenberg MJ, de Romeral LM, Heidenreich PA, Schiller NB, Evans GT Jr. The diagnosis of pericardial effusion and cardiac tamponade by 12-lead ECG. A technology assessment. Chest. 1996;110(2):318–24.
David D, Kitchen JG 3rd, Michelson EL, Naito M, Sawin HS, Chen CC. R-wave amplitude responses to rapid atrial pacing: a marker for myocardial ischemia. Am Heart J. 1984;107(1):53–61.
Schick EC Jr, Weiner DA, Hood WB Jr, Ryan TJ. Increase in R-wave amplitude during transient epicardial injury (Prinzmetal type). J Electrocardiol. 1980;13(3):259–66.
Watanabe K, Bhargava V, Froelicher VF. The relationship between exercise-induced R wave amplitude changes and QRS vector loops. J Electrocardiol. 1981;14(2):129–38.
David D, Naito M, Michelson E, Watanabe Y, Chen CC, Morganroth J, Shaffenburg M, Blenko T. Intramyocardial conduction: a major determinant of R-wave amplitude during acute myocardial ischemia. Circulation. 1982;65(1):161–7.
Lekven J, Chatterjee K, Tyberg JV, Parmley WW. Reduction in ventricular endocardial and epicardial potentials during acute increments in left ventricular dimensions. Am Heart J. 1979;98(2):200–6.
Pinsky MR, Gorcsan J 3rd, Gasior TA, Mandarino WA, Deneault LG, Hattler BG, Kunig H. Changes in electrocardiographic morphology reflect instantaneous changes in left ventricular volume and output in cardiac surgery patients. Am J Cardiol. 1995;76(10):667–74.
Wood A, Bendjelid SM, Bendjelid K. Primary aortoenteric fistula: should enhanced computed tomography be considered in the diagnostic work-up? Anesth Analg. 2005;101(4):1157–9.
Michard F. Volume management using dynamic parameters: the good, the bad, and the ugly. Chest. 2005;128(4):1902–3. doi:10.1378/chest.128.4.1902.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giraud, R., Siegenthaler, N., Morel, D.R. et al. Respiratory change in ECG-wave amplitude is a reliable parameter to estimate intravascular volume status. J Clin Monit Comput 27, 107–111 (2013). https://doi.org/10.1007/s10877-012-9405-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-012-9405-6