Abstract
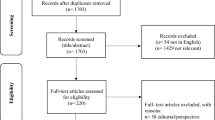
It is well known that information technology (IT) can play a pivotal role in enhancing healthcare quality and patient safety. The use of computational science to enhance the capabilities of hospital information systems helps deliver enhanced healthcare quality. “Smart healthcare” has become a popular term, reflecting the level of IT involvement in healthcare services. However, each hospital has a different level of IT development, and no clear definition of smart healthcare exists. In this study, we aimed to develop and validate a survey standard to evaluate the level of IT involvement in hospitals. The quality improvement task force of the Joint Commission of Taiwan (QITF-JCT) conducted a systematic literature review to identify the key elements of major healthcare IT functions. The modified Delphi technique was used to review the importance and appropriateness of these elements through an expert panel, and the JCT Smart Healthcare Standard version 1.0 (JCT-SHS 1.0) was drafted. A total of 40 healthcare quality improvement campaign (HQIC) application projects in 2018 were selected for evaluating nine key dimensions of hospital functions: security, digitization, automation, interconnection, connectivity, interoperability, mobility, computation, and artificial intelligence. The standard can be used smart hospital evaluation and executed by two experts by on-site evaluation and rating as three-level scale (norm, excellent, and innovative). The internal consistency and inter-rater reliability were investigated using Cronbach’s α and kappa statistics, respectively. This standard was evaluated by using 40 HQIC application projects. The Cronbach’s α values were in the range of 0.74–0.92, indicating the good internal consistency of the JCT-SHS 1.0 among the nine IT dimensions. The kappa correlation coefficients were 0.68 for security (p = 0.027), 0.47 for digitization (p = 0.042), 0.21 for automation (p = 0.048), 0.82 for interconnection (p = 0.014), 0.35 for connectivity (p = 0.036), 0.28 for interoperability (p = 0.042), 0.71 for mobility (p = 0.016), 0.47 for computation (p = 0.029), and 0.34 for artificial intelligence (p = 0.033), revealing moderate inter-rater reliability. The validation data indicated that the JCT-SHS 1.0 is a consistent and reliable instrument for evaluating the levels of IT development in the hospitals. Healthcare providers, external accreditation bodies, and policymakers may use the JCT-SHS 1.0 to assess and plan their organizational and system-wise IT strategy.


Similar content being viewed by others
References
R.O.C, D.o.H., Taiwan Public Health Report. 2010.
PWC, Taiwan health industries - An introductory market overview. 2018: INFOTRUE CO., LTD.
Al Kuwaiti, A., F.A. Al Muhanna, and S. Al Amri, Implementation of Digital Health Technology at Academic Medical Centers in Saudi Arabia. Oman medical journal, 2018. 33(5): p. 367-373.
Alotaibi, Y.K. and F. Federico, The impact of health information technology on patient safety. Saudi Med J, 2017. 38(12): p. 1173-1180.
Haluza, D. and D. Jungwirth, ICT and the future of health care: aspects of health promotion. Int J Med Inform, 2015. 84(1): p. 48-57.
Hemmat, M., et al., Future Research in Health Information Technology: A Review. Perspect Health Inf Manag. 14(Winter): p. 1b, 2017.
Kamei, T., Information and communication technology for home care in the future. Jpn J Nurs Sci, 2013. 10(2): p. 154-61.
Kruse, C.S. and A. Beane, Health Information Technology Continues to Show Positive Effect on Medical Outcomes: Systematic Review. Journal of medical Internet research, 2018. 20(2): p. e41-e41.
Menachemi, N. and T.H. Collum, Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy, 2011. 4: p. 47-55.
Furusa, S.S., A. Coleman, Factors influencing e-health implementation by medical doctors in public hospitals in Zimbabwe. Journal of Information Management, 2018. 20(1): p. a928.
Ancker, J.S., et al., Sociotechnical challenges to developing technologies for patient access to health information exchange data. Journal of the American Medical Informatics Association : JAMIA, 2014. 21(4): p. 664-670.
Keshvari, M., et al., Barriers for the Using of Information Systems in Hospitals: A Qualitative Study. Shiraz E-Med J, 2018. 19(8): e66180.
Pearl, R. 5 Things Preventing Technology Adoption In Health Care. 2014; Available from: https://www.forbes.com/sites/robertpearl/2014/09/11/5-things-preventing-technology-adoption-in-health-care/#33e5de068899.
ENISA, Smart Hospitals. 2016: European Union Agency for Network and Information Security (ENISA).
Shah, S.S. Understanding smart hospitals and why most aren't there yet. 2017.
Sullivan, F., Future of Smart Hospitals. 2017.
Devkaran, S. and P.N. O’Farrell, The impact of hospital accreditation on quality measures: an interrupted time series analysis. BMC Health Serv Res, 2015. 15: p. 137.
Moher, D., et al., Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med, 2009. 151(4): p. 264-9, w64.
Karam, A., Artificial Intelligence in Health Care. 2017.
Timothy Grance, J.H., Peck, S., Smith, J., Korow-Diks, K., Security Guide for Interconnecting Information Technology Systems. NIST Special Publication (NIST SP), p. 800-47, 2002.
Andersen, B., et al., Connecting the clinical IT infrastructure to a service-oriented architecture of medical devices. Biomed Tech (Berl), 2018. 63(1): p. 57-68.
HIMSS, HIMSS Dictionary of Healthcare Information Technology Terms, Acronyms and Organizations. 2nd ed. 2010.
Donner, A. and M. Eliasziw, A goodness-of-fit approach to inference procedures for the kappa statistic: confidence interval construction, significance-testing and sample size estimation. Stat Med, 1992. 11(11): p. 1511-9.
APA: Arifin, W.N. Sample size calculator (web). 2021; Available from: http://wnarifin.github.io.
McHugh, M.L., Interrater reliability: the kappa statistic. Biochem Med (Zagreb), 2012. 22(3): p. 276-82.
Devers, K.J., H.H. Pham, and G. Liu, What is driving hospitals' patient-safety efforts? Health Aff (Millwood), 2004. 23(2): p. 103-15.
Longo, D.R., et al., Hospital patient safety: characteristics of best-performing hospitals. J Healthc Manag, 2007. 52(3): p. 188-204; discussion 204-5.
Funding
This study was funded by the JCT’s annual HQIC grant.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Education & Training
Rights and permissions
About this article
Cite this article
Liao, HH., Rau, HH., Hsu, PC. et al. Development of the Joint Commission of Taiwan’s Smart Healthcare Standard. J Med Syst 45, 67 (2021). https://doi.org/10.1007/s10916-021-01738-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-021-01738-3