ABSTRACT
Purpose
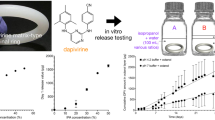
Progering® is the only intravaginal ring intended for contraception therapies during lactation. It is made of silicone and releases progesterone through the vaginal walls. However, some drawbacks have been reported in the use of silicone. Therefore, ethylene vinyl acetate copolymer (EVA) was tested in order to replace it.
Methods
EVA rings were produced by a hot-melt extrusion procedure. Swelling and degradation assays of these matrices were conducted in different mixtures of ethanol/water. Solubility and partition coefficient of progesterone were measured, together with the initial hormone load and characteristic dimensions. A mathematical model was used to design an EVA ring that releases the hormone at specific rate.
Results
An EVA ring releasing progesterone in vitro at about 12.05 ± 8.91 mg day−1 was successfully designed. This rate of release is similar to that observed for Progering®. In addition, it was observed that as the initial hormone load or ring dimension increases, the rate of release also increases. Also, the device lifetime was extended with a rise in the initial amount of hormone load.
Conclusions
EVA rings could be designed to release progesterone in vitro at a rate of 12.05 ± 8.91 mg day−1. This ring would be used in contraception therapies during lactation. The use of EVA in this field could have initially several advantages: less initial and residual hormone content in rings, no need for additional steps of curing or crosslinking, less manufacturing time and costs, and the possibility to recycle the used rings.








Similar content being viewed by others
REFERENCES
Shah B, Surti N, Misra A. 12 - Other routes of protein and peptide delivery: transdermal, topical, uterine, and rectal. In: Ambikanandan M, editor. Challenges in delivery of therapeutic genomics and proteomics. London: Elsevier; 2011. p. 623–71.
Richardson JL, Illum L. (D) Routes of delivery: Case studies: (8) The vaginal route of peptide and protein drug delivery. Adv Drug Deliv Rev. 1992;8(2–3):341–66.
Hussain A, Ahsan F. The vagina as a route for systemic drug delivery. J Control Release. 2005;103(2):301–13.
das Neves J, Bahia MF. Gels as vaginal drug delivery systems. Int J Pharm. 2006;318(1–2):1–14.
Vermani K, Garg S. The scope and potential of vaginal drug delivery. Pharm Sci Technol Today. 2000;3(10):359–64.
Woolfson AD, Elliott GRE, Gilligan CA, Passmore CM. Design of an intravaginal ring for the controlled delivery of 17β-estradiol as its 3-acetate ester. J Control Release. 1999;61:319–28.
Morrow RJ, Woolfson AD, Donnelly L, Curran R, Andrews G, Katinger D, et al. Sustained release of proteins from a modified vaginal ring device. Eur J Pharm Biopharm. 2011;77(1):3–10.
Helbling IM, Cabrera MI, Luna JA. Mathematical modeling of drug delivery from one-layer and two-layer torus-shaped devices with external mass transfer resistance. Eur J Pharm Sci. 2011;44:288–98.
Helbling IM, Ibarra JCD, Luna JA. Application of the refined integral method in the mathematical modeling of drug delivery from one-layer torus-shaped devices. Int J Pharm. 2012;423:240–6.
Helbling IM, Luna JA, Cabrera MI. Mathematical modeling of drug delivery from torus-shaped single-layer devices. J Control Release. 2011;149:258–63.
Greemblatt RB. The physiologic effectiveness of progesterone vaginal suppositories. J Clin Endocrinol Metab. 1954;14(12):1564–7.
Widholm O, Vartiainen E. The absorption of conjugated estrogens and sodium estrone sulfate from the vagina. Ann Chir Gynecol Fenn. 1974;63:186–90.
Roumen FJME, Dieben TOM. Clinical acceptability of an ethylene-vinyl-acetate nonmedicated vaginal ring. Contraception. 1999;59(1):59–62.
Sivin I, Mishell DR, Victor A, Diaz S, Alvarez-Sanchez F, Nielsen NC, et al. A multicenter study of levonorgestrel—estradiol contraceptive vaginal rings II—subjective and objective measures of effects: an international comparative trial. Contraception. 1981;24(4):359–76.
Abbasi F, Mirzadeh H, Katbab A-A. Modification of polysiloxane polymers for biomedical applications: a review. Polym Int. 2001;50(12):1279–87.
Nikolaev OO, Urhanovl VB, Pavlovich V, Babaev AD, Bogdanov VV, Mirzadeh H. A thermoplastic rubber composition for medical purposes. Iran Polym J. 2001;10:9–14.
Robb WL. Thin silicone membranes—their permeation properties and some applications. Ann N Y Acad Sci. 1968;146(1):119–37.
Bates BL, Ragheb AO, Stewart JM, Bourdeau WJ, Choules BD, Purdy JD, et al, inventors; Coated implantable medical device. 2005.
Heredia V, Bianco ID, Tríbulo H, Cuesta G, Chesta P, Bó GA, et al. Room temperature vulcanizing silicone sheaths on a reusable support for progesterone delivery in estrous synchronization treatments in cattle. Anim Reprod Sci. 2008;108(3–4):356–63.
van Laarhoven JAH, Kruft MAB, Vromans H. In vitro release properties of etonogestrel and ethinyl estradiol from a contraceptive vaginal ring. Int J Pharm. 2002;232(1–2):163–73.
Novák A, de la Loge C, Abetz L, van der Meulen EA. The combined contraceptive vaginal ring, NuvaRing®: an international study of user acceptability. Contraception. 2003;67(3):187–94.
Kolacki C, Rocco V. The combined vaginal contraceptive ring, NuvaRing, and cerebral venous sinus thrombosis: a case report and review of the literature. J Emerg Med. 2012;42(4):413–6.
Ahrendt H-J, Nisand I, Bastianelli C, Gómez MA, Gemzell-Danielsson K, Urdl W, et al. Efficacy, acceptability and tolerability of the combined contraceptive ring, NuvaRing, compared with an oral contraceptive containing 30 μg of ethinyl estradiol and 3 mg of drospirenone. Contraception. 2006;74(6):451–7.
Oddsson K, Leifels-Fischer B, de Melo NR, Wiel-Masson D, Benedetto C, Verhoeven CHJ, et al. Efficacy and safety of a contraceptive vaginal ring (NuvaRing) compared with a combined oral contraceptive: a 1-year randomized trial. Contraception. 2005;71(3):176–82.
Nash HA, Alvarez-Sanchez F, Mishell Jr DR, Fraser IS, Maruo T, Harmon TM. Estradiol-delivering vaginal rings for hormone replacement therapy. Am J Obstet Gynecol. 1999;181(6):1400–6.
Nash HA, Brache V, Alvarez-Sanchez F, Jackanicz TM, Harmon TM. Estradiol delivery by vaginal rings: potential for hormone replacement therapy. Maturitas. 1997;26(1):27–33.
Malcolm RK, Edwards K-L, Kiser P, Romano J, Smith TJ. Advances in microbicide vaginal rings. Antivir Res. 2010;88(Supplement(0)):S30–9.
Han YA, Singh M, Saxena BB. Development of vaginal rings for sustained release of nonhormonal contraceptives and anti-HIV agents. Contraception. 2007;76(2):132–8.
Brache V, Faundes A. Contraceptive vaginal rings: a review. Contraception. 2010;82(5):418–27.
Brache V, Sitruk-Ware R, Williams A, Blithe D, Croxatto H, Kumar N, et al. Effects of a novel estrogen-free, progesterone receptor modulator contraceptive vaginal ring on inhibition of ovulation, bleeding patterns and endometrium in normal women. Contraception. 2012;85(5):480–8.
Johansson EDB, Sitruk-Ware R. New delivery systems in contraception: vaginal rings. Am J Obstet Gynecol. 2004;190(4, Supplement):S54–9.
Kerns J, Darney P. Vaginal ring contraception. Contraception. 2011;83(2):107–15.
Landgren BM, Aedo AR, Johannisson E, Cekan SZ. Studies on a vaginal ring releasing levonorgestrel at an initial rate of 27 μg/24h when used alone or in combination with transdermal systems releasing estradiol. Contraception. 1994;50(1):87–100.
Rad M, Kluft C, Ménard J, Burggraaf J, de Kam ML, Meijer P, et al. Comparative effects of a contraceptive vaginal ring delivering a nonandrogenic progestin and continuous ethinyl estradiol and a combined oral contraceptive containing levonorgestrel on hemostasis variables. Am J Obstet Gynecol. 2006;195(1):72–7.
Roumen FJME. The contraceptive vaginal ring compared with the combined oral contraceptive pill: a comprehensive review of randomized controlled trials. Contraception. 2007;75(6):420–9.
Sivin I, Díaz S, Croxatto HB, Miranda P, Shaaban M, Sayed EH, et al. Contraceptives for lactating women: A comparative trial of a progesterone-releasing vaginal ring and the Copper T 380A IUD. Contraception. 1997;55(4):225–32.
Terrell LR, Tanner AE, Hensel DJ, Blythe MJ, Fortenberry JD. Acceptability of the vaginal contraceptive ring among adolescent women. J Pediatr Adolesc Gynecol. 2011;24(4):204–10.
Weisberg E, Fraser IS, Lacarra M, Mishell Jr DR, Jackanicz T. Effect of different insertion regimens on side effects with a combination contraceptive vaginal ring. Contraception. 1997;56(4):233–9.
Díaz S, Zepeda A, Maturana X, Reyes MV, Miranda P, Casado ME, et al. Fertility regulation in nursing women: IX. Contraceptive performance, duration of lactation, infant growth, and bleeding patterns during use of progesterone vaginal rings, progestin-only pills, Norplant® implants, and Copper T 380-A intrauterine devices. Contraception. 1997;56(4):223–32.
Massai R, Miranda P, Valdés P, Lavı́n P, Zepeda A, Casado ME, et al. Preregistration study on the safety and contraceptive efficacy of a progesterone-releasing vaginal ring in Chilean nursing women. Contraception. 1999;60(1):9–14.
Nath A, Sitruk-Ware R. Progesterone vaginal ring for contraceptive use during lactation. Contraception. 2010;82(5):428–34.
Siepmann J, Siepmann F. Mathematical modeling of drug delivery. Int J Pharm. 2008;364(2):328–43.
Siepmann J, Siepmann F. Modeling of diffusion controlled drug delivery. J Control Release. 2012;161(2):351–62.
Moharram AK, Shefee T. Role of mathematical modeling in controlled drug delivery. J Sci Res. 2009;1:539–50.
Chien YW, Lambert HJ, Grant DE. Controlled drug release from polymeric devices I: technique for rapid in vitro release studies. J Pharm Sci. 1974;63(3):365–9.
Matlin SA, Belenguer A, Hall PE. Progesterone-releasing vaginal rings for use in postpartum contraception. I. In vitro release rates of progesterone from core-loaded rings. Contraception. 1992;45(4):329–41.
Jackanicz TM. Levonorgestrel and estradiol release from an improved contraceptive vaginal ring. Contraception. 1981;24(4):323–39.
International A. ASTM D570, Standard test method for water absorption of plastics. West Conshohocken, PA. 1998.
Tang M, Hou J, Lei L, Liu X, Guo S, Wang Z, et al. Preparation, characterization and properties of partially hydrolyzed ethylene vinyl acetate copolymer films for controlled drug release. Int J Pharm. 2010;400:66–73.
Pereira GR, Marchetti JM, Bentley MVLB. A rapid method for determination of progesterone by reversed-phase liquid chromatography from aqueous media. Anal Lett. 2000;33:881–9.
Wenhui D. Mechanism of diffusion of progesterone through ethylene vinyl acetate copolymer. J China Pharmaceut Univ. 1987;18:87–90.
Malcolm K, Woolfson D, Russell J, Tallon P, McAuley L, Craig D. Influence of silicone elastomer solubility and diffusivity on the in vitro release of drugs from intravaginal rings. J Control Release. 2003;90:217–25.
Russell JA, Malcolm RK, Campbell K, Woolfson AD. High-performance liquid chromatographic determination of 17β-estradiol and 17β-estradiol-3-acetate solubilities and diffusion coefficients in silicone elastomeric intravaginal rings. J Chromatogr B. 2000;744:157–63.
Costa P, Sousa Lobo JM. Modeling and comparison of dissolution profiles. Eur J Pharm Sci. 2001;13:123–33.
Moore JW, Flanner HH. Mathematical comparison of dissolution profiles. Pharm Technol. 1996;20:64–74.
Pillay V, Fassihi R. Evaluation and comparison of dissolution data derived from different modified release dosage forms: an alternative method. J Control Release. 1998;55:45–55.
Chien YW. Fundamentals of controlled-release drug administration. Swarbrick J, editor. New York: Marcel Dekker Inc; 1982.
Bunt CR, Rathbone MJ, Burggraaf S, C.R. O, editors. Development of a QC release assessment method for a physically large veterinary product containing a highly water insoluble drug and the effect of formulation variables upon release. Proceed International Symp Control Rel Bioact Mater; 1997.
Nandi I, Bateson M, Bari M, Joshi HN. Synergistic effect of PEG-400 and Cyclodextrin to enhance solubility of Progesterone. AAPS Pharm Sci Technol. 2003;4:1–5.
Papadokostaki KG, Petropoulos JH. Kinetics of release of a model disperse dye from supersaturated cellulose acetate matrices. J Control Release. 1998;54(3):251–64.
Bird RB, Stewart WE, Lightfoot EN. Fenómenos de transporte: un estudio sistemático de los fundamentos del transporte de materia, energía y cantidad de movimiento. Barcelona: Ed. Reverté; 1995.
Mazan J, Leclerc B, Porte H, Torres G, Couarraze G. Influence of network characterisitics on diffusion in silicone elastomer. J Mater Sci Mater Med. 1993;4(2):175–8.
Helbling IM, Ibarra JCD, Luna JA, Cabrera MI, Grau RJA. Modeling of dispersed-drug delivery from planar polymeric systems: optimizing analytical solutions. Int J Pharm. 2010;400(1–2):131–7.
Helbling IM, Ibarra JCD, Luna JA, Cabrera MI, Grau RJA. Modeling of drug delivery from erodible and non-erodible laminated planar devices into a finite external medium. J Membr Sci. 2010;350(1–2):10–8.
Brache V, Payán LJ, Faundes A. Current status of contraceptive vaginal rings. Contraception. 2013;87(3):264–72.
Narasimhan B, Langer R. Zero-order release of micro- and macromolecules from polymeric devices: the role of the burst effect. J Control Release. 1997;47(1):13–20.
Sheikh Hassan A, Sapin A, Lamprecht A, Emond E, El Ghazouani F, Maincent P. Composite microparticles with in vivo reduction of the burst release effect. Eur J Pharm Biopharm. 2009;73(3):337–44.
Xiang A, McHugh AJ. Quantifying sustained release kinetics from a polymer matrix including burst effects. J Membr Sci. 2011;371(1–2):211–8.
Alexander NJ, Arkin ES, Einhaus KB, Singh M, Thompson MM. Results of a patient acceptance survey administered to women in the NuvaRing Premier Program. Obstet Gynecol. 2003;101(4, Supplement):S16–7.
Fine PM, Meyers N, Tryggestad J. Patient satisfaction with the use of nuvaring after surgical or medical abortion. Contraception. 2005;72(3):232.
Liu KE, Alhajri M, Greenblatt E. A randomized controlled trial of NuvaRing versus combined oral contraceptive pills for pretreatment in in vitro fertilization cycles. Fertil Steril. 2011;96(3):605–8.
Mulders TMT, Dieben TOM. Use of the novel combined contraceptive vaginal ring NuvaRing for ovulation inhibition. Fertil Steril. 2001;75(5):865–70.
ACKNOWLEDGMENTS AND DISCLOSURES
The authors wish to express their gratitude to Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), and to Universidad Nacional del Litoral (UNL) of Argentina, for the financial support granted to this contribution.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 33 kb)
Rights and permissions
About this article
Cite this article
Helbling, I.M., Ibarra, J.C.D. & Luna, J.A. The Optimization of an Intravaginal Ring Releasing Progesterone Using a Mathematical Model. Pharm Res 31, 795–808 (2014). https://doi.org/10.1007/s11095-013-1201-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-013-1201-6