Abstract
Objective
The aim of this study is to evaluate the impact of rapid palatal expansion (RPE) on the nasal airway subjectively by utilizing patient-reported outcome measures (PROM) and objectively by evaluating validated internal nasal valve (INV) measurements obtained from cone beam computed tomography (CBCT) in pediatrics.
Materials and methods
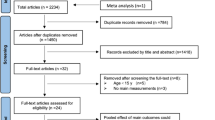
In this retrospective cohort study, subjects who underwent RPE from March to December 2018 with cone beam CT and Nasal Obstruction Symptom Evaluation (NOSE) scores were included. Exclusion criteria included craniofacial deformity, allergies, asthma, recent nasal trauma, or surgery. INV measurements (angle and cross-sectional area), diastema, midpalatal suture opening, and NOSE scores were evaluated.
Results
Fifty-one subjects met the inclusion criteria with a mean age of 10.1 ± 2.6. Pre-expansion mean NOSE score was 32.55 (moderate) while post-expansion was 13.92 (mild). Mean NOSE score improved significantly by an average of 18.63 following post-expansion (P < 0.0001). The patients’ right and left INV angles increased significantly by a mean of 2.42° and 2.65° respectively (P < 0.0001). Right and left INV cross-sectional areas increased significantly by an average of 14.35 mm2 (P < 0.0001) and 14.17 mm2 (P < 0.0001) respectively. An average expansion of the diastema and the suture was 1.60 mm and 3.05 mm respectively (P < 0.0001), with an average of 6.29 mm of expansion. We found the amount of diastema expansion to correlate with change in NOSE score (R = − 0.32, P = 0.022). Age and diastema showed a negative correlation (R = − 0.44, P = 0.0019), while INV angle and diastema showed a statistically significant positive correlation (R = 0.28, P = 0.048).
Conclusions
RPE showed improvement in both NOSE scores and objective measures of the INV. This may show the possibility of considering RPE in managing resistant pediatric nasal airways. Future studies should include collaboration with pediatric otolaryngologists, with the inclusion of pediatric patients with persistent nasal obstruction.






Similar content being viewed by others
References
Hsu DW, Suh JD (2018) Anatomy and physiology of nasal obstruction. Otolaryngol Clin N Am 51:853–865. https://doi.org/10.1016/j.otc.2018.05.001
Schuman TA, Senior BA (2018) Treatment paradigm for nasal airway obstruction. Otolaryngol Clin N Am 51:873–882. https://doi.org/10.1016/j.otc.2018.05.003
Awad MI, Kacker A (2018) Nasal obstruction considerations in sleep apnea. Otolaryngol Clin N Am 51:1003–1009. https://doi.org/10.1016/j.otc.2018.05.012
Miman MC, Deliktaş H, Özturan O, Toplu Y, Akarçay M (2006) Internal nasal valve: revisited with objective facts. Otolaryngol Head Neck Surg. https://doi.org/10.1016/j.otohns.2005.08.027
Bloom JD, Sridharan S, Hagiwara M, Babba JS, White WM, Constantinides M (2012) Reformatted computed tomography to assess the internal nasal valve and association with physical examination. Arch Facial Plast Surg. https://doi.org/10.1001/archfacial.2012.50
Pirelli P, Saponara M, Guilleminault C (2012) Rapid maxillary expansion before and after adenotonsillectomy in children with obstructive sleep apnea Forcierte Gaumennahterweiterung vor und nach Adenotonsillektomie bei Kindern mit obstruktiver Schlafapnoe, Somnologie - Schlafforsch. Und Schlafmedizin. https://doi.org/10.1007/s11818-012-0560-2
Villa MP, Rizolli A, Miano S, Malagola C (2011) Efficacy of rapid maxillary expansion in children with obstructive sleep apnea syndrome: 36 months of follow-up. Sleep Breath. https://doi.org/10.1007/s11325-011-0505-1LK
Lotfi V, Ghoneima A, Lagravere M, Kula K, Stewart K (2018) Three-dimensional evaluation of airway volume changes in two expansion activation protocols. Int Orthod 16:144–157. https://doi.org/10.1016/j.ortho.2018.01.001
Christie KF, Boucher N, Chung CH (2010) Effects of bonded rapid palatal expansion on the transverse dimensions of the maxilla: a cone-beam computed tomography study. Am J Orthod Dentofac Orthop. https://doi.org/10.1016/j.ajodo.2008.11.024
El H, Palomo JM (2014) Three-dimensional evaluation of upper airway following rapid maxillary expansion A CBCT study. Angle Orthod. https://doi.org/10.2319/012313-71.1
Oliveira De Felippe NL, Da Silveira AC, Viana G, Kusnoto B, Smith B, Evans CA (2008) Relationship between rapid maxillary expansion and nasal cavity size and airway resistance: short- and long-term effects. Am J Orthod Dentofac Orthop. https://doi.org/10.1016/j.ajodo.2006.10.034
Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT (2004) Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) Scale. Otolaryngol Head Neck Surg. https://doi.org/10.1016/j.otohns.2003.09.016
Camacho M, Zaghi S, Certal V, Abdullatif J, Means C, Acevedo J, Liu S, Brietzke SE, Kushida CA, Capasso R (2015) Inferior turbinate classification system, grades 1 to 4: development and validation study. Laryngoscope. https://doi.org/10.1002/lary.24923
Poetker DM, Rhee JS, Mocan BO, Michel MA (2004) Computed tomography technique for evaluation of the nasal valve. Arch Facial Plast Surg. https://doi.org/10.1001/archfaci.6.4.240
Abdelwahab M, Yoon A, Okland T, Poomkonsarn S, Gouveia C, Liu SY-C (2019) Impact of distraction osteogenesis maxillary expansion on the internal nasal valve in obstructive sleep apnea. Otolaryngol Neck Surg 019459981984280:362–367. https://doi.org/10.1177/0194599819842808
Abdelwahab MA, Neves CA, Patel PN, Most SP (2020) Impact of dorsal preservation rhinoplasty versus dorsal hump resection on the internal nasal valve : a quantitative radiological study. Aesthet Plast Surg. https://doi.org/10.1007/s00266-020-01627-z
Lipan MJ, Most SP (2013) Development of a severity classification system for subjective nasal obstruction. JAMA Facial Plast Surg. https://doi.org/10.1001/jamafacial.2013.344
Cicchetti DV, Nelson LD (1994) Re-examining threats to the reliability and validity of putative brain-behavior relationships: new guidelines for assessing the effect of patients lost to follow-up. J Clin Exp Neuropsychol 16:339–343. https://doi.org/10.1080/01688639408402644
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. https://doi.org/10.1016/j.jcm.2016.02.012
Vaezeafshar R, Moubayed SP, Most SP (2018) Repair of lateral wall insufficiency. JAMA Facial Plast Surg. https://doi.org/10.1001/jamafacial.2017.0718
Samra S, Steitz JT, Hajnas N, Toriumi DM (2018) Surgical management of nasal valve collapse. Otolaryngol Clin N Am 51:929–944. https://doi.org/10.1016/j.otc.2018.05.009
Abdelwahab M, Most S (2020) The miniature lateral crural strut graft: efficacy of a novel technique in tip plasty. Laryngoscope. https://doi.org/10.1002/lary.28530
Smith MM, Ishman SL (2018) Pediatric nasal obstruction. Otolaryngol Clin N Am 51:971–985. https://doi.org/10.1016/j.otc.2018.05.005
Most SP, Rudy SF (2017) Septoplasty: basic and advanced techniques. Facial Plast Surg Clin North Am 25:161–169. https://doi.org/10.1016/j.fsc.2016.12.002
Funamura JL, Sykes JM (2014) Pediatric septorhinoplasty. Facial Plast Surg Clin North Am. https://doi.org/10.1016/j.fsc.2014.07.005
Baccetti T, Mucedero M, Leonardi M, Cozza P (2009) Interceptive treatment of palatal impaction of maxillary canines with rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofac Orthop. https://doi.org/10.1016/j.ajodo.2008.03.019
Baccetti T, Franchi L, Cameron CG, McNamara JA (2001) Treatment timing for rapid maxillary expansion. Angle Orthod. https://doi.org/10.1043/0003-3219(2001)071<0343:TTFRME>2.0.CO;2
Haralambidis A, Ari-Demirkaya A, Acar A, Küçükkeleş N, Ateş M, Özkaya S (2009) Morphologic changes of the nasal cavity induced by rapid maxillary expansion: a study on 3-dimensional computed tomography models. Am J Orthod Dentofac Orthop. https://doi.org/10.1016/j.ajodo.2008.03.020
Kim SY, Park YC, Lee KJ, Lintermann A, Han SS, Yu HS, Choi YJ (2018) Assessment of changes in the nasal airway after nonsurgical miniscrew-assisted rapid maxillary expansion in young adults. Angle Orthod. https://doi.org/10.2319/092917-656.1
Rohra AK, Demko CA, Hans MG, Rosen C, Palomo JM (2018) Sleep disordered breathing in children seeking orthodontic care. Am J Orthod Dentofac Orthop. https://doi.org/10.1016/j.ajodo.2017.11.027
Williams R, Patel V, Chen YF, Tangbumrungtham N, Thamboo A, Most SP, Nayak JV, Liu SYC (2019) The upper airway nasal complex: structural contribution to persistent nasal obstruction. Otolaryngol - Head Neck Surg (United States). https://doi.org/10.1177/0194599819838262
Din H, Bundogji N, Leuin SC (2019) Psychometric evaluation of the nasal obstruction symptom evaluation scale for pediatric patients. Otolaryngol - Head Neck Surg (United States). https://doi.org/10.1177/0194599819890835
Çakmak Ö, Coşkun M, Çelik H, Büyüklü F, Özlüoǧlu LN (2003) Value of acoustic rhinometry for measuring nasal valve area. Laryngoscope. https://doi.org/10.1097/00005537-200302000-00018
De Felice F, Di Carlo G, Saccucci M, Tombolini V, Polimeni A (2019) Dental cone beam computed tomography in children: clinical effectiveness and cancer risk due to radiation exposure. Oncology. https://doi.org/10.1159/000497059
Ng BA, Ramsey RG, Corey JP (1999) The distribution of nasal erectile mucosa as visualized by magnetic resonance imaging. Ear, Nose Throat J. https://doi.org/10.1177/014556139907800309
Cole P, Haight JSJ, Cooper PW, Kassel EE (1983) A computed tomographic study of nasal mucosa: effects of vasoactive substances. J Otolaryngol 12(1):58–60
Saunders MW, Jones NS, Kabala J, Lowe J (1995) An anatomical, histological and magnetic resonance imaging study of the nasal septum. Clin Otolaryngol Allied Sci 20:434–438. https://doi.org/10.1111/j.1365-2273.1995.tb00077.x
Wexler D, Braverman I, Amar M (2006) Histology of the nasal septal swell body (septal turbinate). Otolaryngol Head Neck Surg. https://doi.org/10.1016/j.otohns.2005.10.058
Bishara SE, Staley RN (1987) Maxillary expansion: clinical implications. Am J Orthod Dentofac Orthop. https://doi.org/10.1016/0889-5406(87)90202-2
Acknowledgments
The authors would like to thank Dr. Myung Shim Sim for her valuable statistical assistance.
Author information
Authors and Affiliations
Contributions
All authors have seen and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This retrospective study was approved by University of California, Los Angeles Institutional Review Board (IRB#18-001326).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yoon, A., Abdelwahab, M., Liu, S. et al. Impact of rapid palatal expansion on the internal nasal valve and obstructive nasal symptoms in children. Sleep Breath 25, 1019–1027 (2021). https://doi.org/10.1007/s11325-020-02140-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02140-y