Abstract
Introduction
Surgical resection is the only option for long-term survival in patients with hilar cholangiocarcinoma (HC), but it is associated with high morbidity and mortality. The aim of the present study was to prospectively assess the perioperative management and short-term outcomes of surgical treatment of HC in a recent, multi-institutional study with a short inclusion period.
Methods
Between January and December 2008, a register prospectively collected data on patients operated on for HC (exploratory or curative surgery) in eight tertiary centers. The register focused on perioperative management, resectability, surgical procedures employed, morbidity, and mortality. The study cohort consisted of 56 patients (40 men and 16 women) with a median age of 63 years (range, 33–83 years).
Results
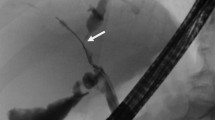
Among the 56 patients, 47 (84%) were jaundiced and 42 (75%) tumors were classified as Bismuth–Corlette type III–IV. Nine patients (16%) underwent staging laparoscopy and four (7%) received neoadjuvant chemotherapy. Preoperative biliary drainage (endoscopy, 42%) was performed in 38 (81%) jaundiced patients and portal vein embolization (right side, 83%) was performed prior to surgery in 18 patients (32%). Among these 56 patients, curative resection was achieved in 39 (70%). All underwent major liver resection (>3 segments), bile duct resection, and lymphadenectomy. Thirteen patients (36%) underwent portal vein resection, one of whom also required pancreaticoduodenectomy. Eighty-two percent of resected patients (n = 32) had no proof of malignancy prior to hepatectomy. Clear surgical margins were obtained in 77% (n = 30). The postoperative mortality was 8% and complications occurred in 72% of the resected patients. Seven (25%) patients required reoperation, and 15 (54%) patients required percutaneous drainage. In a univariate analysis, the risk factors for morbidity were intraoperative blood transfusion (p = 0.009) and vascular clamping (p = 0.006). The median length of hospitalization was 20 ± 13 days.
Conclusion
Curative resection for HC is associated with a high rate of R0 resection. However, surgery is associated with high levels of morbidity and mortality, despite intensive perioperative management.
Similar content being viewed by others
Abbreviations
- HC:
-
Hilar cholangiocarcinoma
- PVE:
-
Portal vein embolization
- SD:
-
Standard deviation
References
Seyama Y, Kubota K, Sano K, Noie T, Takayama T, Kosuge T, et al. Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg. 2003;238:73–83.
Launois B, Reding R, Lebeau G, Buard JL. Surgery for hilar cholangiocarcinoma : French experience in a collective survey of 552 extrahepatic bile duct cancers. J Hepatobiliary Pancreat Surg 2000;7:128-34.
Nishio H, Nagino M, Nimura Y. Surgical management of hilar cholangiocarcinoma: the Nagoya experience. HPB (Oxford) 2005;7:259–62.
Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg 1999;230:808–18.
Kondo S, Katoh H, Hirano S, Ambo Y, Tanaka E, Okushiba S. Portal vein resection and reconstruction prior to hepatic dissection during right hepatectomy and caudate lobectomy for hepatobiliary cancer. Br J Surg 2003;90:694–7.
Nagino M, Kamiya J, Nishio H, Ebata T, Arai T, Nimura Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg 2006;243:364–72.
Ferrero A, Lo Tesoriere R, Vigano` L, Caggiano L, Sgotto E, Capussotti L. Preoperative biliary drainage increases infectious complications after hepatectomy for proximal bile duct tumor obstruction. World J Surg 2009;33:318–25
Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH, Kim KH, Ahn CS, Kim MH, Lee SK, Sung KB, Ko GY. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Surg 2010;17:476–489
Are C, Gonen M, D’Angelica M, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR. Differential diagnosis of proximal biliary obstruction. Surgery 2006;140:756-63
Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K, Matsumoto J, Kawasaki R. Outcome of surgical treatment of hilar cholangiocarcinoma: a special reference to postoperative morbidity and mortality. J Hepatobiliary Pancreat Surg 2009 [Epub ahead of print]
Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg 2004;240:95–101
Sano T, Shimada K, Sakamoto Y, Yamamoto J, Yamasaki S, Kosuge T. One hundred two consecutive hepatobiliary resections for perihilar cholangiocarcinoma with zero mortality. Ann Surg 2006;244:240–7.
Kanazawa H, Nagino M, Kamiya S, Komatsu S, Mayumi T, Takagi K, Asahara T, Nomoto K, Tanaka R, Nimura Y. Synbiotics reduce postoperative infectious complications: a randomized controlled trial in biliary cancer patients undergoing hepatectomy. Langenbecks Arch Surg 2005;390:104-13.
Sugawara G, Nagino M, Nishio H, Ebata T, Takagi K, Asahara T, Nomoto K, Nimura Y. Perioperative synbiotic treatment to prevent postoperative infectious complications in biliary cancer surgery: a randomized controlled trial. Ann Surg 2006;244:706-14.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13.
Kennedy TJ, Yopp A, Qin Y, Zhao B, Guo P, Liu F, et al. Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB (Oxford). 2009;11:445-51.
Regimbeau JM, Farges O, Pruvot FR. Chirurgie des cholangiocarcinomes intrahépatiques, hilaires et vésiculaires. Cancer du hile : drainage biliaire et embolisation portale avant hépatectomie (pp. 169-176). In Monographie de l’Association Française de Chirurgie. Springer-Verlag Paris 2009.
Montero JL, Pozo JC, Barrera P, Fraga E, Costan G, Dominguez JL, et al. Treatment of refractory cholestatic pruritus with molecular adsorbent recirculating system (MARS). Transplant Proc 2006;38:2511-3
Francoz C, Sobesky R, Paugam-Burtz C, Sommacale D, Dondero F, Belghiti J, et al. Albumin dialysis using MARS: an effective treatment for patients with diffuse cholangitis and refractory pruritus while awaiting for retransplantation. Liver Transpl 2007;13:S163 [abstract]
Sturm E, Franssen CF, Gouw A, Staels B, Boverhof R, De Knegt RJ, Stellaard F, Bijleveld CM, Kuipers F. Extracorporal albumin dialysis (MARS) improves cholestasis and normalizes low apo A-I levels in a patient with benign recurrent intrahepatic cholestasis (BRIC). Liver. 2002;22 Suppl 2:72-5
Tsao JI, Nimura Y, Kamiya J, Hayakawa N, Kondo S, Nagino M, et al. Management of hilar cholangiocarcinoma: comparison of an American and a Japanese experience. Ann Surg 2000;232:166–74.
Jarnagin WR, Bowne W, Klimstra DS, Ben-Porat L, Roggin K, Cymes K, et al. Papillary phenotype confers improved survival after resection of hilar cholangiocarcinoma. Ann Surg 2005;241:703–12.
Baton O, Azoulay D, Adam DV, Castaing D. Major hepatectomy for hilar cholangiocarcinoma type 3 and 4: prognostic factors and longterm outcomes. J Am Coll Surg 2007;204:250-60.
Maeno H, Ono T, Yamanoi A, Nagasue N. Our experiences in surgical treatment for hilar cholangiocarcinoma. Hepatogastroenterology. 2007;54:669-73.
Chen XP, Lau WY, Huang ZY, Zhang ZW, Chen YF, Zhang WG, Qiu FZ. Extent of liver resection for hilar cholangiocarcinoma. Br J Surg 2009;96:1167-75
Paik KY, Choi DW, Chung JC, Kang KT, Kim SB. Improved survival following right trisectionectomy with caudate lobectomy without operative mortality: surgical treatment for hilar cholangiocarcinoma. J Gastrointest Surg 2008;12:1268-74.
Igami T, Nishio H, Ebata T, Yokoyama Y, Sugawara G, Nimura Y, Nagino M. Surgical treatment of hilar cholangiocarcinoma in the “new era”: the Nagoya University experience. J Hepatobiliary Pancreat Surg 2009. [Epub ahead of print]
Shimizu H, Kimura F, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, Furukawa K, Miyazaki M. Aggressive surgical resection for hilar cholangiocarcinoma of the left-side predominance: radicality and safety of left-sided hepatectomy. Ann Surg 2010;251:281-6.
Acknowledgments
The authors wish to thank the following surgeons, who included patients in the study: J Hardwigsen (Hôpital de la Conception, Marseille), P Pessaux (Hôpital Hautepierre, Strasbourg), J Belghiti (Hôpital Beaujon, Clichy), C Ducerf (Hôpital de la Croix Rousse, Lyon), E Boleslawski (Hôpital Huriez, Lille), D Cherqui (Hôpital Henri Mondor, Créteil), A Laurent (Hôpital Henri Mondor, Créteil), G Mantion (Centre Hospitalier Universitaire, Besançon), J Lubrano (Centre Hospitalier Universitaire, Besançon), B Suc (Centre Hospitalier Universitaire, Toulouse), G Fourtanier (Centre Hospitalier Universitaire, Toulouse), G Nuzzo (Université Catholique de Rome), D Bertrand (Hôpital de Jolimont-Lobbes, Belgique), D Dili (Hôpital de Jolimont-Lobbes, Belgique), N Dehni (Centre Hospitalier Universitaire, Brest), O Soubrane (Hôpital Cochin, Paris), O Scatton (Hôpital Cochin, Paris), C Letoublon (Centre Hospitalier Universitaire, Grenoble), D Badic (Centre Hospitalier Universitaire, Grenoble), and M Scotte (Hôpital Charles Nicolle, Rouen).
Conflicts of interest
None of the authors have any financial or personal relationships with other people or organizations that could inappropriately influence (bias) this work.
Responsibility
This multicenter study is an original work not submitted to any other journal. The corresponding author had full access to all study data and has final responsibility for the decision to submit this manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors’ contributions
All authors are justifiably credited with authorship:
For Study conception and design: JM. Regimbeau, O. Farges, and FR. Pruvot;
For Acquisition of data: all authors;
For Analysis and interpretation of data: D. Fuks, JM. Regimbeau, O. Farges;
For Drafting of manuscript: JM. Regimbeau, D. Fuks;
For Critical revision of manuscript: JM. Regimbeau, O. Farges, D. Fuks;
And for Supervision: JM. Regimbeau, O. Farges.
All authors agree with the submission and have given their final approval.
Rights and permissions
About this article
Cite this article
Regimbeau, J.M., Fuks, D., Le Treut, YP. et al. Surgery for Hilar Cholangiocarcinoma: A Multi-institutional Update on Practice and Outcome by the AFC-HC Study Group. J Gastrointest Surg 15, 480–488 (2011). https://doi.org/10.1007/s11605-011-1414-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1414-0