ABSTRACT
BACKGROUND
Racial disparities in hypertension control contribute to higher rates of cardiovascular mortality among blacks. Patient-physician communication quality is associated with better health outcomes, including blood pressure (BP) control. Both race/ethnicity and BP control may adversely affect communication.
OBJECTIVE
To determine whether being black and having poor BP control interact to adversely affect patient-physician communication more than either condition alone, a situation referred to as “double jeopardy.”
DESIGN, SETTINGS, AND PATIENTS
Cross-sectional study of enrollment data from a randomized controlled trial of interventions to enhance patient adherence to therapy for hypertension. Participants included 226 hypertensive patients and 39 physicians from 15 primary care practices in Baltimore, MD.
MEASUREMENTS
Communication behaviors and visit length from coding of audiotapes.
RESULTS
After controlling for patient and physician characteristics, blacks with uncontrolled BP have shorter visits (B = −3.9 min, p < 0.01) with less biomedical (B = −24.0, p = 0.05), psychosocial (B = −19.4, p < 0.01), and rapport-building (B = −19.5, p = 0.01) statements than whites with controlled BP. Of all communication outcomes, blacks with uncontrolled BP are only in “double jeopardy” for a patient positive affect—coders give them lower ratings than all other patients. Blacks with controlled BP also experience shorter visits and less communication with physicians than whites with controlled BP. There are no significant communication differences between the visits of whites with uncontrolled versus controlled BP.
CONCLUSIONS
This study reveals that patient race is associated with the quality of patient-physician communication to a greater extent than BP control. Interventions that improve patient-physician communication should be tested as a strategy to reduce racial disparities in hypertension care and outcomes.

Similar content being viewed by others
References
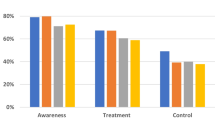
Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290(2):199–206.
Fields LE, Burt VL, Cutler JA, Hughes J, Roccella EJ, Sorlie P. The burden of adult hypertension in the United States 1999 to 2000: a rising tide. Hypertension. 2004;44(4):398–404.
Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339(27):1957–63.
Gu Q, Burt VL, Paulose-Ram R, Yoon S, Gillum RF. High blood pressure and cardiovascular disease mortality risk among US adults: the third National Health and Nutrition Examination Survey mortality follow-up study. Ann Epidemiol. 2008;18(4):302–9.
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Stamler J. End-stage renal disease in African-American and white men. 16-year MRFIT findings. JAMA. 1997;277(16):1293–8.
Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347(20):1585–92.
National Center for Health Statistics. Health, United States. 2003. Available at http://www.cdc.gov/nchs/data/hus/hus03.pdf
Lillie-Blanton M, Maddox TM, Rushing O, Mensah GA. Disparities in cardiac care: rising to the challenge of Healthy People 2010. J Am Coll Cardiol. 2004;44(3):503–8.
Hicks LS, Fairchild DG, Horng MS, Orav EJ, Bates DW, Ayanian JZ. Determinants of JNC VI guideline adherence, intensity of drug therapy, and blood pressure control by race and ethnicity. Hypertension. 2004;44(4):429–34.
Bosworth HB, Dudley T, Olsen MK, et al. Racial differences in blood pressure control: potential explanatory factors. Am J Med. 2006;119(1):70.e9–70.15.
Hyre AD, Krousel-Wood MA, Muntner P, Kawasaki L, DeSalvo KB. Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting. J Clin Hypertens (Greenwich). 2007;9(3):179–86.
Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. N Engl J Med. 1992;327(11):776–81.
Moy E, Bartman BA, Weir MR. Access to hypertensive care. Effects of income, insurance, and source of care. Arch Intern Med. 1995;155(14):1497–502.
Wyatt SB, Akylbekova EL, Wofford MR, et al. Prevalence, awareness, treatment and control of hypertension in the Jackson Heart Study. Hypertension. 2008;51(3):650–6.
Alexander M, Gordon NP, Davis CC, Chen RS. Patient knowledge and awareness of hypertension is suboptimal: results from a large health maintenance organization. J Clin Hypertens (Greenwich). 2003;5(4):254–60.
Ogedegbe G, Harrison M, Robbins L, Mancuso CA, Allegrante JP. Barriers and facilitators of medication adherence in hypertensive African Americans: a qualitative study. Ethn Dis. 2004;14(1):3–12.
Lukoschek P. African Americans’ beliefs and attitudes regarding hypertension and its treatment: a qualitative study. J Health Care Poor Underserved. 2003;14(4):566–87.
He J, Muntner P, Chen J, Roccella EJ, Streiffer RH, Whelton PK. Factors associated with hypertension control in the general population of the United States. Arch Intern Med. 2002;162(9):1051–8.
Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–27.
Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–33.
Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press, Washington, DC; 2001.
Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804.
Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323(7318):908–11.
Wilson IB, Kaplan S. Physician-patient communication in HIV disease: the importance of patient, physician, and visit characteristics. J Acquir Immune Defic Syndr. 2000;25(5):417–25.
Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17(4):243–52.
Diette GB, Rand C. The contributing role of health-care communication to health disparities for minority patients with asthma. Chest. 2007;132(5 Suppl):802S–9S.
Ghods BK, Roter DL, Ford DE, Larson S, Arbelaez JJ, Cooper LA. Patient-physician communication in the primary care visits of African Americans and whites with depression. J Gen Intern Med. 2008.
Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94(12):2084–90.
Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907–15.
Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns. 2006;62(3):355–60.
Roter DL, Stewart M, Putnam SM, Lipkin M Jr, Stiles W, Inui TS. Communication patterns of primary care physicians. JAMA. 1997;277(4):350–6.
Hooper EM, Comstock LM, Goodwin JM, Goodwin JS. Patient characteristics that influence physician behavior. Med Care. 1982;20(6):630–8.
Kressin NR, Wang F, Long J, et al. Hypertensive patients’ race, health beliefs, process of care, and medication adherence. J Gen Intern Med. 2007;22(6):768–74.
Fung CH, Setodji CM, Kung FY, et al. The relationship between multimorbidity and patients’ ratings of communication. J Gen Intern Med. 2008;23(6):788–93.
Min LC, Wenger NS, Fung C, et al. Multimorbidity is associated with better quality of care among vulnerable elders. Med Care. 2007;45(6):480–8.
Higashi T, Wenger NS, Adams JL, et al. Relationship between number of medical conditions and quality of care. N Engl J Med. 2007;356(24):2496–504.
Chang JT, Hays RD, Shekelle PG, et al. Patients’ global ratings of their health care are not associated with the technical quality of their care. Ann Intern Med. 2006;144(9):665–72.
Wolff JL, Roter DL. Hidden in plain sight: medical visit companions as a resource for vulnerable older adults. Arch Intern Med. 2008;168(13):1409–15.
Cooper LA, Roter DL, Bone LR, et al. A randomized controlled trial of interventions to enhance patient-physician partnership, patient adherence and high blood pressure control among ethnic minorities and poor persons: study protocol NCT00123045. Implement Sci. 2009;4:7.
Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391–5.
Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs. 2000;15(3):90–6.
Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46(4):243–51.
www.rias.org. Last updated 2/4/09. Accessed Septemerber 17, 2008.
Roter DL, Larson S. The relationship between residents’ and attending physicians’ communication during primary care visits: an illustrative use of the Roter Interaction Analysis System. Health Commun. 2001;13(1):33–48.
Liang KY, Zeger SL. Regression analysis for correlated data. Annu Rev Public Health. 1993;14:43–68.
van Wieringen JC, Harmsen JA, Bruijnzeels MA. Intercultural communication in general practice. Eur J Public Health. 2002;12(1):63–8.
Hall JA, Roter DL, Rand CS. Communication of affect between patient and physician. J Health Soc Behav. 1981;22(1):18–30.
Oliver MN, Goodwin MA, Gotler RS, Gregory PM, Stange KC. Time use in clinical encounters: are African-American patients treated differently? J Natl Med Assoc. 2001;93(10):380–5.
Wiggers JH, Sanson-Fisher R. Duration of general practice consultations: association with patient occupational and educational status. Soc Sci Med. 1997;44(7):925–34.
Gross DA, Zyzanski SJ, Borawski EA, Cebul RD, Stange KC. Patient satisfaction with time spent with their physician. J Fam Pract. 1998;47(2):133–7.
Wilson IB, Kaplan S. Physician-patient communication in HIV disease: the importance of patient, physician, and visit characteristics. J Acquir Immune Defic Syndr. 2000;25(5):417–25.
Howie JG, Porter AM, Heaney DJ, Hopton JL. Long to short consultation ratio: a proxy measure of quality of care for general practice. Br J Gen Pract. 1991;41(343):48–54.
Morrell DC, Evans ME, Morris RW, Roland MO. The “five minute” consultation: effect of time constraint on clinical content and patient satisfaction. Br Med J (Clin Res Ed). 1986;292(6524):870–3.
Schlomann P, Schmitke J. Lay beliefs about hypertension: an interpretive synthesis of the qualitative research. J Am Acad Nurse Pract. 2007;19(7):358–67.
Boutin-Foster C, Ogedegbe G, Ravenell JE, Robbins L, Charlson ME. Ascribing meaning to hypertension: a qualitative study among African Americans with uncontrolled hypertension. Ethn Dis. 2007;17(1):29–34.
Sharkness CM, Snow DA. The patient’s view of hypertension and compliance. Am J Prev Med. 1992;8(3):141–6.
Meyer D, Leventhal H, Gutmann M. Common-sense models of illness: the example of hypertension. Health Psychol. 1985;4(2):115–35.
Hall JA, Roter DL, Milburn MA, Daltroy LH. Patients’ health as a predictor of physician and patient behavior in medical visits. A synthesis of four studies. Med Care. 1996;34(12):1205–18.
Walsh JM, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44(7):646–57.
Cooper LA. A 41-year-old African American man with poorly controlled hypertension: review of patient and physician factors related to hypertension treatment adherence. JAMA. 2009;301(12):1260–72.
Brownstein JN, Chowdhury FM, Norris SL, et al. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med. 2007;32(5):435–47.
Ornstein S, Jenkins RG, Nietert PJ, et al. A multimethod quality improvement intervention to improve preventive cardiovascular care: a cluster randomized trial. Ann Intern Med. 2004;141(7):523–32.
Simon SR, Majumdar SR, Prosser LA, et al. Group versus individual academic detailing to improve the use of antihypertensive medications in primary care: a cluster-randomized controlled trial. Am J Med. 2005;118(5):521–8.
Goldstein MK, Lavori P, Coleman R, Advani A, Hoffman BB. Improving adherence to guidelines for hypertension drug prescribing: cluster-randomized controlled trial of general versus patient-specific recommendations. Am J Manag Care. 2005;11(11):677–85.
Fretheim A, Havelsrud K, Oxman AD. Rational Prescribing in Primary care (RaPP): process evaluation of an intervention to improve prescribing of antihypertensive and cholesterol-lowering drugs. Implement Sci. 2006;1:19.
Hicks LS, Sequist TD, Ayanian JZ, et al. Impact of computerized decision support on blood pressure management and control: a randomized controlled trial. J Gen Intern Med. 2008;23(4):429–41.
Bonds DE, Hogan PE, Bertoni AG, et al. A multifaceted intervention to improve blood pressure control: The Guideline Adherence for Heart Health (GLAD) study. Am Heart J. 2009;157(2):278–84.
Acknowledgements
This paper was presented, in part, at the 30th Annual Meeting of the Society of General Internal Medicine, April 27, 2007, Toronto, Ontario. This work was supported by grants from the National Heart, Lung, and Blood Institute (R01HL069403, K24HL083113, and T32HL07180). The authors would like to thank David M. Levine, MD, MPH, ScD, Michael S. Barr, MD, MBA, and Lee R. Bone, MPH, RN for their contributions as co-investigators in the Patient-Physician Partnership to Improve High Blood Pressure Adherence Study and Drs. Levine and Barr for reviewing earlier versions of this manuscript. Dr. Cene also received salary support from the National Center for Research Resources (KL2RR025746). The content of the manuscript is solely the responsibility of the authors and does not necessarily reflect the views of the National Center for Research Resources or the National Heart, Lung, and Blood Institute.
Conflict of Interest
Dr. Debra Roter is the author of the Roter Interaction Analysis System (RIAS) and holds the copyright for the system. Johns Hopkins University also has rights to enhancements of the system. Neither Debra Roter nor Johns Hopkins collect royalties for use of the system in research conducted at the Johns Hopkins University and Medical Institutions. Debra Roter is owner of RIASWorks LLC, a company that provides RIAS coding services to clients outside of the Johns Hopkins University System. It may be possible that the company will benefit indirectly from dissemination of the current research. Dr. Lisa Cooper received a grant, and Ms. Kathryn Carson received salary support, from AMGEN, a human therapeutics company in the biotechnology industry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cené, C.W., Roter, D., Carson, K.A. et al. The Effect of Patient Race and Blood Pressure Control on Patient-Physician Communication. J GEN INTERN MED 24, 1057–1064 (2009). https://doi.org/10.1007/s11606-009-1051-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1051-4