Abstract
Background
The occurrence and timing of prostate biopsy following an elevated prostate-specific antigen (PSA) test varied considerably in randomized screening trials.
Objective
Examine practice patterns in routine clinical care in response to an elevated PSA test (≥4 ng/μl) and determine whether time to biopsy was associated with cancer stage at diagnosis.
Design
Retrospective cohort study.
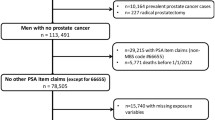
Participants
All veterans (n = 13,591) in the Pacific Northwest VA Network with a PSA ≥4 ng/μl between 1998 and 2006 and no previous elevated PSA tests or prostate biopsy.
Main Measures
We assessed follow-up care including additional PSA testing, urology consults, and biopsies. We compared stage at diagnosis for men who were biopsied within 24 months vs. those men biopsied and diagnosed >24 months after the elevated PSA test.
Key Results
Two-thirds of patients received follow-up evaluation within 24 months of the elevated PSA test: 32.8% of men underwent a biopsy, 15.5% attended a urology visit but were not biopsied, and 18.8% had a subsequent normal PSA test. Younger age, higher PSA levels, more prior PSA tests, no co-payment requirements, existing urologic conditions, low body mass index, and low comorbidity scores were associated with more complete follow-up. Among men who underwent radical prostatectomy, a delayed diagnosis was not significantly associated with having a pathologically advanced-stage cancer (T3/T4), although we found an increased likelihood of presenting with stage T2C relative to stage T2A or T2B cancer.
Conclusions
Follow-up after an elevated PSA test is highly variable with more than a third of men receiving care that could be considered incomplete. A delayed diagnosis was not associated with poorer prognosis.
Similar content being viewed by others
References
Wolf AM, Wender RC, Etzioni RB, et al. American Cancer Society guideline for the early detection of prostate cancer: update 2010. CA Cancer J Clin. 2010;60:70–98.
Andriole GL, Crawford ED, Grubb RL 3rd, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009;360:1310–1319.
Schroder FH, Hugosson J, Roobol MJ, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360:1320–1328.
Pinsky PF, Andriole GL, Kramer BS, et al. Prostate biopsy following a positive screen in the prostate, lung, colorectal and ovarian cancer screening trial. J Urol. 2005;173:746–750. discussion 750-741.
Grubb RL 3rd, Pinsky PF, Greenlee RT, et al. Prostate cancer screening in the Prostate, Lung, Colorectal and Ovarian cancer screening trial: update on findings from the initial four rounds of screening in a randomized trial. BJU Int. 2008;102:1524–1530.
de Koning HJ, Auvinen A, Berenguer Sanchez A, et al. Large-scale randomized prostate cancer screening trials: program performances in the European Randomized Screening for Prostate Cancer trial and the Prostate, Lung, Colorectal and Ovary cancer trial. Int J Cancer. 2002;97:237–244.
Hoffman RM, Blume P, Gilliland F. Prostate-specific antigen testing practices and outcomes. J Gen Intern Med. 1998;13:106–110.
Maynard C, Chapko MK. Data resources in the Department of Veterans Affairs. Diabetes Care. 2004;27(Suppl 2):B22–26.
Haggstrom, DA. Developing Validated Algorithms to Identify Cancer in Existing VA Databases. Health Services Research & Development Service (HSR&D) Studies 2009; www.hsrd.research.va.gov/research/abstracts.cfm?Project_ID = 2141698776 Last accessed July 2, 2010.
Nattinger AB, Laud PW, Bajorunaite R, et al. An algorithm for the use of Medicare claims data to identify women with incident breast cancer. Health Serv Res. 2004;39:1733–1749.
Kuo YF, Goodwin JS, Shahinian VB. Gonadotropin-releasing hormone agonist use in men without a cancer registry diagnosis of prostate cancer. BMC Health Serv Res. 2008;8:146.
Walter LC, Bertenthal D, Lindquist K, et al. PSA screening among elderly men with limited life expectancies. JAMA. 2006;296:2336–2342.
Wei JT, Calhoun EA, Jacobsen SJ. Benign Prostatic Hyperplasia. In: Litwin MS, Saigal CS, eds. Urologic Diseases in America. Washington DC: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2007:43–69.
McNaughton-Collins M, Joyce GF, Wise M, et al. Prostatitis. In: Litwin MS, Saigal CS, eds. Urologic Diseases in America. Washington DC: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2007:9–41.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139.
Morrill R, Cromartie J, Hart G. Metropolitan, urban, and rural commuting areas: toward a better depiction of the United States settlement system. Urban Geography. 1999;20:727–748.
Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. Am J Public Health. 2005;95:1149–1155.
Hosmer DW, Lemeshow S. Applied Logistic Regression. Chichester: Wiley; 1989.
Long JS, Freese J. Regression models for categorical dependent variables using Stata 2nd ed. College Station: Stata Press; 2006.
Long JS, Freese J. Spost9: Post-estimation interpretation of regression models including multinomial regression models. UCLA: Academic Technology Services, Statistical Consulting Group. Los Angeles 2009.
Carroll P, Albertson PC, Green K, et al. Prostate-Specific Antigen Best Practice Statement: 2009 Update. Available at http://www.auanet.org/content/guidelines-and-quality-care/clinical-guidelines/main-reports/psa09.pdf Last accessed July 2, 2010.
Stamey TA, Johnstone IM, McNeal JE, et al. Preoperative serum prostate specific antigen levels between 2 and 22 ng./ml. correlate poorly with post-radical prostatectomy cancer morphology: prostate specific antigen cure rates appear constant between 2 and 9 ng./ml. J Urol. 2002;167:103–111.
Stephenson AJ, Scardino PT, Eastham JA, et al. Postoperative nomogram predicting the 10-year probability of prostate cancer recurrence after radical prostatectomy. J Clin Oncol. 2005;23:7005–7012.
Ankerst DP, Miyamoto R, Nair PV, et al. Yearly prostate specific antigen and digital rectal examination fluctuations in a screened population. J Urol. 2009;181:2071–2075. discussion 2076.
McNaughton-Collins M, Fowler FJ Jr, Caubet JF, et al. Psychological effects of a suspicious prostate cancer screening test followed by a benign biopsy result. Am J Med. 2004;117:719–725.
Schwartz LM, Woloshin S, Fowler FJ Jr, et al. Enthusiasm for cancer screening in the United States. JAMA. 2004;291:71–78.
Volk RJ, Hawley ST, Kneuper S, et al. Trials of decision aids for prostate cancer screening: A systematic review. Am J Prev Med. 2007;33:428–434.
Sheridan SL, Harris RP, Woolf SH. Shared decision making about screening and chemoprevention. a suggested approach from the US Preventive Services Task Force. Am J Prev Med. 2004;26:56–66.
Feldman-Stewart D, Brundage MD, McConnell BA, et al. Practical issues in assisting shared decision-making. Health Expect. 2000;3:46–54.
Holmes-Rovner M, Stableford S, Fagerlin A, et al. Evidence-based patient choice: a prostate cancer decision aid in plain language. BMC Med Inform Decis Mak. 2005;5:16.
Hoffman RM, Couper MP, Zikmund-Fisher BJ, et al. Prostate cancer screening decisions: results from the National Survey of Medical Decisions (DECISIONS study). Arch Intern Med. 2009;169:1611–1618.
Federman DG, Goyal S, Kamina A, et al. Informed consent for PSA screening: does it happen? Eff Clin Pract. 1999;2:152–157.
Nelson KM, Starkebaum GA, Reiber GE. Veterans using and uninsured veterans not using Veterans Affairs (VA) health care. Public Health Rep. 2007;122:93–100.
Ross LE, Taylor YJ, Richardson LC, et al. Patterns in prostate-specific antigen test use and digital rectal examinations in the Behavioral Risk Factor Surveillance System, 2002-2006. J Natl Med Assoc. 2009;101:316–324.
Nepple KG, Joudi FN, Hillis SL, et al. Prevalence of delayed clinician response to elevated prostate-specific antigen values. Mayo Clin Proc. 2008;83:439–448.
Collins MM, Fowler FJ Jr, Roberts RG, et al. Medical malpractice implications of PSA testing for early detection of prostate cancer. J Law Med Ethics. 1997;25:234–242. 230.
Merenstein D. A piece of my mind. Winners and losers. JAMA. 2004;291:15–16.
Overmyer M. PSA in older men: New data, lawsuits raise the stakes. Urology Times. March 1, 2007.
Krist AH, Woolf SH, Johnson RE. How physicians approach prostate cancer screening before and after losing a lawsuit. Ann Fam Med. 2007;5:120–125.
Acknowledgements
This work was supported by the VA. The VA Office of Research and Development Health Services R&D, Department of Veterans Affairs, funded this study through a Short-term Health Services Project grant: SHP-08-165. The authors are grateful to Adam Batten for data processing, and to Bruce Wynar and Carol Simons for chart review and data abstraction. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the VA. The VA Office of Research and Development Health Services R&D, Department of Veterans Affairs, Short-term Health Services Project, SHP-08-165, funded this study. Portions of the data presented here were presented at the VA Health Services R&D National Meeting in February 2009 and at the Annual Meeting of the American Urological Association in April 2009.
Rights and permissions
About this article
Cite this article
Zeliadt, S.B., Hoffman, R.M., Etzioni, R. et al. What Happens After an Elevated PSA Test: The Experience of 13,591 Veterans. J GEN INTERN MED 25, 1205–1210 (2010). https://doi.org/10.1007/s11606-010-1468-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1468-9