Abstract
Purpose
The present work investigated the relationship between patient activation, treatment decision-making, and adherence to the prescribed treatment regimen. Given the role of informal caregivers in patient-reported outcomes, it was additionally assessed whether caregiver involvement acted as a moderator of this relationship.
Methods
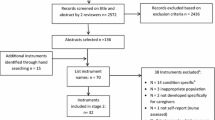
Survey data collected from 504 cancer survivors were utilized. Structural equation modeling (SEM) controlling for covariates was used to examine the relationship between patient activation measure (PAM), caregiver involvement, and the identified outcomes. Moderator analysis was conducted using multiple group SEM.
Results
Patient activation was significantly associated with treatment planning being reflective of survivors’ goals and values (p < 0.001); adherence to treatment (p = 0.011); and satisfaction (p < 0.001). Caregiver’s involvement significantly moderated the association between activation and adherence to treatment.
Conclusions
Patient activation was positively associated with all three selected outcomes. However, for cancer survivors reporting low rates of caregiver’s involvement, patient activation was not associated with treatment adherence. Research is needed to test and deliver self-management interventions inclusive of informal caregivers.
Implications for Cancer Survivors
Findings supported the need not only to monitor and sustain patient activation across the cancer continuum, but also to assume a dyadic perspective when designing self-management interventions in cancer survivorship.


Similar content being viewed by others
Data availability
Data are available upon request.
Code availability
Not applicable.
References
IOM, Delivering high-quality cancer care: charting a new course for a system in crisis, ed. L.A. Levit, et al. 2013, Washington, DC: The National Academies Press. 412.
Jaffee EM, et al. Future cancer research priorities in the USA: a Lancet Oncology Commission. Lancet Oncol. 2017;18(11):e653–706.
Covvey JR, et al. Barriers and facilitators to shared decision-making in oncology: a systematic review of the literature. Support Care Cancer. 2019;27(5):1613–37.
Hibbard, et al. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005–26.
Hibbard JH, et al. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918–30.
Greene J, et al. When patient activation levels change, health outcomes and costs change, too. Health Aff (Millwood). 2015;34(3):431–7.
Shively MJ, et al. Effect of patient activation on self-management in patients with heart failure. J Cardiovasc Nurs. 2013;28(1):20–34.
Rogvi S, et al. Patient factors and glycaemic control–associations and explanatory power. Diabet Med. 2012;29(10):e382–9.
Mosen DM, et al. Is patient activation associated with outcomes of care for adults with chronic conditions? J Ambul Care Manage. 2007;30(1):21–9.
Remmers C, et al. Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? J Ambul Care Manage. 2009;32(4):320–7.
Kinney RL, et al. The association between patient activation and medication adherence, hospitalization, and emergency room utilization in patients with chronic illnesses: a systematic review. Patient Educ Couns. 2015;98(5):545–52.
Hibbard JH, Mahoney E, Sonet E. Does patient activation level affect the cancer patient journey? Patient Educ Couns. 2017;100(7):1276–9.
Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;32(2):207–14.
Fowles JB, et al. Measuring self-management of patients’ and employees’ health: further validation of the patient activation measure (PAM) based on its relation to employee characteristics. Patient Educ Couns. 2009;77(1):116–22.
Hibbard JH. Using systematic measurement to target consumer activation strategies. Med Care Res Rev. 2009;66(1):9s–27s.
Hibbard JH, et al. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42(4):1443–63.
Hibbard JH, Cunningham PJ. How engaged are consumers in their health and health care, and why does it matter? Res Brief. 2008;8:1–9.
TABRIZI, J.S., A.J. WILSON, and P.K. O ROURKE, Customer quality and type 2 diabetes from the patients’ perspective: a cross-sectional study. JOURNAL OF RESEARCH IN HEALTH SCIENCES (JRHS), 2010. 10 (2).
Krouse RS, et al. A chronic care ostomy self-management program for cancer survivors. Psychooncology. 2016;25(5):574–81.
O’Malley D, et al. Determinants of patient activation in a community sample of breast and prostate cancer survivors. Psychooncology. 2018;27(1):132–40.
Mazanec SR, et al. Activation for health management in colorectal cancer survivors and their family caregivers. West J Nurs Res. 2016;38(3):325–44.
Miller KD, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–85.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Kayser K, Watson LE, Andrade JT. Cancer as a “we-disease”: examining the process of coping from a relational perspective. Fam Syst Health. 2007;25(4):404–18.
Manne S, Badr H. Intimacy and relationship processes in couples’ psychosocial adaptation to cancer. Cancer. 2008;112(S11):2541–55.
Lund L, et al. Cancer caregiving tasks and consequences and their associations with caregiver status and the caregiver’s relationship to the patient: a survey. BMC Cancer. 2014;14:541.
Kent EE, et al. Caring for caregivers and patients: Research and clinical priorities for informal cancer caregiving. Cancer. 2016;122(13):1987–95.
Epplein M, et al. Quality of life after breast cancer diagnosis and survival. J Clin Oncol. 2011;29(4):406–12.
Poghosyan H, et al. Health-related quality of life after surgical treatment in patients with non-small cell lung cancer: a systematic review. Lung Cancer. 2013;81(1):11–26.
Drake, K., Quality of life for cancer patients: from diagnosis to treatment and beyond. Nurs Manage, 2012.
Duijts SF, et al. Physical and psychosocial problems in cancer survivors beyond return to work: a systematic review. Psychooncology. 2014;23(5):481–92.
Deshields TL, et al. Documenting the symptom experience of cancer patients. J Support Oncol. 2011;9(6):216–23.
Kent EE, et al. The importance of symptom surveillance during follow-up care of leukemia, bladder, and colorectal cancer survivors. Support Care Cancer. 2014;22(1):163–72.
Kim Y, et al. Quality of life of family caregivers 8 years after a relative’s cancer diagnosis: follow-up of the National Quality of Life Survey for Caregivers. Psychooncology. 2016;25(3):266–74.
Meeker MA, Finnell D, Othman AK. Family caregivers and cancer pain management: a review. J Fam Nurs. 2011;17(1):29–60.
McCorkle R, et al. Self-management: Enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin. 2011;61(1):50–62.
Litzelman K, Yabroff KR. How are spousal depressed mood, distress, and quality of life associated with risk of depressed mood in cancer survivors? Longitudinal findings from a national sample. Cancer Epidemiol Biomarkers Prev. 2015;24(6):969–77.
Kim Y, et al. Cancer caregiving predicts physical impairments: roles of earlier caregiving stress and being a spousal caregiver. Cancer. 2015;121(2):302–10.
Shaffer KM, Kim Y, Carver CS. Physical and mental health trajectories of cancer patients and caregivers across the year post-diagnosis: a dyadic investigation. Psychol Health. 2016;31(6):655–74.
Große J, Treml J, Kersting A. Impact of caregiver burden on mental health in bereaved caregivers of cancer patients: a systematic review. Psychooncology. 2018;27(3):757–67.
Bradley CJ. Economic burden associated with cancer caregiving. Semin Oncol Nurs. 2019;35(4):333–6.
Girgis A, et al. Physical, psychosocial, relationship, and economic burden of caring for people with cancer: a review. J Oncol Pract. 2013;9(4):197–202.
Paek MS, et al. Contextual and stress process factors associated with head and neck cancer caregivers’ physical and psychological well-being. Eur J Cancer Care. 2018;27(2):e12833–e12833.
Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psychooncology. 2010;19(10):1013–25.
Mollica MA, et al. The role of medical/nursing skills training in caregiver confidence and burden: A CanCORS study. Cancer. 2017;123(22):4481–7.
van Ryn M, et al. Objective burden, resources, and other stressors among informal cancer caregivers: a hidden quality issue? Psychooncology. 2011;20(1):44–52.
Streck BP, et al. Interdependence of physical and psychological morbidity among patients with cancer and family caregivers: review of the literature. Psychooncology. 2020;29(6):974–89.
Meyler D, Stimpson JP, Peek MK. Health concordance within couples: a systematic review. Soc Sci Med. 2007;64(11):2297–310.
Wittenberg E, Saada A, Prosser LA. How illness affects family members: a qualitative interview survey. Patient. 2013;6(4):257–68.
Kim Y, et al. Quality of life of couples dealing with cancer: dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Ann Behav Med. 2008;35(2):230–8.
Teixeira RJ, et al. The impact of coping strategies of cancer caregivers on psychophysiological outcomes: an integrative review. Psychol Res Behav Manag. 2018;11:207–15.
Dorros SM, et al. Interdependence in women with breast cancer and their partners: an interindividual model of distress. J Consult Clin Psychol. 2010;78(1):121–5.
Heffner KL, et al. Spousal support satisfaction as a modifier of physiological responses to marital conflict in younger and older couples. J Behav Med. 2004;27(3):233–54.
Kiecolt-Glaser JK, et al. Chronic stress alters the immune response to influenza virus vaccine in older adults. Proc Natl Acad Sci U S A. 1996;93(7):3043–7.
Vitaliano PP, et al. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med. 2002;64(3):418–35.
Li Q, Loke AY. A literature review on the mutual impact of the spousal caregiver–cancer patients dyads: ‘communication’, ‘reciprocal influence’, and ‘caregiver–patient congruence.’ Eur J Oncol Nurs. 2014;18(1):58–65.
Traa MJ, et al. Dyadic coping and relationship functioning in couples coping with cancer: a systematic review. Br J Health Psychol. 2015;20(1):85–114.
Vellone E, et al. Effects of self-care on quality of life in adults with heart failure and their spousal caregivers: testing dyadic dynamics using the actor–partner interdependence model. J Fam Nurs. 2014;20(1):120–41.
Van Houtven CH, Voils CI, Weinberger M. An organizing framework for informal caregiver interventions: detailing caregiving activities and caregiver and care recipient outcomes to optimize evaluation efforts. BMC Geriatr. 2011;11:77.
Mosher CE, et al. Development of a symptom management intervention: qualitative feedback from advanced lung cancer patients and their family caregivers. Cancer Nurs. 2017;40(1):66–75.
Oh YS. Communications with health professionals and psychological distress in family caregivers to cancer patients: a model based on stress-coping theory. Appl Nurs Res. 2017;33:5–9.
Mazer BL, et al. “Speaking-for” and “speaking-as”: pseudo-surrogacy in physician–patient–companion medical encounters about advanced cancer. Patient Educ Couns. 2014;96(1):36–42.
Laidsaar-Powell R, et al. The TRIO Framework: conceptual insights into family caregiver involvement and influence throughout cancer treatment decision-making. Patient Educ Couns. 2017;100(11):2035–46.
Laidsaar-Powell R, et al. Family involvement in cancer treatment decision-making: A qualitative study of patient, family, and clinician attitudes and experiences. Patient Educ Couns. 2016;99(7):1146–55.
Eggly S, et al. Information seeking during “bad news” oncology interactions: question asking by patients and their companions. Soc Sci Med. 2006;63(11):2974–85.
Street RL, Gordon HS. Companion participation in cancer consultations. Psychooncology. 2008;17(3):244–51.
Laidsaar-Powell R, et al. Attitudes and experiences of family involvement in cancer consultations: a qualitative exploration of patient and family member perspectives. Support Care Cancer. 2016;24(10):4131–40.
Wallner LP, et al. Decision-support networks of women newly diagnosed with breast cancer. Cancer. 2017;123(20):3895–903.
Dionne-Odom JN, et al. How family caregivers of persons with advanced cancer assist with upstream healthcare decision-making: a qualitative study. PLOS ONE. 2019;14(3):e0212967.
GILBAR R, GILBAR O. The medical decision-making process and the family: the case of breast cancer patients and their husbands. Bioethics. 2009;23(3):183–92.
Gonçalves F, et al. Breaking bad news: experiences and preferences of advanced cancer patients at a Portuguese oncology centre. Palliat Med. 2005;19(7):526–31.
Pardon K, Deschepper R, Stichele RV, Bernheim JL, Mortier F, Bossuyt N, Schallier D, Germonpré P, Galdermans D, Van Kerckhoven W, Deliens L; EOLIC-Consortium. Preferences of patients with advanced lung cancer regarding the involvement of family and others in medical decision-making. J Palliat Med. 2010;13(10):1199–203. https://doi.org/10.1089/jpm.2010.0100.
Schäfer C, et al. Medical decision-making of the patient in the context of the family: results of a survey. Support Care Cancer. 2006;14(9):952–9.
Shin DW, et al. Preferences for and experiences of family involvement in cancer treatment decision-making: patient-caregiver dyads study. Psychooncology. 2013;22(11):2624–31.
Wolff JL, Roter DL. Hidden in plain sight: medical visit companions as a resource for vulnerable older adults. Arch Intern Med. 2008;168(13):1409–15.
DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207–18.
Hilton BA. The 1993 Schering lecture: family decision-making processes about early stage breast cancer treatment. Can Oncol Nurs J. 2015;4(1):8.
Öhlén J, et al. The influence of significant others in complementary and alternative medicine decisions by cancer patients. Soc Sci Med. 2006;63(6):1625–36.
Hobbs GS, et al. The role of families in decisions regarding cancer treatments. Cancer. 2015;121(7):1079–87.
Krieger JL, et al. Caregiver perceptions of their influence on cancer treatment decision making: intersections of language, identity, and illness. J Lang Soc Psychol. 2015;34(6):640–56.
Miller LM, Sullivan DR, Lyons KS. Dyadic perceptions of the decision process in families living with lung cancer. Oncol Nurs Forum. 2017;44(1):108–15.
Shin DW, et al. Patient’s cognitive function and attitudes towards family involvement in cancer treatment decision making: a patient-family caregiver dyadic analysis. Cancer Res Treat. 2018;50(3):681–90.
Hallward L, et al. Prostate cancer survivors’ and caregivers’ experiences using behavior change techniques during a web-based self-management and physical activity program: a qualitative study. J Clin Med. 2020;9(10):3244.
Irani E, Niyomyart A, Hickman RL. Systematic review of technology-based interventions targeting chronically Ill adults and their caregivers. West J Nurs Res. 2020;42(11):974–92.
Pethybridge, R., L. Teleni, and R.J. Chan, How do family-caregivers of patients with advanced cancer provide symptom self-management support? A qualitative study. European Journal of Oncology Nursing, 2020. 48.
Høeg, B.L., et al., Is the health literacy of informal caregivers associated with the psychological outcomes of breast cancer survivors? Journal of Cancer Survivorship, 2020.
West, S.G., Taylor, A. B., Wu, W. , Model fit and model selection in structural equation modeling, in Handbook of structural equation modeling, R.H. Hoyle, Editor. 2014, Guildford Press. p. 209–231.
Muthén, L.K.a.M., B.O. , Mplus User’s Guide. Eighth Edition. 1998–2017, Los Angeles, CA: Muthén & Muthén.
Santana MJ, Feeny D. Framework to assess the effects of using patient-reported outcome measures in chronic care management. Qual Life Res. 2014;23(5):1505–13.
Santana MJ, et al. How to practice person-centred care: a conceptual framework. Health Expect. 2018;21(2):429–40.
Castro EM, et al. Patient empowerment, patient participation and patient-centeredness in hospital care: a concept analysis based on a literature review. Patient Educ Couns. 2016;99(12):1923–39.
Graffigna G, Barello S, Bonanomi A. The role of Patient Health Engagement Model (PHE-model) in affecting patient activation and medication adherence: a structural equation model. PLoS One. 2017;12(6):e0179865.
Leech M, et al. Empowering patients in decision-making in radiation oncology - can we do better? Mol Oncol. 2020;14(7):1442–60.
Gao J, et al. Understanding patient activation and adherence to nebuliser treatment in adults with cystic fibrosis: responses to the UK version of PAM-13 and a think aloud study. BMC Health Serv Res. 2019;19(1):420.
Mollborn S, Lawrence EM, Hummer RA. A gender framework for understanding health lifestyles. Soc Sci Med. 2020;265:113182.
Samulowitz A, et al. “Brave men” and “emotional women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manage. 2018;2018:6358624.
Mack, J.W., K.M. Fasciano, and S.D. Block, Adolescent and young adult cancer patients' experiences with treatment decision-making. Pediatrics, 2019. 143 (5).
Chen F, et al. Adherence to treatment guidelines as a major determinant of survival disparities between black and white patients with ovarian cancer. Gynecol Oncol. 2021;160(1):10–5.
DiMartino LD, Birken SA, Mayer DK. The relationship between cancer survivors’ socioeconomic status and reports of follow-up care discussions with providers. J Cancer Educ. 2017;32(4):749–55.
Regan, T.W., et al., Cross-sectional relationships between dyadic coping and anxiety, depression, and relationship satisfaction for patients with prostate cancer and their spouses. Patient Educ Couns, 2014. 96.
Rood JAJ, et al. Shared decision-making and providing information among newly diagnosed patients with hematological malignancies and their informal caregivers: Not “one-size-fits-all.” Psychooncology. 2017;26(12):2040–7.
Moon Z, et al. Barriers and facilitators of adjuvant hormone therapy adherence and persistence in women with breast cancer: a systematic review. Patient Prefer Adherence. 2017;11:305–22.
Entwistle VA, Watt IS. Patient involvement in treatment decision-making: the case for a broader conceptual framework. Patient Educ Couns. 2006;63(3):268–78.
Rapley T. Distributed decision making: the anatomy of decisions-in-action. Sociol Health Illn. 2008;30(3):429–44.
Epstein RM, Street RL. Shared mind: communication, decision making, and autonomy in serious illness. Ann Fam Med. 2011;9(5):454–61.
Elwyn G, et al. Collaborative deliberation: a model for patient care. Patient Educ Couns. 2014;97(2):158–64.
Juraskova I, et al. eTRIO trial: study protocol of a randomised controlled trial of online education modules to facilitate effective family caregiver involvement in oncology. BMJ Open. 2021;11(5):e043224.
Borson S, et al. Measuring caregiver activation to identify coaching and support needs: extending MYLOH to advanced chronic illness. PLoS ONE. 2018;13(10):e0205153–e0205153.
Barello S, et al. The Caregiving Health Engagement Scale (CHE-s): development and initial validation of a new questionnaire for measuring family caregiver engagement in healthcare. BMC Public Health. 2019;19(1):1562–1562.
Dingley CE, et al. Caregiver activation and home hospice nurse communication in advanced cancer care. Cancer Nurs. 2017;40(5):E38–50.
Rapelli G, et al. The combined effect of psychological and relational aspects on cardiac patient activation. J Clin Psychol Med Settings. 2020;27(4):783–94.
Allegrante JP, Wells MT, Peterson JC. Interventions to support behavioral self-management of chronic diseases. Annu Rev Public Health. 2019;40:127–46.
Hanlon P, et al. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res. 2017;19(5):e172–e172.
Kuijpers W, et al. A systematic review of web-based interventions for patient empowerment and physical activity in chronic diseases: relevance for cancer survivors. J Med Internet Res. 2013;15(2):e37.
Solomon M, Wagner SL, Goes J. Effects of a Web-based intervention for adults with chronic conditions on patient activation: online randomized controlled trial. J Med Internet Res. 2012;14(1):e32.
Taylor, S.J.C., et al., Health services and delivery research, in a rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions: PRISMS – Practical systematic Review of Self-Management Support for long-term conditions. 2014, NIHR Journals Library.
Rimmer, B., L. Sharp, and t. on behalf of Ways Ahead study, Implementation of self-management interventions in cancer survivors: why are we not there yet? Journal of Cancer Education, 2021.
Badr H, et al. Self-management intervention for head and neck cancer couples: results of a randomized pilot trial. Cancer. 2019;125(7):1176–84.
Badr H, et al. Development and usability testing of a web-based self-management intervention for oral cancer survivors and their family caregivers. Eur J Cancer Care (Engl). 2016;25(5):806–21.
Acknowledgements
This article is dedicated to the memory of Dr. Paul R. Swank, a generous mentor and colleague.
Author information
Authors and Affiliations
Contributions
CA, JD, and EMS contributed to study conceptualization and design; JD and EMS contributed to acquisition of data; CA, JD, ES, AZ, and EI contributed to analysis and interpretation of the data. CA, JD, ES, AZ, and EI contributed to drafting of manuscript and critical revisions.
Corresponding author
Ethics declarations
Ethics approval
STUDY00001137 University of Houston IRB.
Consent to participate
This is a secondary data analysis; participants in the original study completed informed consent documents.
Consent for publication
Not applicable.
Conflict of interest
Chiara Acquati, Ellen Miller-Sonet, Anao Zhang, and Elena Ionescu have no potential conflict of interest. Judith H. Hibbard is a consultant to and equity stakeholder in Insignia Health.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The present work was presented at the 2021 ASCO Annual Meeting, June 4-8, 2021 as part of the poster session: Symptoms and Survivorship.
Rights and permissions
About this article
Cite this article
Acquati, C., Hibbard, J.H., Miller-Sonet, E. et al. Patient activation and treatment decision-making in the context of cancer: examining the contribution of informal caregivers’ involvement. J Cancer Surviv 16, 929–939 (2022). https://doi.org/10.1007/s11764-021-01085-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-021-01085-9