Abstract
Purpose of Review
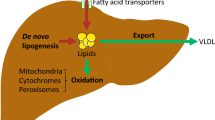
Drug-induced fatty liver disease (DIFLD) is one of the manifestations of drug-induced liver injury (DILI) based on histopathology findings of steatosis or steatohepatitis. DIFLD has high semblance to nonalcoholic fatty liver disease (NAFLD), where similar histopathological features are seen. As NAFLD is a commonly occurring disease, differentiating DIFLD from NAFLD requires a thorough history of medication use. Outcomes in DIFLD vary with the clinical presentation, with extremely high mortality in acute fatty liver presentations and indolent course in the rest. Pathophysiology in almost all cases of DIFLD encompasses one of the following: increased uptake or decreased output of triglycerides from hepatocytes or decreased metabolism of triglycerides (such as fatty acid oxidation) or electron transport chain. DIFLD may present as acute fatty liver or more commonly as indolent fatty liver disease. In this article, we outline pathophysiology, diagnosis, management, and common medications associated with DIFLD.
Recent Findings
Recent findings give insights into new technologies that may help us understand common pathways that are associated with drugs that cause and factors that modify susceptibility to DIFLD. Latest research has also allowed for identification of genetic polymorphisms associated with increased risk for DIFLD using genome-wide association studies (GWAS).
Summary
Drugs associated with DIFLD may have distinct clinical presentations, disease progression, and outcomes, timely identification of which is crucial to clinical management. We provide a succinct read for anyone interested in DIFLD phenotype of DILI, pathophysiology, clinical presentation, and management.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
On behalf of the Practice Parameters Committee of the American College of Gastroenterology, Chalasani NP, Hayashi PH, Bonkovsky HL, Navarro VJ, Lee WM, et al. ACG clinical guideline: the diagnosis and management of idiosyncratic drug-induced liver injury. Am J Gastroenterol. 2014;109:950–66.
Lammert C, Bjornsson E, Niklasson A, Chalasani N. Oral medications with significant hepatic metabolism at higher risk for hepatic adverse events. Hepatology. 2010;51:615–20.
Wang B, Avorn J, Kesselheim AS. Clinical and regulatory features of drugs not initially approved by the FDA. Clin Pharmacol Ther. 2013;94:670–7.
•• Clinical course and diagnosis of drug induced liver disease [Internet]. National Library Of Medicine and National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); Available from: https://livertox.nih.gov/ClinicalCourse.html. LiverTox is an authoritative online resource for drug-induced liver injury developed by Liver Diseases Branch, NIDDK in collaboration with Division of Specialized Information Services, National Library of Medicine.
•• Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–95. Landmark population-based study in the USA reporting prevalence of nonalcoholic fatty liver disease based in a multi-ethnic population based on magnetic resonance spectroscopy imaging.
Burt A, Mutton A, Day C. Diagnosis and interpretation of steatosis and steatohepatitis. Semin Diagn Pathol. 1998;15:246–58.
Kim S-H, Naisbitt DJ. Update on advances in research on idiosyncratic drug-induced liver injury. Allergy Asthma Immunol Res. 2016;8:3–11.
Chojkier M. Troglitazone and liver injury: in search of answers. Hepatology. 2005;41:237–46.
Chen M, Suzuki A, Borlak J, Andrade RJ, Lucena MI. Drug-induced liver injury: interactions between drug properties and host factors. J Hepatol. 2015;63:503–14.
• Lammert C, Einarsson S, Saha C, Niklasson A, Bjornsson E, Chalasani N. Relationship between daily dose of oral medications and idiosyncratic drug-induced liver injury: search for signals. Hepatology. 2008;47:2003–9. A study demonstrating the interesting relationship between dose of a drug and DILI.
Chen M, Borlak J, Tong W. High lipophilicity and high daily dose of oral medications are associated with significant risk for drug-induced liver injury. Hepatology. 2013;58:388–96.
Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the Liver 1978.
El-Ghaiesh S, Monshi MM, Whitaker P, Jenkins R, Meng X, Farrell J, et al. Characterization of the antigen specificity of T-cell clones from piperacillin-hypersensitive patients with cystic fibrosis. J Pharmacol Exp Ther. 2012;341:597–610.
Porebski G, Gschwend-Zawodniak A, Pichler WJ. In vitro diagnosis of T cell-mediated drug allergy: in vitro diagnosis of T cell-mediated drug allergy. Clin Exp Allergy. 2011;41:461–70.
Chessman D, Kostenko L, Lethborg T, Purcell AW, Williamson NA, Chen Z, et al. Human leukocyte antigen class I-restricted activation of CD8+ T cells provides the immunogenetic basis of a systemic drug hypersensitivity. Immunity. 2008;28:822–32.
Tang TT. Reye syndrome: a correlated Electron-microscopic, viral, and biochemical observation. JAMA. 1975;232:1339–46.
Young RSK. Reye’s syndrome associated with long-term aspirin therapy. JAMA J Am Med Assoc. 1984;251:754–6.
. McKenzie R, Fried MW, Sallie R, Conjeevaram H, Di Bisceglie AM, Park Y, et al. Hepatic failure and lactic acidosis due to fialuridine (FIAU), an investigational nucleoside analogue for chronic hepatitis B. N Engl J Med. 1995;333:1099–105. This study reports acute fatty liver associated with high mortality rate, associated with an investigational drug, fialuridine, during phase 2 study. Interestingly, this manifestation of hepatotoxicity was not seen during prior pilot studies where the drug was used at shorter intervals.
• Lewis JH, Ranard RC, Caruso A, Jackson LK, Mullick F, Ishak KG, et al. Amiodarone hepatotoxicity: prevalence and clinicopathologic correlations among 104 patients. Hepatology. 1989;9:679–85. A prospective study to characterize liver toxicity in 104 individuals who received amiodarone in the long term.
Poucell S, Ireton J, Valencia-Mayoral P, Downar E, Larratt L, Patterson J, et al. Amiodarone-associated phospholipidosis and fibrosis of the liver. Light, immunohistochemical, and electron microscopic studies. Gastroenterology. 1984;86:926–36.
Lüllmann H, Lüllmann-Rauch R, Wassermann O. Drug-induced phospholipidosis. Ger Med. 1973;3:128–35.
Shaikh NA, Downar E, Butany J. Amiodarone—an inhibitor of phospholipase activity: a comparative study of the inhibitory effects of amiodarone, chloroquine and chlorpromazine. Mol Cell Biochem. 1987;76:163–72.
Kennedy JA, Unger SA, Horowitz JD. Inhibition of carnitine palmitoyltransferase-1 in rat heart and liver by perhexiline and amiodarone. Biochem Pharmacol. 1996;52:273–80.
Fromenty B, Fisch C, Labbe G, Degott C, Deschamps D, Berson A, et al. Amiodarone inhibits the mitochondrial beta-oxidation of fatty acids and produces microvesicular steatosis of the liver in mice. J Pharmacol Exp Ther. 1990;255:1371–6.
Cronstein BN. The mechanism of action of methotrexate. Rheum Dis Clin N Am. 1997;23:739–55.
Baggott JE, Vaughn WH, Hudson BB. Inhibition of 5-aminoimidazole-4-carboxamide ribotide transformylase, adenosine deaminase and 5′-adenylate deaminase by polyglutamates of methotrexate and oxidized folates and by 5-aminoimidazole-4-carboxamide riboside and ribotide. Biochem J. 1986;236:193–200.
Dolezalová P, Krijt J, Chládek J, Nemcová D, Hoza J. Adenosine and methotrexate polyglutamate concentrations in patients with juvenile arthritis. Rheumatol Oxf Engl. 2005;44:74–9.
Langman G, Hall PM, Todd G. Role of non-alcoholic steatohepatitis in methotrexate-induced liver injury. J Gastroenterol Hepatol. 2001;16:1395–401.
Flowers MA, Heathcote J, Wanless IR, Sherman M, Reynolds WJ, Cameron RG, et al. Fulminant hepatitis as a consequence of reactivation of hepatitis B virus infection after discontinuation of low-dose methotrexate therapy. Ann Intern Med. 1990;112:381–2.
Shea B, Swinden MV, Tanjong Ghogomu E, Ortiz Z, Katchamart W, Rader T, et al. Folic acid and folinic acid for reducing side effects in patients receiving methotrexate for rheumatoid arthritis. Cochrane Database Syst Rev. 2013:CD000951.
Maybury CM, Samarasekera E, Douiri A, Barker JN, Smith CH. Diagnostic accuracy of noninvasive markers of liver fibrosis in patients with psoriasis taking methotrexate: a systematic review and meta-analysis. Br J Dermatol. 2014;170:1237–47.
Dreifuss FE, Langer DH, Moline KA, Maxwell JE. Valproic acid hepatic fatalities. II. US experience since 1984. Neurology. 1989;39:201–7.
van Zoelen MAD, de Graaf M, van Dijk MR, Bogte A, van Erpecum KJ, Rockmann H, et al. Valproic acid-induced DRESS syndrome with acute liver failure. Neth. J Med. 2012;70:155.
• Stewart JD, Horvath R, Baruffini E, Ferrero I, Bulst S, Watkins PB, et al. Polymerase γ gene POLG determines the risk of sodium valproate-induced liver toxicity. Hepatology. 2010;52:1791–6. In this study, POLG variant was shown to be associated with valproate toxicity.
Eadie MJ, Hooper WD, Dickinson RG. Valproate-associated hepatotoxicity and its biochemical mechanisms. Med Toxicol. 1988;3:85–106.
Coulter DL. Carnitine deficiency: a possible mechanism for valproate hepatotoxicity. Lancet Lond. Engl. 1984;1:689.
Böhles H, Sewell AC, Wenzel D. The effect of carnitine supplementation in valproate-induced hyperammonaemia. Acta Paediatr. Oslo Nor. 1992 1996;85:446–449.
Loomus GN, Aneja P, Bota RA. A case of peliosis hepatis in association with tamoxifen therapy. Am J Clin Pathol. 1983;80:881–3.
Saphner T, Triest-Robertson S, Li H, Holzman P. The association of nonalcoholic steatohepatitis and tamoxifen in patients with breast cancer. Cancer. 2009;115:3189–95.
Larosche I, Letteron P, Fromenty B, Vadrot N, Abbey-Toby A, Feldmann G, et al. Tamoxifen inhibits topoisomerases, depletes mitochondrial DNA, and triggers steatosis in mouse liver. J Pharmacol Exp Ther. 2007;321:526–35.
Raal FJ, Santos RD, Blom DJ, Marais AD, Charng M-J, Cromwell WC, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, for lowering of LDL cholesterol concentrations in patients with homozygous familial hypercholesterolaemia: a randomised, double-blind, placebo-controlled trial. Lancet Lond Engl. 2010;375:998–1006.
Li N, Li Q, Tian X-Q, Qian H-Y, Yang Y-J. Mipomersen is a promising therapy in the management of hypercholesterolemia: a meta-analysis of randomized controlled trials. Am J Cardiovasc Drugs Drugs Devices Interv. 2014;14:367–76.
Panta R, Dahal K, Kunwar S. Efficacy and safety of mipomersen in treatment of dyslipidemia: a meta-analysis of randomized controlled trials. J. Clin. Lipidol. 2015;9:217–25.
Hashemi N, Odze RD, McGowan MP, Santos RD, Stroes ESG, Cohen DE. Liver histology during mipomersen therapy for severe hypercholesterolemia. J Clin Lipidol. 2014;8:606–11.
Burnett J, Bell, Hooper, Watts. Mipomersen and other therapies for the treatment of severe familial hypercholesterolemia. Vasc Health Risk Manag 2012;651.
Cuchel M, Bloedon LT, Szapary PO, Kolansky DM, Wolfe ML, Sarkis A, et al. Inhibition of microsomal triglyceride transfer protein in familial hypercholesterolemia. N Engl J Med. 2007;356:148–56.
Cuchel M, Meagher EA, du Toit Theron H, Blom DJ, Marais AD, Hegele RA, et al. Efficacy and safety of a microsomal triglyceride transfer protein inhibitor in patients with homozygous familial hypercholesterolaemia: a single-arm, open-label, phase 3 study. Lancet. 2013;381:40–6.
JUXTAPID (lomitapide) Risk Evaluation and Mitigation Strategy (REMS) Program [Internet]. Available from: https://www.fda.gov/downloads/ForIndustry/UserFees/PrescriptionDrugUserFee/UCM361072.pdf
Costa MLV, Lima-Júnior RCP, Aragão KS, Medeiros RP, Marques-Neto RD, de Sá Grassi L, et al. Chemotherapy-associated steatohepatitis induced by irinotecan: a novel animal model. Cancer Chemother Pharmacol. 2014;74:711–20.
Gurzu S, Jung I, Comsulea M, Kadar Z, Azamfirei L, Molnar C. Lethal cardiotoxicity, steatohepatitis, chronic pancreatitis, and acute enteritis induced by capecitabine and oxaliplatin in a 36-year-old woman. Diagn. Pathol. [Internet]. 2013 [cited 2018 Apr 25]; 8. Available from: http://diagnosticpathology.biomedcentral.com/articles/10.1186/1746-1596-8-150
Liang J-T, Chen T-C, Huang J, Jeng Y-M, JC-H C. Treatment outcomes regarding the addition of targeted agents in the therapeutic portfolio for stage II-III rectal cancer undergoing neoadjuvant chemoradiation. Oncotarget. 2017;8:101832–46.
Miyake K, Hayakawa K, Nishino M, Morimoto T, Mukaihara S. Effects of oral 5-fluorouracil drugs on hepatic fat content in patients with colon cancer. Acad Radiol. 2005;12:722–7.
Donadon M, Vauthey J-N, Loyer EM, Charnsangavej C, Abdalla EK. Portal thrombosis and steatosis after preoperative chemotherapy with FOLFIRI-bevacizumab for colorectal liver metastases. World J Gastroenterol. 2006;12:6556–8.
Robinson SM, Wilson CH, Burt AD, Manas DM, White SA. Chemotherapy-associated liver injury in patients with colorectal liver metastases: a systematic review and meta-analysis. Ann Surg Oncol. 2012;19:4287–99.
Bodmer M, Sulz M, Stadlmann S, Droll A, Terracciano L, Krähenbühl S. Fatal liver failure in an adult patient with acute lymphoblastic leukemia following treatment with L-asparaginase. Digestion. 2006;74:28–32.
Pratt CB, Johnson WW. Duration and severity of fatty metamorphosis of the liver following L-asparaginase therapy. Cancer. 1971;28:361–4.
• Sahini N, Selvaraj S, Borlak J. Whole genome transcript profiling of drug induced steatosis in rats reveals a gene signature predictive of outcome. PLoS One. 2014;9:e114085. Study using whole genome transcription of rat models with DIFLD to identify differentially expressed genes to predict DIFLD.
Zhou J, Febbraio M, Wada T, Zhai Y, Kuruba R, He J, et al. Hepatic fatty acid transporter Cd36 is a common target of LXR, PXR, and PPAR gamma in promoting steatosis. Gastroenterology. 2008;134:556–67.
Fulgencio J-P, Kohl C, Girard J, Pegorier J-P. Troglitazone inhibits fatty acid oxidation and esterification, and gluconeogenesis in isolated hepatocytes from starved rats. Diabetes. 1996;45:1556–62.
Berson A. The anti-inflammatory drug, nimesulide (4-Nitro-2-phenoxymethane-sulfoanilide), uncouples mitochondria and induces mitochondrial permeability transition in human hepatoma cells: protection by albumin. J Pharmacol Exp Ther. 2006;318:444–54.
Berson A, Renault S, Letteron P, Robin M-A, Fromenty B, Fau D, et al. Uncoupling of rat and human mitochondria: a possible explanation for tacrine-induced liver dysfunction. Gastroenterology. 1996;110:1878–90.
Pessayre D, Mansouri A, Berson A, Fromenty B. Mitochondrial involvement in drug-induced liver injury. Handb Exp Pharmacol. 2010:311–65.
Watmough NJ, Bindoff LA, Birch-Machin MA, Jackson S, Bartlett K, Ragan CI, et al. Impaired mitochondrial beta-oxidation in a patient with an abnormality of the respiratory chain. Studies in skeletal muscle mitochondria. J Clin Invest. 1990;85:177–84.
Brivet FG, Nion I, Mégarbane B, Slama A, Brivet M, Rustin P, et al. Letters to the editor. J Hepatol. 2000;32:364–5.
Lewis W, Dalakas MC. Mitochondrial toxicity of antiviral drugs. Nat Med. 1995;1:417–22.
Chen CH, Vazquez-Padua M, Cheng YC. Effect of anti-human immunodeficiency virus nucleoside analogs on mitochondrial DNA and its implication for delayed toxicity. Mol Pharmacol. 1991;39:625–8.
Bissuel F, Bruneel F, Habersetzer F, Chassard D, Cotte L, Chevallier M, et al. Fulminant hepatitis with severe lactate acidosis in HIV-infected patients on didanosine therapy. J Intern Med. 1994;235:367–72.
Hammond E, McKinnon E, Nolan D. Human immunodeficiency virus treatment–induced adipose tissue pathology and lipoatrophy: prevalence and metabolic consequences. Clin Infect Dis. 2010;51:591–9.
Gougeon M-L, Pénicaud L, Fromenty B, Leclercq P, Viard J-P, Capeau J. Adipocytes targets and actors in the pathogenesis of HIV-associated lipodystrophy and metabolic alterations. Antivir Ther. 2004;9:161–77.
Estrada V, Serrano-Ríos M, Martínez Larrad MT, Villar NGP, González López A, Téllez MJ, et al. Leptin and adipose tissue maldistribution in HIV-infected male patients with predominant fat loss treated with antiretroviral therapy. J Acquir Immune Defic Syndr 1999. 2002;29:32–40.
Schilling C, Gilles M, Blum WF, Daseking E, Colla M, Weber-Hamann B, et al. Leptin plasma concentrations increase during antidepressant treatment with amitriptyline and mirtazapine, but not paroxetine and venlafaxine: leptin resistance mediated by antihistaminergic activity? J Clin Psychopharmacol. 2013;33:99–103.
• Domecq JP, Prutsky G, Leppin A, Sonbol MB, Altayar O, Undavalli C, et al. Drugs commonly associated with weight change: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100:363–70. Meta-analysis provides a comprehensive list of drugs that cause either weight gain or weight loss.
Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, Pennacchio LA, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461–5.
Kozlitina J, Smagris E, Stender S, Nordestgaard BG, Zhou HH, Tybjærg-Hansen A, et al. Exome-wide association study identifies a TM6SF2 variant that confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2014;46:352–6.
Chalasani N, Guo X, Loomba R, Goodarzi MO, Haritunians T, Kwon S, et al. Genome-wide association study identifies variants associated with histologic features of nonalcoholic fatty liver disease. Gastroenterology. 2010;139:1567–76. e1–6
Valenti L, Al-Serri A, Daly AK, Galmozzi E, Rametta R, Dongiovanni P, et al. Homozygosity for the patatin-like phospholipase-3/adiponutrin I148M polymorphism influences liver fibrosis in patients with nonalcoholic fatty liver disease. Hepatol. Baltim. Md. 2010;51:1209–17.
Liu Y-L, Patman GL, Leathart JBS, Piguet A-C, Burt AD, Dufour J-F, et al. Carriage of the PNPLA3 rs738409 C >G polymorphism confers an increased risk of non-alcoholic fatty liver disease associated hepatocellular carcinoma. J Hepatol. 2014;61:75–81.
•• Guzman CB, Duvvuru S, Akkari A, Bhatnagar P, Battioui C, Foster W, et al. Coding variants in PNPLA3 and TM6SF2 are risk factors for hepatic steatosis and elevated serum alanine aminotransferases caused by a glucagon receptor antagonist. Hepatol Commun. 2018;2:561–70. In this study, authors resourcefully conducted target gene approach of selected variants among diabetic subjects treated with glucagon receptor antagonists in two phase 2 trials, identifying a significant association of PNPL3 and TM6SF2 with drug-induced fatty liver.
Santos JDB, Mendonça AAS, Sousa RC, Silva TGS, Bigonha SM, Santos EC, et al. Food-drug interaction: anabolic steroids aggravate hepatic lipotoxicity and nonalcoholic fatty liver disease induced by trans fatty acids. Food Chem Toxicol. 2018;116:360–8.
Donthamsetty S, Bhave VS, Mitra MS, Latendresse JR, Mehendale HM. Nonalcoholic fatty liver sensitizes rats to carbon tetrachloride hepatotoxicity. Hepatology. 2007;45:391–403.
Luo Y, Rana P, Will Y. Palmitate increases the susceptibility of cells to drug-induced toxicity: an in vitro method to identify drugs with potential contraindications in patients with metabolic disease. Toxicol Sci. 2012;129:346–62.
Trost LC, Lemasters JJ. The mitochondrial permeability transition: a new pathophysiological mechanism for Reye’s syndrome and toxic liver injury. J Pharmacol Exp Ther. 1996;278:1000–5.
Lewis JH, Ranard RC, Caruso A, Jackson LK, Mullick F, Ishak KG, et al. Amiodarone hepatotoxicity: prevalence and clinicopathologic correlations among 104 patients. Hepatol Baltim Md. 1989;9:679–85.
Berson A, De Beco V, Lettéron P, Robin MA, Moreau C, Kahwaji JE, et al. Steatohepatitis-inducing drugs cause mitochondrial dysfunction and lipid peroxidation in rat hepatocytes. Gastroenterology. 1998;114:764–74.
Zaccara G, Messori A, Moroni F. Clinical pharmacokinetics of valproic acid--1988. Clin Pharmacokinet. 1988;15:367–89.
Aires CCP, IJlst L, Stet F, Prip-Buus C, de Almeida IT, Duran M, et al. Inhibition of hepatic carnitine palmitoyl-transferase I (CPT IA) by valproyl-CoA as a possible mechanism of valproate-induced steatosis. Biochem Pharmacol. 2010;79:792–9.
Knapp AC, Todesco L, Beier K, Terracciano L, Sagesser H, Reichen J, et al. Toxicity of valproic acid in mice with decreased plasma and tissue carnitine stores. J Pharmacol Exp Ther. 2007;324:568–75.
Zhao F, Xie P, Jiang J, Zhang L, An W, Zhan Y. The effect and mechanism of tamoxifen-induced hepatocyte steatosis in vitro. Int J Mol Sci. 2014;15:4019–30.
Aithal GP, Thomas JA, Kaye PV, Lawson A, Ryder SD, Spendlove I, et al. Randomized, placebo-controlled trial of pioglitazone in nondiabetic subjects with nonalcoholic steatohepatitis. Gastroenterology. 2008;135:1176–84.
Huang C-C, Hsu P-C, Hung Y-C, Liao Y-F, Liu C-C, Hour C-T, et al. Ornithine decarboxylase prevents methotrexate-induced apoptosis by reducing intracellular reactive oxygen species production. Apoptosis Int J Program Cell Death. 2005;10:895–907.
Tabassum H, Parvez S, Pasha ST, Banerjee BD, Raisuddin S. Protective effect of lipoic acid against methotrexate-induced oxidative stress in liver mitochondria. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc. 2010;48:1973–9.
Chan ESL, Montesinos MC, Fernandez P, Desai A, Delano DL, Yee H, et al. Adenosine A(2A) receptors play a role in the pathogenesis of hepatic cirrhosis. Br J Pharmacol. 2006;148:1144–55.
Masubuchi Y, Kano S, Horie T. Mitochondrial permeability transition as a potential determinant of hepatotoxicity of antidiabetic thiazolidinediones. Toxicology. 2006;222:233–9.
Peters RL, Edmondson HA, Mikkelsen WP, Tatter D. Tetracycline-induced fatty liver in nonpregnant patients. A report of six cases. Am J Surg. 1967;113:622–32.
Pride GL, Cleary RE, Hamburger RJ. Disseminated intravascular coagulation associated with tetracycline-induced hepatorenal failure during pregnancy. Am J Obstet Gynecol. 1973;115:585–6.
Wenk RE, Gebhardt FC, Bhagavan BS, Lustgarten JA, EF MC. Tetracycline-associated fatty liver of pregnancy, including possible pregnancy risk after chronic dermatologic use of tetracycline. J Reprod Med. 1981;26:135–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Niharika Samala declares no conflicts of interest; Naga Chalasani reports several consulting agreements and research grants from Pharmaceutical Companies but declares that they are not relevant for the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Drug-Induced Liver Injury.
Rights and permissions
About this article
Cite this article
Samala, N., Chalasani, N. Drug-Induced Fatty Liver Disease. Curr Hepatology Rep 17, 260–269 (2018). https://doi.org/10.1007/s11901-018-0418-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-018-0418-6