Abstract
Purpose of Review
Defective cell–mediated immunity is a major risk factor for cryptococcosis, a fatal disease if untreated. Cryptococcal meningitis (CM), the main presentation of disseminated disease, occurs through hematogenous spread to the brain from primary pulmonary foci, facilitated by yeast virulence factors. We revisit remarkable recent improvements in the prevention, diagnosis and management of CM.
Recent Findings
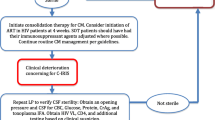
Cryptococcal antigen (CrAg), main capsular polysaccharide of Cryptococcus spp. is detectable in blood and cerebrospinal fluid of infected patients with point of care lateral flow assays. Recent World Health Organization guidelines recommend 7-day amphotericin B plus flucytosine, then 7-day high dose (1200 mg/day) fluconazole for induction treatment of HIV-associated CM. Management of raised intracranial pressure, a consequence of CM, should rely mainly on daily therapeutic lumbar punctures until normalisation. In HIV-associated CM, following introduction of antifungal therapy, (re)initiation of antiretroviral therapy should be delayed by 4–6 weeks to prevent immune reconstitution inflammatory syndrome, common in CM.
Summary
CM is a fatal disease whose diagnosis has recently been simplified. Treatment should always include antifungal combination therapy and management of raised intracranial pressure. Screening for immune deficiency should be mandatory in all patients with cryptococcosis.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kwon-Chung KJ, Fraser JA, Doering TL, Wang Z, Janbon G, Idnurm A, et al. Cryptococcus neoformans and Cryptococcus gattii, the etiologic agents of cryptococcosis. Cold Spring Harbor Perspect Med. 2014;4(7):a019760. https://doi.org/10.1101/cshperspect.a019760.
• Rajasingham R, Smith RM, Park BJ, Jarvis JN, Govender NP, Chiller TM, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis. 2017;17(8):873–81. https://doi.org/10.1016/S1473-3099(17)30243-8 This paper gives an update on the epidemiology of cryptococcal meningitis cases worldwide, with an estimated number of cases of 223,000 and 180,000 deaths, mainly in sub-Saharan Africa.
Ni M, Feretzaki M, Sun S, Wang X, Heitman J. Sex in fungi. Annu Rev Genet. 2011;45:405–30.
Kwon-Chung KJ, Boekhout T, Fell JW, Diaz M. (1557) Proposal to conserve the name Cryptococcus gattii against C. hondurianus and C. bacillisporus (Basidiomycota, Hymenomycetes, Tremellomycetidae). Taxon. 2002;51(4):804–6.
Chen SC-A, Korman TM, Slavin MA, Marriott D, Byth K, Bak N, et al. Antifungal therapy and management of complications of cryptococcosis due to Cryptococcus gattii. Clin Infect Dis. 2013;57(4):543–51.
Hagen F, Khayhan K, Theelen B, Kolecka A, Polacheck I, Sionov E, et al. Recognition of seven species in the Cryptococcus gattii/Cryptococcus neoformans species complex. Fungal Genet Biol. 2015;78:16–48.
Kwon-Chung KJ, Bennett JE, Wickes BL, Meyer W, Cuomo CA, Wollenburg KR, et al. The case for adopting the “species complex” nomenclature for the etiologic agents of cryptococcosis. mSphere. 2017;2(1):e00357–16.
Lin X, Heitman J. The biology of the Cryptococcus neoformans species complex. Annu Rev Microbiol. 2006;60:69–105.
Casadevall A, Steenbergen JN, Nosanchuk JD. ‘Ready made’virulence and ‘dual use’ virulence factors in pathogenic environmental fungi—the Cryptococcus neoformans paradigm. Curr Opin Microbiol. 2003;6(4):332–7.
Litvintseva AP, Carbone I, Rossouw J, Thakur R, Govender NP, Mitchell TG. Evidence that the human pathogenic fungus Cryptococcus neoformans var. grubii may have evolved in Africa. PloS One. 2011;6(5):e19688.
Bliska JB, Casadevall A. Intracellular pathogenic bacteria and fungi—a case of convergent evolution? Nat Rev Microbiol. 2009;7(2):165–71.
Kronstad JW, Attarian R, Cadieux B, Choi J, D'souza CA, Griffiths EJ, et al. Expanding fungal pathogenesis: Cryptococcus breaks out of the opportunistic box. Nat Rev Microbiol. 2011;9(3):193–203.
Kozel T, Gotschlich E. The capsule of Cryptococcus neoformans passively inhibits phagocytosis of the yeast by macrophages. J Immunol. 1982;129(4):1675–80.
O'Meara TR, Alspaugh JA. The Cryptococcus neoformans capsule: a sword and a shield. Clin Microbiol Rev. 2012;25(3):387–408.
Chammard TB, Temfack E, Lortholary O, Alanio A. Diagnostic and therapeutic strategies in cryptococcosis: impact on outcome. Mem Inst Oswaldo Cruz. 2018;113(7).
Rodrigues ML, Nakayasu ES, Oliveira DL, Nimrichter L, Nosanchuk JD, Almeida IC, et al. Extracellular vesicles produced by Cryptococcus neoformans contain protein components associated with virulence. Eukaryot Cell. 2008;7(1):58–67.
Nosanchuk JD, Casadevall A. The contribution of melanin to microbial pathogenesis. Cell Microbiol. 2003;5(4):203–23.
Shea JM, Kechichian TB, Luberto C, Del Poeta M. The cryptococcal enzyme inositol phosphosphingolipid-phospholipase C confers resistance to the antifungal effects of macrophages and promotes fungal dissemination to the central nervous system. Infect Immun. 2006;74(10):5977–88.
Shi M, Li SS, Zheng C, Jones GJ, Kim KS, Zhou H, et al. Real-time imaging of trapping and urease-dependent transmigration of Cryptococcus neoformans in mouse brain. J Clin Invest. 2010;120(5):1683–93.
Dromer F, Mathoulin-Pélissier S, Launay O, Lortholary O, Group FCS. Determinants of disease presentation and outcome during cryptococcosis: the CryptoA/D study. PLoS Med. 2007;4(2):e21.
Garcia-Hermoso D, Janbon G, Dromer F. Epidemiological evidence for dormant Cryptococcus neoformans infection. J Clin Microbiol. 1999;37(10):3204–9.
Alanio A, Vernel-Pauillac F, Sturny-Leclère A, Dromer F. Cryptococcus neoformans host adaptation: toward biological evidence of dormancy. mBio. 2015;6(2):e02580–14.
Charlier C, Chrétien F, Baudrimont M, Mordelet E, Lortholary O, Dromer F. Capsule structure changes associated with Cryptococcus neoformans crossing of the blood-brain barrier. Am J Pathol. 2005;166(2):421–32.
Chrétien F, Lortholary O, Kansau I, Neuville S, Gray F, Dromer F. Pathogenesis of cerebral Cryptococcus neoformans infection after fungemia. J Infect Dis. 2002;186(4):522–30.
Charlier C, Nielsen K, Daou S, Brigitte M, Chretien F, Dromer F. Evidence of a role for monocytes in dissemination and brain invasion by Cryptococcus neoformans. Infect Immun. 2009;77(1):120–7.
Santiago-Tirado FH, Onken MD, Cooper JA, Klein RS, Doering TL. Trojan horse transit contributes to blood-brain barrier crossing of a eukaryotic pathogen. mBio. 2017;8(1):e02183–16.
Neofytos D, Fishman J, Horn D, Anaissie E, Chang CH, Olyaei A, et al. Epidemiology and outcome of invasive fungal infections in solid organ transplant recipients. Transpl Infect Dis. 2010;12(3):220–9.
Camargo JF. Donor-derived infections in solid organ transplant recipients: challenging the 30-day paradigm. Transpl Infect Dis. 2017;19(2):e12665.
Kusne S, Taranto S, Covington S, Kaul D, Blumberg E, Wolfe C, et al. Coccidioidomycosis transmission through organ transplantation: a report of the OPTN ad hoc disease transmission advisory committee. Am J Transplant. 2016;16(12):3562–7.
Bernard C, Maucort-Boulch D, Varron L, Charlier C, Sitbon K, Freymond N, et al. Cryptococcosis in sarcoidosis: cryptOsarc, a comparative study of 18 cases. QJM Int J Med. 2013;106(6):523–39.
Hutto JO, Bryan CS, Greene FL, White CJ, Gallin JI. Cryptococcosis of the colon resembling Crohn's disease in a patient with the hyperimmunoglobulinemia E-recurrent infection (Job's) syndrome. Gastroenterology. 1988;94(3):808–12.
Jacobs DH, Macher AM, Handler R, Bennett JE, Collen MJ, Gallin JI. Esophageal cryptococcosis in a patient with the hyperimmunoglobulin E-recurrent infection (Job's) syndrome. Gastroenterology. 1984;87(1):201–3.
Garty BZ, Wolacfr B, Ashkenazi S, Weisman Y, Rachmel A, Nitzan M. Cryptococcal meningitis in a child with hyperimmunoglobulin E syndrome. Pediatr Allergy Immunol. 1995;6(3):175–7.
Lanternier F, Cypowyj S, Picard C, Bustamante J, Lortholary O, Casanova J-L, et al. Primary immunodeficiencies underlying fungal infections. Curr Opin Pediatr. 2013;25(6):736.
Pilmis B, Puel A, Lortholary O, Lanternier F. New clinical phenotypes of fungal infections in special hosts. Clin Microbiol Infect. 2016;22(8):681–7.
Chong I, Wang KY, Lincoln CM. Cryptococcal meningitis in a multiple sclerosis patient treated with Fingolimod: a case report and review of imaging findings. Clin Imaging. 2019;54:53–6.
Gundacker ND, Jordan SJ, Jones BA, Drwiega JC, Pappas PG, editors. Acute cryptococcal immune reconstitution inflammatory syndrome in a patient on natalizumab. Open forum infectious diseases; 2016: Oxford University Press.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European organization for research and treatment of cancer/invasive fungal infections cooperative group and the national institute of allergy and infectious diseases mycoses study group (EORTC/MSG) consensus group. Clin Infect Dis. 2008;46(12):1813–21.
Lazcano O, Speights JV, Strickler J, Bilbao J, Becker J, Diaz J. Combined histochemical stains in the differential diagnosis of Cryptococcus neoformans. Mod Pathol. 1993;6(1):80–4.
Bloomfield N, Gordon MA, Elmendorf DF Jr. Detection of Cryptococcus neoformans antigen in body fluids by latex particle agglutination. Proc Soc Exp Biol Med. 1963;114(1):64–7.
Jarvis JN, Percival A, Bauman S, Pelfrey J, Meintjes G, Williams GN, et al. Evaluation of a novel point-of-care cryptococcal antigen test on serum, plasma, and urine from patients with HIV-associated cryptococcal meningitis. Clin Infect Dis. 2011;53(10):1019–23.
Lindsley MD, Mekha N, Baggett HC, Surinthong Y, Autthateinchai R, Sawatwong P, et al. Evaluation of a newly developed lateral flow immunoassay for the diagnosis of cryptococcosis. Clin Infect Dis. 2011;53(4):321–5.
Vidal JE, Boulware DR. Lateral flow assay for cryptococcal antigen: an important advance to improve the continuum of HIV care and reduce cryptococcal meningitis-related mortality. Rev Inst Med Trop Sao Paulo. 2015;57:38–45.
Longley N, Jarvis JN, Meintjes G, Boulle A, Cross A, Kelly N, et al. Cryptococcal antigen screening in patients initiating ART in South Africa: a prospective cohort study. Clin Infect Dis. 2015;62(5):581–7.
Mfinanga S, Chanda D, Kivuyo SL, Guinness L, Bottomley C, Simms V, et al. Cryptococcal meningitis screening and community-based early adherence support in people with advanced HIV infection starting antiretroviral therapy in Tanzania and Zambia: an open-label, randomised controlled trial. Lancet. 2015;385(9983):2173–82. https://doi.org/10.1016/S0140-6736(15)60164-7.
•• Temfack E, Bigna JJ, Luma HN, Spijker R, Meintjes G, Jarvis JN, et al. Impact of routine Cryptococcal antigen screening and targeted preemptive fluconazole therapy in antiretroviral-naive human immunodeficiency virus–infected adults with CD4 cell counts< 100/μL: a systematic review and meta-analysis. Clin Infect Dis. 2018;68(4):688–98 This systematic review and meta-analysis emphasise the high rate of cryptococcal meningitis (more than a third) in asymptomatic patients with cryptococcal antigenemia, and the major role for pre-emptive fluconazole.
French N, Gray K, Watera C, Nakiyingi J, Lugada E, Moore M, et al. Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. Aids. 2002;16(7):1031–8.
Kozel TR, Bauman SK. CrAg lateral flow assay for cryptococcosis. Exp Opin Med Diagn. 2012;6(3):245–51.
• Temfack E, Kouanfack C, Mossiang L, Loyse A, Fonkoua MC, Molloy SF, et al. Cryptococcal antigen screening in asymptomatic HIV-infected antiretroviral naive patients in Cameroon and evaluation of the new semi-quantitative Biosynex CryptoPS test. Front Microbiol. 2018;9:409 In this study, the authors show the very important role of cryptococcal antigen screening for patients with advanced HIV disease, to guide pre-emptive treatment and identify asymptomatic cases of cryptococcal meningitis.
Jackson AT, van der Horst CM. Cryptococcosis in AIDS: new data but questions remain. OXFORD UNIV PRESS INC JOURNALS DEPT, 2001 EVANS RD, CARY, NC 27513 USA; 2016.
• Wake RM, Britz E, Sriruttan C, Rukasha I, Omar T, Spencer DC, et al. High cryptococcal antigen titers in blood are predictive of subclinical cryptococcal meningitis among human immunodeficiency virus-infected patients. Clin Infect Dis. 2017;66(5):686–92 In this study the authors found that about a third of asymptomatic HIV-infected patients with cryptococcal antigenemia had cryptococcal meningitis, and that the antigen titres in blood were a good tool to predict meningitis diagnosis.
Mpoza E, Mukaremera L, Kundura DA, Akampurira A, Luggya T, Tadeo KK, et al. Evaluation of a point-of-care immunoassay test kit ‘StrongStep’for cryptococcal antigen detection. PLoS One. 2018;13(1):e0190652.
Graybill JR, Sobel J, Saag M, van der Horst C, Powderly W, Cloud G, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. Clin Infect Dis. 2000;30(1):47–54.
Bicanic T, Brouwer AE, Meintjes G, Rebe K, Limmathurotsakul D, Chierakul W, et al. Relationship of cerebrospinal fluid pressure, fungal burden and outcome in patients with cryptococcal meningitis undergoing serial lumbar punctures. Aids. 2009;23(6):701–6.
•• Beardsley J, Wolbers M, Kibengo FM, Ggayi A-BM, Kamali A, Cuc NTK, et al. Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med. 2016;374(6):542–54 This major clinical trial definitely ruled out the use of concomitant steroids with induction phase antifungals for cryptococcal meningitis, as it led to higher mortality and higher impairment than placebo.
Newton PN, Thai LH, Tip NQ, Short JM, Chierakul W, Rajanuwong A, et al. A randomized, double-blind, placebo-controlled trial of acetazolamide for the treatment of elevated intracranial pressure in cryptococcal meningitis. Clin Infect Dis. 2002;35(6):769–72.
Rolfes MA, Hullsiek KH, Rhein J, Nabeta HW, Taseera K, Schutz C, et al. The effect of therapeutic lumbar punctures on acute mortality from cryptococcal meningitis. Clin Infect Dis. 2014;59(11):1607–14.
Fessler RD, Sobel J, Guyot L, Crane L, Vazquez J, Szuba MJ, et al. Management of elevated intracranial pressure in patients with Cryptococcal meningitis. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17(2):137–42.
Boyles TH, Gatley E, Wasserman S, Meintjes G. Brief report: flow rate of cerebrospinal fluid through a spinal needle can accurately predict intracranial pressure in cryptococcal meningitis. J Acquir Immune Defic Syndr. 2017;74(3):e64–e6.
Thakur KT, Mateyo K, Hachaambwa L, Kayamba V, Mallewa M, Mallewa J, et al. Lumbar puncture refusal in sub-Saharan Africa: a call for further understanding and intervention. Neurology. 2015;84(19):1988–90.
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(3):291–322.
Van der Horst CM, Saag MS, Cloud GA, Hamill RJ, Graybill JR, Sobel JD, et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. N Engl J Med. 1997;337(1):15–21.
Brouwer AE, Rajanuwong A, Chierakul W, Griffin GE, Larsen RA, White NJ, et al. Combination antifungal therapies for HIV-associated cryptococcal meningitis: a randomised trial. Lancet. 2004;363(9423):1764–7.
Day JN, Chau TT, Wolbers M, Mai PP, Dung NT, Mai NH, et al. Combination antifungal therapy for cryptococcal meningitis. N Engl J Med. 2013;368(14):1291–302.
Pappas PG, Chetchotisakd P, Larsen RA, Manosuthi W, Morris MI, Anekthananon T, et al. A phase II randomized trial of amphotericin B alone or combined with fluconazole in the treatment of HIV-associated cryptococcal meningitis. Clin Infect Dis. 2009;48(12):1775–83.
Nussbaum JC, Jackson A, Namarika D, Phulusa J, Kenala J, Kanyemba C, et al. Combination flucytosine and high-dose fluconazole compared with fluconazole monotherapy for the treatment of cryptococcal meningitis: a randomized trial in Malawi. Clin Infect Dis. 2010;50(3):338–44.
Gaskell KM, Rothe C, Gnanadurai R, Goodson P, Jassi C, Heyderman RS, et al. A prospective study of mortality from cryptococcal meningitis following treatment induction with 1200mg oral fluconazole in Blantyre, Malawi. PloS One. 2014;9(11):e110285.
Rothe C, Sloan DJ, Goodson P, Chikafa J, Mukaka M, Denis B, et al. A prospective longitudinal study of the clinical outcomes from cryptococcal meningitis following treatment induction with 800 mg oral fluconazole in Blantyre, Malawi. PloS One. 2013;8(6):e67311.
• Beyene T, Zewde AG, Balcha A, Hirpo B, Yitbarik T, Gebissa T, et al. Inadequacy of high-dose fluconazole monotherapy among cerebrospinal fluid Cryptococcal antigen (CrAg)–positive human immunodeficiency virus-infected persons in an Ethiopian CrAg screening program. Clin Infect Dis. 2017;65(12):2126–9 This study confirmed that the use of fluconazole monotherapy should not be an option for cryptococcal meningitis treatment.
•• Molloy SF, Kanyama C, Heyderman RS, Loyse A, Kouanfack C, Chanda D, et al. Antifungal combinations for treatment of cryptococcal meningitis in Africa. N Engl J Med. 2018;378(11):1004–17 This major phase III randomised clinical trial found 1 week of amphotericin B given with flucytosine to be noninferior to two weeks, flucytosine to be a better partner for amphotericin than fluconazole and for oral combination antifungal treatment with flucytosine and fluconazole to be an acceptable alternative to intravenous treatment. It has led to change the latest WHO guidelines for management of cryptococcal meningitis.
•• Tenforde MW, Shapiro AE, Rouse B, Jarvis JN, Li T, Eshun-Wilson I et al. Treatment for HIV-associated cryptococcal meningitis. Cochrane Database Syst Rev. 2018(7). This Cochrane review has confirmed the recent WHO guidelines using results from recent clinical trials for cryptococcal meningitis therapy.
World Health Organisation. Guidelines for the diagnosis, prevention, and management of cryptococcal disease in HIV-infected adults, adolescents and children. Supplement to the 2016 consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. 2018. https://www.who.int/hiv/pub/guidelines/cryptococcal-disease/en/. 2018.
Aguirre JPB, Hamid AMR. Amphotericin B deoxycholate versus liposomal amphotericin B: effects on kidney function. Cochrane Database Syst Rev. 2015;11.
Hamill RJ, Sobel JD, El-Sadr W, Johnson PC, Graybill JR, Javaly K, et al. Comparison of 2 doses of liposomal amphotericin B and conventional amphotericin B deoxycholate for treatment of AIDS-associated acute cryptococcal meningitis: a randomized, double-blind clinical trial of efficacy and safety. Clin Infect Dis. 2010;51(2):225–32.
Lawrence DS, Youssouf N, Molloy SF, Alanio A, Alufandika M, Boulware DR, et al. Correction to: AMBIsome Therapy Induction OptimisatioN (AMBITION): high dose AmBisome for cryptococcal meningitis induction therapy in sub-Saharan Africa: study protocol for a phase 3 randomised controlled non-inferiority trial. Trials. 2019;20(1):48. https://doi.org/10.1186/s13063-018-3155-9.
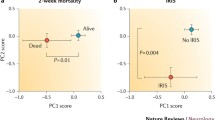
Boulware DR, Meya DB, Muzoora C, Rolfes MA, Huppler Hullsiek K, Musubire A, et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N Engl J Med. 2014;370(26):2487–98.
•• Eshun-Wilson I, Okwen MP, Richardson M, Bicanic T. Early versus delayed antiretroviral treatment in HIV-positive people with cryptococcal meningitis. Cochrane Database Syst Rev. 2018(7). This Cochrane review has reconfirmed the need to delay antiretroviral therapy initiation for at least 4 weeks from initiation of antifungal treatment for cryptococcal meningitis.
Haddow LJ, Colebunders R, Meintjes G, Lawn SD, Elliott JH, Manabe YC, et al. Cryptococcal immune reconstitution inflammatory syndrome in HIV-1-infected individuals: proposed clinical case definitions. Lancet Infect Dis. 2010;10(11):791–802.
Sun H-Y, Singh N. Immune reconstitution inflammatory syndrome in non-HIV immunocompromised patients. Curr Opin Infect Dis. 2009;22(4):394–402.
Legris T, Massad M, Purgus R, Vacher-Coponat H, Ranque S, Girard N, et al. Immune reconstitution inflammatory syndrome mimicking relapsing cryptococcal meningitis in a renal transplant recipient. Transpl Infect Dis. 2011;13(3):303–8.
Singh N, Sifri CD, Silveira FP, Miller R, Gregg KS, Huprikar S, et al. Cryptococcosis in patients with cirrhosis of the liver and posttransplant outcomes. Transplantation. 2015;99(10):2132–41.
Ingram PR, Howman R, Leahy MF, Dyer JR. Cryptococcal immune reconstitution inflammatory syndrome following alemtuzumab therapy. Clin Infect Dis. 2007;44(12):e115–e7.
• Dellière S, Guery R, Candon S, Rammaert B, Aguilar C, Lanternier F, et al. Understanding pathogenesis and care challenges of immune reconstitution inflammatory syndrome in fungal infections. J Fungi. 2018;4(4):139 This review aims to understand the recent challenges of immune reconstitution inflammatory syndrome in all fungal infections, including cryptococcal meningitis.
Legrand F, Lecuit M, Dupont B, Bellaton E, Huerre M, Rohrlich P-S, et al. Adjuvant corticosteroid therapy for chronic disseminated candidiasis. Clin Infect Dis. 2008;46(5):696–702.
Lortholary O, Fontanet A, Mémain N, Martin A, Sitbon K, Dromer F, et al. Incidence and risk factors of immune reconstitution inflammatory syndrome complicating HIV-associated cryptococcosis in France. Aids. 2005;19(10):1043–9.
Shearer GM. HIV-induced immunopathogenesis. Immunity. 1998;9(5):587–93.
Becker Y. The changes in the T helper 1 (Th1) and T helper 2 (Th2) cytokine balance during HIV-1 infection are indicative of an allergic response to viral proteins that may be reversed by Th2 cytokine inhibitors and immune response modifiers–a review and hypothesis. Virus Genes. 2004;28(1):5–18.
Sun H-Y, Alexander BD, Huprikar S, Forrest GN, Bruno D, Lyon GM, et al. Predictors of immune reconstitution syndrome in organ transplant recipients with cryptococcosis: implications for the management of immunosuppression. Clin Infect Dis. 2014;60(1):36–44.
Singh N, Lortholary O, Alexander BD, Gupta KL, John GT, Pursell K, et al. Allograft loss in renal transplant recipients with Cryptococcus neoformans associated immune reconstitution syndrome. Transplantation. 2005;80(8):1131–3.
Rhein J, Bahr NC, Morawski BM, Schutz C, Zhang Y, Finkelman M et al, editors. Detection of high cerebrospinal fluid levels of (1→ 3)-β-d-glucan in cryptococcal meningitis. Open forum infectious diseases; 2014: Oxford University Press.
Müller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger M. Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10(4):251–61.
Manabe YC, Campbell JD, Sydnor E, Moore RD. Immune reconstitution inflammatory syndrome: risk factors and treatment implications. J Acquir Immune Defic Syndr. 2007;46(4):456–62.
Chang CC, Dorasamy AA, Gosnell BI, Elliott JH, Spelman T, Omarjee S, et al. Clinical and mycological predictors of cryptococcosis-associated immune reconstitution inflammatory syndrome. Aids. 2013;27(13):2089–99.
Yoon HA, Nakouzi A, Chang CC, Kuniholm MH, Carreño LJ, Wang T, et al. Association between plasma antibody responses and risk for Cryptococcus-associated immune reconstitution inflammatory syndrome. J Infect Dis. 2018;219(3):420–8.
Chang CC, Lim A, Omarjee S, Levitz SM, Gosnell BI, Spelman T, et al. Cryptococcosis-IRIS is associated with lower cryptococcus-specific IFN-γ responses before antiretroviral therapy but not higher T-cell responses during therapy. J Infect Dis. 2013;208(6):898–906.
Boulware DR, Meya DB, Bergemann TL, Wiesner DL, Rhein J, Musubire A, et al. Clinical features and serum biomarkers in HIV immune reconstitution inflammatory syndrome after cryptococcal meningitis: a prospective cohort study. PLoS Med. 2010;7(12):e1000384.
Boulware DR, Bonham SC, Meya DB, Wiesner DL, Park GS, Kambugu A, et al. Paucity of initial cerebrospinal fluid inflammation in cryptococcal meningitis is associated with subsequent immune reconstitution inflammatory syndrome. J Infect Dis. 2010;202(6):962–70.
Psichogiou M, Basoulis D, Tsikala-Vafea M, Vlachos S, Kapelios CJ, Daikos GL. Integrase strand transfer inhibitors and the emergence of immune reconstitution inflammatory syndrome (IRIS). Curr HIV Res. 2017;15(6):405–10.
Vitoria M, Ford N, Clayden P, Pozniak AL, Hill AM. When could new antiretrovirals be recommended for national treatment programmes in low-income and middle-income countries: results of a WHO think tank. Curr Opin HIV AIDS. 2017;12(4):414–22.
Gaube G, De Castro N, Gueguen A, Lascoux C, Zagdanski A, Alanio A, et al. Treatment with adalimumab for severe immune reconstitution inflammatory syndrome in an HIV-infected patient presenting with cryptococcal meningitis. Med Mal Infect. 2016;46(3):154–6.
Brunel A-S, Reynes J, Tuaillon E, Rubbo P-A, Lortholary O, Montes B, et al. Thalidomide for steroid-dependent immune reconstitution inflammatory syndromes during AIDS. Aids. 2012;26(16):2110–2.
Scemla A, Gerber S, Duquesne A, Parize P, Martinez F, Anglicheau D, et al. Dramatic improvement of severe cryptococcosis-induced immune reconstitution syndrome with adalimumab in a renal transplant recipient. Am J Transplant. 2015;15(2):560–4.
Acknowledgements
The authors wish to thank Dr. John C.M. Brust for providing the full review of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Elvis Temfack, David Lawrence, Sarah Delliere, Angela Loyse each declare no potential conflicts of interest. Alexandre Alanio reports personal fees (Educational symposium) from Gilead sciences, outside the submitted work. Fanny Lanternier reports personal fees from Gilead, and from Basilea, outside the submitted work. Olivier Lortholary reports personal fees (Speaker during congresses) from Gilead, Merck, Pfizer, Astellas, outside the submitted work. Timothée Boyer-Chammard reports personal fees (Educational symposium) from Gilead Science, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Infection
Rights and permissions
About this article
Cite this article
Temfack, E., Boyer-Chammard, T., Lawrence, D. et al. New Insights Into Cryptococcus Spp. Biology and Cryptococcal Meningitis. Curr Neurol Neurosci Rep 19, 81 (2019). https://doi.org/10.1007/s11910-019-0993-0
Published:
DOI: https://doi.org/10.1007/s11910-019-0993-0