Abstract
Purpose of Review
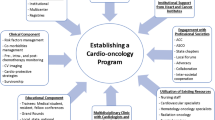
Cardio-oncology is a growing multi-disciplinary field that focuses on treating and preventing cardiovascular complications in cancer survivors and patients. This review summarizes the current clinical needs and system-based approaches to target barriers of care.
Recent Findings
The field of cardio-oncology has experienced significant growth in recent years, and an increasing number of programs have been developed across the nation to provide improved and multi-disciplinary care to this patient population. Despite this burgeoning growth, practitioners in the field continue to face important challenges which include lack of administrative and departmental support, funding limitations, and gaps in the areas of mentoring, education, and research.
Summary
Despite continued growth, cardio-oncology providers continue to face a multitude of challenges. Early inclusion of multi-disciplinary stakeholders, oncologists, cardiovascular team members, and administrative leadership provides an opportunity to collaborate and achieve unique patient care and health system benefits, such as prevention of adverse cardiovascular outcomes, and facilitates the delivery of optimal oncologic treatment.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bovelli D, Plataniotis G, Roila F. Cardiotoxicity of chemotherapeutic agents and radiotherapy-related heart disease: ESMO clinical practice guidelines. Ann Oncol : official journal of the European Society for Medical Oncology. 2010;21(Suppl 5):v277–82.
Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53(24):2231–47.
• Fradley MG, Brown AC, Shields B, Viganego F, Damrongwatanasuk R, Patel AA, et al. Developing a comprehensive cardio-oncology program at a cancer institute: the Moffitt Cancer Center Experience. Oncol Rev. 2017;11(2):340 This article details the experience of developing a cardio-oncology program and provides an overview of the challenges faced and practical solution suggestions.
American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2016–2017. Atlanta: American Cancer Society; 2016.
• Lancellotti P, Suter TM, López-Fernández T, Galderisi M, Lyon AR, Van der Meer P, et al. Cardio-oncology services: rationale, organization, and implementation. A report from the ESC Cardio-Oncology council. Eur Heart J. 2018;2018:ehy453 A comprehensive review article by the European Society of Cardiology Cardio-Oncology Council that discusses the rationale, organization, and implementation of cardio-oncology services.
Barac A, Murtagh G, Carver JR, Chen MH, Freeman AM, Herrmann J, et al. Cardiovascular health of patients with cancer and cancer survivors: a roadmap to the next level. J Am Coll Cardiol. 2015;65(25):2739–46.
Herrmann J, Lerman A, Sandhu NP, Villarraga HR, Mulvagh SL, Kohli M. Evaluation and management of patients with heart disease and cancer: cardio-oncology. Mayo Clin Proc. 2014;89(9):1287–306.
Armenian SH, Lacchetti C, Barac A, Carver J, Constine LS, Denduluri N, et al. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2017;35(8):893–911.
Zamorano JL, Lancellotti P, Rodriguez Munoz D, Aboyans V, Asteggiano R, Galderisi M, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: the Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(36):2768–801.
Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2014;15(10):1063–93.
Okwuosa TM, Barac A. Burgeoning cardio-oncology programs: challenges and opportunities for early career cardiologists/faculty directors. J Am Coll Cardiol. 2015;66(10):1193–7.
Swain SM, Whaley FS, Ewer MS. Congestive heart failure in patients treated with doxorubicin: a retrospective analysis of three trials. Cancer. 2003;97(11):2869–79.
Suter TM, Procter M, van Veldhuisen DJ, Muscholl M, Bergh J, Carlomagno C, et al. Trastuzumab-associated cardiac adverse effects in the herceptin adjuvant trial. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2007;25(25):3859–65.
Guarneri V, Lenihan DJ, Valero V, Durand JB, Broglio K, Hess KR, et al. Long-term cardiac tolerability of trastuzumab in metastatic breast cancer: the M.D. Anderson Cancer Center experience. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2006;24(25):4107–15.
Jovenaux L, Cautela J, Resseguier N, Pibarot M, Taouqi M, Orabona M, et al. Practices in management of cancer treatment-related cardiovascular toxicity: a cardio-oncology survey. Int J Cardiol. 2017;241:387–92.
Salem JE, Manouchehri A, Moey M, Lebrun-Vignes B, Bastarache L, Pariente A, et al. Cardiovascular toxicities associated with immune checkpoint inhibitors: an observational, retrospective, pharmacovigilance study. Lancet Oncol. 2018;19(12):1579–89.
Johnson DB, Balko JM, Compton ML, Chalkias S, Gorham J, Xu Y, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375(18):1749–55.
Gulati G, Heck SL, Ree AH, Hoffmann P, Schulz-Menger J, Fagerland MW, et al. Prevention of cardiac dysfunction during adjuvant breast cancer therapy (PRADA): a 2 x 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur Heart J. 2016;37(21):1671–80.
Avila MS, Ayub-Ferreira SM, de Barros Wanderley MR Jr, das Dores Cruz F, Goncalves Brandao SM, Rigaud VOC, et al. Carvedilol for prevention of chemotherapy-related cardiotoxicity: the CECCY trial. J Am Coll Cardiol. 2018;71(20):2281–90.
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–82.
Armstrong GT, Oeffinger KC, Chen Y, Kawashima T, Yasui Y, Leisenring W, et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol : official journal of the American Society of Clinical Oncology. 2013;31(29):3673–80.
Kenigsberg B, Wellstein A, Barac A. Left ventricular dysfunction in cancer treatment: is it relevant? JACC Heart Fail. 2018;6(2):87–95.
American College of Cardiology. Advancing the Cardiovascular Care of the Oncology Patient [Available from: https://www.acc.org/education-and-meetings/meetings/meeting-items/2018/06/06/06/54/2019-cardio-oncology. Accessed 10 Dec 2018.
United States Food and Drug Administration. FDA Public Workshop: cardiovascular toxicity assessment in oncology trials [Available from: https://www.fda.gov/drugs/newsevents/ucm513031.htm. Accessed 10 Dec 2018.
United States Food and Drug Administration. FDA Public Workshop: assessment of cardiovascular toxicities in immuno-oncology trials [Available from: https://www.fda.gov/Drugs/NewsEvents/ucm574741.htm. Accessed 10 Dec 2018.
NIH. Department of Health and Human Services [Available from: https://grants.nih.gov/grants/guide/pa-files/pa-16-035.html. Accessed 10 Dec 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardio-oncology
Rights and permissions
About this article
Cite this article
Agunbiade, T.A., Ottaviano, Y., Goswami, D. et al. Targeting Barriers of Systems of Care in a Growing Multi-disciplinary Field. Curr Oncol Rep 21, 36 (2019). https://doi.org/10.1007/s11912-019-0785-3
Published:
DOI: https://doi.org/10.1007/s11912-019-0785-3