Opinion statement
Central nervous system tumors are a major cause of morbidity and mortality in the United States. Outside of brain metastasis, low- and high-grade gliomas are the most common intrinsic brain tumors. Low-grade gliomas have a 5- and 10-year survival rate of 97 % and 91 %, respectively, when extent of resection is greater than 90 %. High-grade gliomas are extremely aggressive with the vast majority of patients experiencing recurrence and a median survival of 1 to 3 years. Survival of patients with both low- and high-grade gliomas is enhanced with maximal tumor resection. The pursuit of more aggressive extent of resection must be balanced with preservation of functional pathways. Several innovations in neurosurgical oncology have expanded our understanding of individualized patient neuroanatomy, physiology, and function. Emerging imaging technologies as well as intraoperative techniques have expanded our ability to resect maximal amounts of tumor while preserving essential function. Stimulation mapping of language and motor pathways is well-established for the safe resection of intrinsic brain lesions. Additional techniques including neuro-navigation, fluorescence-guided microsurgery using 5-aminolevulinic acid, intraoperative magnetic resonance imaging, and high-frequency ultrasonography can all be used to improve extent of resection in glioma patients.
Similar content being viewed by others
Introduction
With an estimated 18,820 new cases and 12,820 deaths per year, primary brain and central nervous system tumors are a major cause of morbidity and mortality in the United States [1]. More than 50 % of brain tumor cases are malignant gliomas (World Health Organization [WHO] grades III–IV), which have a propensity for diffuse brain invasion and recurrence after initial treatment. Glioblastoma (WHO grade IV) have a median survival of 12.2 to 18.2 months, while anaplastic astrocytomas (WHO grade III) have a 41-month median survival [2, 3]. Patients with low-grade gliomas have a better prognosis, with median survival times ranging between 4.6 to 6.5 years and median time to malignant progression of 8.8 to 11.4 years when extent of resection is greater than 90 % [4]. Even so, 50 %–75 % of patients with low-grade gliomas will eventually expire from their disease.
Microsurgery plays a central role in glioma management; however, because of a lack of class I evidence, there is no general consensus regarding the value of extent of glioma resection to improve patient outcome and quality of life. Radical resections of flair or contrast-enhancing tumor can be difficult to achieve due to proximity to eloquent structures and uncertainty about tumor margins. Much focus has been aimed at surgical techniques to improve extent of resection while minimizing morbidity. Intraoperative neurophysiological stimulation testing, intraoperative magnetic resonance imaging (iMRI), fluorescence-guided surgery using 5-aminolevulinic acid (5-ALA), and intraoperative ultrasound are all intraoperative tools used to improve extent of tumor resection. The value of mapping language and motor pathways has been well-documented for the safe removal of intrinsic brain tumors. Cumulative evidence suggests that a more extensive surgical resection is associated with longer survival and improved quality of life for both low- and high-grade gliomas. In this article, we focus on the evidence supporting the role of surgery for gliomas and modalities to assist with surgical resection.
Understanding the value of extent of resection in glioma surgery
With the exception of WHO grade I gliomas, patients with both low- and high-grade gliomas are likely to encounter recurrence. The value of extent of resection to improve outcome remains controversial. Mounting evidence, however, places extent of resection alongside patient age, tumor histology, performance, and IDH status as predictive of patient outcome [5–10]. Over the past 2 decades, significant emphasis has been given to understanding the effect of glioma resection on progression-free, overall survival, and time to malignant progression.
Low-grade glioma
A total of 21 studies since 1990 have examined the effect of extent of resection on patient survival and tumor progression for low-grade gliomas [4, 6–9, 11–26]. Different methods of calculating tumor volume can yield dramatically divergent results (Fig. 1). Commonly used methods include extent of resection as determined by surgeon or radiologist interpretation of postoperative imaging, 2-dimensional measurements, and 3-dimensional volumetric analysis. Volumetric analysis is the gold standard for most accurate calculations. Eight studies of low-grade glioma did not use volumetric analysis, with seven studies showing evidence in support of extent of resection as a predictor of either 5-year progression-free or overall survival [7, 16, 19, 20, 22, 26, 27]. Five studies used volumetric analysis of extent of resection with four validating a statistically significant improvement in 5-year survival with maximum extent of resection [3, 5, 28–30•]. Taken together, the literature shows a mean survival benefit from 61.1 to 90 months with maximal resection (Fig. 2, Table 1) [4, 21, 31••, 32].
Overlay of survival curves for total, subtotal, and partial resections for low-grade (A) (Reprinted from Smith et al. [4] with permission; copyright 2008, American Society of Clinical Oncology. All rights reserved); and high-grade (B) gliomas (Reprinted from Sanai et al. [30•]; copyright 2011, American Association of Neurological Surgeons).
The value of surgical resection for low-grade gliomas has been further validated in a population-based study of Norwegian patients [33••]. Jakola et al. [33••] reviewed 153 patients treated at two university hospitals serving adjacent geographical regions. Treatment strategy in individualized patients was dependent on patient residential address. Neurosurgeons from hospital A favored tumor biopsy and watchful waiting, whereas hospital B advocated early resection. Median follow-up was 7 years for both hospitals. Overall survival was superior with early resection. Patients receiving biopsy only had a median survival of 5.9 years, whereas the group receiving early resection did not reach median survival by the end of the study period. Estimated 5-year survival was 60 % for biopsy patients and 74 % for those receiving early surgery. The challenge, therefore, is to offer maximal resection for patients with low-grade glioma while preserving quality of life and limiting postoperative neurologic complications [34, 35].
Early maximal surgical resection is the first therapeutic option to delay malignant transformation and increase patient survival. Malignant transformation of low-grade gliomas ranges from 4 to 29 months [36, 37]. Early studies suggested that 50 % of patients with diffuse low-grade WHO grade II gliomas will undergo transformation to anaplastic (WHO grade III) gliomas within 5 years [38]. To determine the impact of extent of resection on malignant transformation, Smith et al [4] retrospectively studied 216 patients with hemispheric low-grade gliomas. Median time to progression was 5.5 years, and median time to malignant transformation was 10.1 years. Patients with at least 90 % extent of resection had 5- and 8-year survival rates of 97 % and 91 %, respectively, whereas patients with less than 90 % extent of resection had 5- and 8-year survival rates of 76 % and 60 %, respectively. Extent of surgical resection strongly predicted malignant progression-free survival [4].
Seizures are a common presenting symptom in patients with gliomas. Patients with low-grade tumors often survive for many years [39], so achieving seizure control is important for maintaining an acceptable quality of life. Englot et al [40] performed a systematic literature review of seizure control outcomes in 1181 epilepsy patients after subtotal vs gross total lesionectomy or anatomically tailored resection including gross total resection with lesionectomy plus neocortical temporal lobectomy with hippocampectomy. Although no randomized clinical trials were identified, a clear benefit was seen with gross total lesionectomy. Forty-three percent of patients were seizure-free after subtotal lesionectomy, 79 % were seizure-free after gross total tumor resection, and 87 % were seizure-free after lesionectomy with hippocampectomy and/or temporal neocortical resection. These findings suggest that greater extent of resection for low-grade gliomas (gross total resection) offers not only long-term survival benefit but also seizure control.
High-grade glioma
There have been 31 studies to date examining the role of extent of resection to improve the survival of patients with high-grade gliomas [3, 5, 27–30•, 41–65]. Volumetric analysis of tumor volume was used in five of these studies, 60 % of which showed a significant survival benefit with greater extent of resection [3, 5, 28–30•]. Of the 24 nonvolumetric studies, 13 showed evidence supporting extent of resection as a significant predictor of either progression-free or overall survival. The effect of greater extent of resection was not as pronounced as with low-grade gliomas, with an increase from 64.9 to 75.2 months for WHO grade III and from 11.3 to 14.5 months in WHO grade IV gliomas (Fig. 2).
Although extent of resection is an important prognostic factor for survival in patients undergoing initial resection of glioblastoma, its value for recurrence remains less clear. Bloch et al [42•] performed a retrospective review analysis of 107 patients who were offered a second craniotomy at recurrence. Volumetric extent of resection was measured and of patients who received an initial subtotal resection a mean survival benefit was noted for those who had a gross total resection at recurrence vs subtotal resection (19 months gross total resection, 15.9 months subtotal resection) (Table 2) [42•]. Furthermore, in addition to age and Karnofsky Performance Score at recurrence, extent of resection at second surgery was an independent predictor of survival (not extent of resection at initial surgery).
Techniques to improve extent of resection
Advancements in neurosurgical technique have allowed for safer, more aggressive operations that maximize surgical resection while minimizing neurologic complications. Intraoperative stimulation mapping, fluorescence-guided resections, neuro-navigation, intraoperative magnetic resonance imaging (iMRI) and high-resolution ultrasonography are all tools used to safely maximize extent of resection in glioma patients.
Mapping functional pathways
A key concept in neurosurgery is the utilization of intraoperative stimulation mapping to identify functional pathways. Direct stimulation of the cerebral cortex was first employed by Foerster in 1931 and later revisited by Penfield in 1937 [66], aiding in the identification of motor and sensory representation in the human brain. Because of individual variability and pathway distortion from mass lesions, intraoperative cortical and subcortical stimulation has been adopted to identify and preserve these critical language and motor pathways. The prediction of cortical language sites through anatomical localization is inadequate due to marked variability between individuals, distortion of pathways from tumor mass effect, and reorganization of pathways through plasticity [67–74]. Speech arrest, anomia, and alexia for individual patients are located far outside of the anatomic boundaries of Broca’s area [75]. Furthermore, numerous studies have failed to predict the location of speech arrest using functional neuroimaging or anatomical predictions based on frontal anatomy [76–81]. Though the exact mechanism of stimulation effect is poorly understood, direct stimulation depolarizes a focal area of cortex, exciting local neurons inducing either excitation or inhibition. There is further diffusion of stimulation to distant areas via orthodromic and antidromic propagation [82]. Bipolar stimulation with 5 mm of tip separation minimized distant propagation, allowing only local diffusion (of 3–5 mm), more precise mapping, and better accuracy [83]. The resection margin should be greater than 1 cm from the identified functional language site, which results in fewer permanent language deficits [83]. Early mapping techniques in the setting of epilepsy surgery used large craniotomies exposing extensive regions of cortex to identify positive motor and language sites. These positive controls have since been phased out in brain tumor surgery where smaller exposures directly over the lesion are used and resection is driven by “negative sites” that possess no inducible language or motor function. Negative mapping strategies represent a shift in mapping techniques, keeping eloquent areas untouched and free from exposure [75]. Craniotomies can, therefore, be tailored to expose the tumor and up to 2 cm of surrounding brain.
Knowing that the majority of gliomas recur within 1–2 cm of the infiltrative margin, the brain tumor surgeon must balance the goal of maximal tumor resection with intraoperative motor and language mapping to preserve function [84]. Skirboll et al [85] performed intraoperative stimulation mapping in 28 patients, finding both cortical and subcortical functional language sites within infiltrative gliomas. It is, therefore, important to consider mapping functional pathways in tumors that not only are within the frontal operculum, but also tumors that abut this region.
Specialized neuroanesthesia is critical for a successful and uncomplicated awake craniotomy. Communication and expertise between surgery and anesthesiology ensure accurate intraoperative mapping. Awake craniotomies are associated with fewer postoperative complications and less intraoperative morbidity [84]. In our experience, we apply patient monitors (axillary temperature probe, blood pressure cuff, arterial line) and premedicate with 2 mg of midazolam and 50–100 μg of fentanyl prior to positioning. Sedation is achieved with propofol (up to 100 μg/kg/min) and remifentanil (0.07–2.0 μg/kg/h). Dexmedetomidine (up to 1 μg/kg/min) may be used as an alternative to propofol for select patients. Propofol/remifentanil is used during Foley catheter insertion and Mayfield head holder pin placement. A complete scalp block or local analgesia around the incision (a 1:1 mixture of 1 % lidocaine with 1:100,000 epinephrine, 0.5 % bupivacaine, plus 4.5 ml of 8.4 % sodium bicarbonate) is applied by the neurosurgeon. After skin incision and removal of the bone flap, all sedatives are discontinued, after which the patient is asked to take multiple deep breaths and hyperventilate before opening of dura. For select patients the dura can be infiltrated with lidocaine in the region around the middle meningeal artery. Before language and motor mapping commences, a dedicated IV line is filled with a 1 mg per kg bolus of propofol 6 inches from the vein if needed for suppression of an intraoperative grand mal seizure. Topical ice-cold Ringers lactate solution is available on the surgical field for seizure suppression [86]. After completion of mapping, sedation is resumed.
Mapping starts at 2 mA and increases to a maximum of 6 mA if necessary. A constant current generator delivers 1.25 millisecond biphasic square waves in 4-second trains at 60 Hz. One-mm bipolar electrodes separated by 5 mm are used for cortical stimulation testing. Approximately 10–20 numerically marked stimulation sites separated by 1 cm are placed on the field (Fig. 3). To improve accuracy and limit subclinical seizure activity, continuous electrocorticography is used throughout language mapping to monitor after-discharge potentials. All language stimulation testing is repeated at least three times and a positive site is defined as the inability to count, name objects, or read words during stimulation 66 % of times [75, 87]. Language testing seeks to identify sites responsible for speech arrest, anomia, and alexia with stimulation testing. Speech arrest is defined as discontinuation in number counting without simultaneous motor response [75]. Dysarthria can be distinguished from speech arrest by an absence of involuntary muscle contractions affecting speech [75]. Stimulation is applied for 3 seconds at sequential naming points during a slide presentation. To identify reading sites, the same stimulation is applied during a slide presentation of words. A 1-cm margin of tissue is measured and preserved in all cases around positive language sites to protect language function [5, 87].
Cortical stimulation testing used for identification of language sites in a patient with left frontal low-grade glioma (A). Numbered markers are placed 1 cm apart (B). Testing for speech arrest, naming, and reading-identified silent regions (C) through which the resection is carried out. Subcortical stimulation identifies additional naming sites within the arcuate fasciculus (panel C, site 11).
Long-term language function after intraoperative stimulation of dominant hemisphere language sites was evaluated by our series of 250 consecutive dominant hemisphere glioma patients (WHO grades II–IV) [75]. A total 145 of 250 (58 %) patients had at least one site identified, with intraoperative stimulation causing speech arrest, anomia, or alexia. A total of 63.6 % of patients had intact speech preoperatively, and 1 week after surgery 77.6 % of patients had speech return to their baseline preoperative function. However, speech worsened in 8.4 %, and 14.0 % developed new speech deficits [75]. Patients were re-evaluated 6 months after surgery and only 1.6 % (four of 243 surviving patients) had persistent language deficits [75]. Duffau et al [34] published similar results in their series of dominant hemisphere insular WHO grade II gliomas. Their series showed that despite 50 % of patients showing a temporary worsening of language function, all patients returned to baseline language function within 3 months, with 25 % improving in comparison to preoperative examination.
5-ALA and fluorescence-guided brain tumor surgery
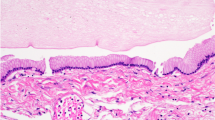
Complete removal of contrast-enhancing malignant gliomas can be difficult, and most neurosurgeons overestimate the degree of resection they are able to achieve [88, 89]. For this reason, technologies to improve extent of resection have been of interest. Neuro-navigation remains limited by registration constraints and brain shift throughout the course of the operation. Intraoperative ultrasound requires substantial experience to interpret the imaging. iMRI is expensive and available in only a number of specialized centers. 5-ALA is a nonfluorescent amino acid precursor that induces the accumulation of fluorescent porphyrins (mainly protoporphyrin IX) in malignant glioma. 5-ALA is produced in the mitochondria of all human cells, and under normal conditions 5-ALA and protoporphyrin IX are tightly controlled under a negative feedback loop [90]. However, exogenous 5-ALA leads to increased intracellular concentrations of fluorescent protoporphyrins in various malignant tumors, which peak 6 hours after administration and remains elevated for 12 hours [91–93]. Protoporphyrin IX has an absorption band strongest in the 380 ± 420 nm spectrum emitting red fluorescence at 635 nm and 704 nm in brain tissue [94]. 5-ALA induced fluorescence does not occur in healthy brain, and blood-brain barrier disruption in glioma allows the low lipid soluble 5-ALA to penetrate glioma tissue [93, 95].
5-ALA is administered either intravenously or orally 3 hours before the induction of general anesthesia with a goal of tumor removal 4–5 hours after 5-ALA administration [93]. A long-pass filter mounted to the surgical microscope allows for tumor visualization as the operator switches between white light and violet (Fig. 4).
5-ALA has been successfully used to better visualize malignant gliomas leading to improved extent of resection and longer patient survival. Microsurgical resections tailored for complete removal of all fluorescent material (“5-ALA complete resection”) offer greater 6-month and overall survival in malignant glioma without increase in postoperative neurologic deficits [93, 96, 97]. A phase III clinical trial conducted in Germany by the 5-ALA study group randomly assigned 322 patients with suspected malignant glioma to either conventional white light microsurgery or fluorescence-guided surgery assisted with 5-ALA. 5-ALA patients received 20 mg/kg of 5-ALA for a fluorescence-guided resection. After a mean follow-up of 35.4 months, 65 % of 5-ALA patients received complete removal of all contrast-enhancing tumor compared with 36 % of conventional white light microsurgery patients. 5-ALA patients experienced a 50 % improvement in 6-month progression-free survival (41 % vs 21.1 %) [97]. The literature provides class IIb evidence that 5-ALA-assisted extent of resection contributes to survival in glioblastoma [98]. 5-ALA is now combined with iMRI and direct cortical stimulation mapping to preserve eloquent functional pathways [99–101].
Neuro-navigation
Noninvasive functional neuroimaging techniques such as functional MRI (fMRI), magnetoencephalography (MEG), and positron emission topography were developed to generate working maps of functional brain pathways. Variability of individual neuroanatomy, distortion due to mass lesions, and reorganization caused by plasticity make classic anatomic identification of eloquent structures insufficient [68, 72]. These studies can offer individualized maps of eloquent areas and their relationship with mass lesions within the brain. For the brain tumor surgeon, these studies are an essential part of determining the risks associated with surgery and consulting patients about potential postoperative neurological outcomes [102–109]. They also allow for a generalized preoperative impression of where a pathway might be displaced in relationship to a space-occupying lesion. Neuro-navigation is widely used in brain tumor surgery and has been integrated with fMRI (commonly referred to as “functional neuro-navigation”) to determine cortical areas with sensory, motor, language, and visual function [104, 106].
Identification of subcortical pathways is critical to preventing injury to white matter pathways and preserving function. The current gold-standard method for assessing functional tissue cortically and subcortically is intraoperative stimulation testing. It is, however, advantageous to preoperatively and intraoperatively visualize white matter tractography and its spatial relationship to a brain tumor. Resting state coherence measured with MEG is capable of mapping functional connectivity of the brain, thereby offering valuable information for preoperative planning [103]. MEG’s potential to predict postoperative neurological outcome was investigated by Tarapore et al [108]. They measured resting whole brain MEG recordings from 79 subjects with unilateral gliomas near or within sensory, motor, or language areas during the preoperative and postoperative period. Patients with baseline decreased functional connectivity had a 29 % rate of new neurological deficits 1 week after surgery and 0 % at 6-month follow-up. However, patients with increased functional connectivity had a 60 % rate of new deficits at 1 week and 25 % at 6 months. This study, therefore, suggests that tumors with decreased resting state connectivity have a relatively low risk of postoperative neurologic deficits, while those with increased resting state connectivity are associated with higher risk of postoperative neurological deficits [108]. Though these rates of postoperative neurologic compromise are higher than that seen with awake cortical stimulation mapping, they offer a valuable option for those patients in whom awake surgery is contraindicated.
Positron emission tomography (PET) has also been used to map cortical language and motor areas in adult patients with brain tumors [105, 107]. Similar to other noninvasive imaging modalities, PET’s accuracy is inferior to intraoperative stimulation mapping, yielding 94 % sensitivity and 95 % specificity for identification of motor-associated brain areas [107]. Broca’s area is able to be identified in an estimated 66 % of brain tumor patients demarcated by a cerebral blood flow increase during verb generation in the posterior inferior frontal gyrus (frontal operculum) [105]. These modalities offer important adjuvants for preoperative planning and intraoperative guidance for brain tumor surgery.
iMRI
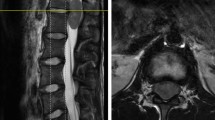
Over the past decade, MRI-guided brain tumor surgery has sought to enhance extent of tumor resection, quality of life, and patient survival. iMRI technology started with 0.5 Tesla systems, but the field has since evolved with 3 Tesla machines currently in use. Several studies have attempted to quantify iMRI effect on extent of tumor resection, but only a few address how iMRI affected the surgical plan, survival, and quality of life.
The main rationale for the use of iMRI over conventional neuro-navigation-guided resection is the avoidance of brain shift related to resected tumor, loss of cerebrospinal fluid, and tissue edema. Conventional neuro-navigation becomes progressively less reliable during surgery, while iMRI can be updated during surgery. Several studies have attempted to quantify the added value of iMRI in brain tumor surgery [110–120]. It has been used with success in surgery for low-grade gliomas, increasing both extent of resection and survival [12, 119, 121]. Schneider et al [119] studied 12 patients with low-grade gliomas who underwent surgery within a 0.5 Tesla iMRI suite. At the point in which the surgeon would have classically terminated the operation as well at the final end of the case, residual tumor was measured using iMRI. The initial extent of resection was 68 %. However, at final analysis, gross total resection was seen in 50 % of cases, 90 % resection in 42 % of cases, and less than 85 % resection in 8 % of cases. Claus et al [12] preformed a single-institution retrospective analysis of 156 patients with unifocal supratentorial low-grade gliomas using iMRI. They noted decreased death rates at 1, 2, and 5 years (1.9 %, 3.6 %, 17.6 %, respectively) compared with historical controls. Given concern that iMRI might lead to an increased rate of postoperative neurological deficits, Nimsky et al [115] reviewed their experience and found no difference.
iMRI for high-grade glioma has been shown to be more effective than conventional neuro-navigation-guided surgery for increasing extent of resection; however, studies examining survival, neurological outcome, and quality of life are limited. Published reports display an overall survival for glioblastoma patients of 13.3–18.5 months for gross total resection and 7.9–11.5 months for subtotal resection using iMRI [113, 120, 122, 123]. As with all surgical modalities, extent of glioma resection must be measured against quality of life and postoperative clinical performance.
Ultrasound-guided resections
Intraoperative ultrasound has been used in neurosurgery since the1960s, but its use in brain tumor surgery has been limited [124–127]. Using 3.5–7.5 MHz ultrasound probes, Le Roux et al [126] were the first to note that nearly all neoplasms, including low-grade tumors, were visible by intraoperative ultrasound. Pitfalls limiting its effectiveness include user-dependent interpretation, difficulty differentiating between tissue edema and tumor tissue, difficulty in detecting small lesions, and trouble deciphering between normal brain and pathologic tissue in low-grade tumors. Innovations in high-frequency ultrasound technology have improved image quality. However, there are still pitfalls limiting its usefulness to determine intraoperative extent of resection. Furthermore, it can be profoundly difficult to interpret imaging in the presence of blood products within the resection cavity. High-frequency ultrasound probes (7–15 MHz) have been introduced with promising results for high-grade gliomas. When compared with postoperative MRI, 90 %–95.5 % of patients receive gross total resection when used by experienced neurosurgeons [127]. However promising, no published studies to date have investigated overall or progression-free survival in glioma patients treated with microsurgery-assisted high-frequency ultrasound.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Barnholtz-Sloan JS, Sloan AE, Schwartz AG. Chapter 25: Cancer of the brain and other central nervous system. In: SEER Survival Monograph: Cancer Survival Among Adults: U.S. SEER Program, 1988–2001, Patient and Tumor Characteristics. Bethesda: National Cancer Institute, 2007. Available at: http://seer.cancer.gov/publications/survival/surv_brain.pdf. Accessed September 3, 2013.
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352(10):997–1003.
Keles GE, Chang EF, Lamborn KR, Tihan T, Chang CJ, Chang SM, et al. Volumetric extent of resection and residual contrast enhancement on initial surgery as predictors of outcome in adult patients with hemispheric anaplastic astrocytoma. J Neurosurg. 2006;105(1):34–40.
Smith JS, Chang EF, Lamborn KR, Chang SM, Prados MD, Cha S, et al. Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol. 2008;26(8):1338–45.
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001;95(2):190–8.
Lote K, Egeland T, Hager B, Stenwig B, Skullerud K, Berg-Johnsen J, et al. Survival, prognostic factors, and therapeutic efficacy in low-grade glioma: a retrospective study in 379 patients. J Clin Oncol. 1997;15(9):3129–40.
Nakamura M, Konishi N, Tsunoda S, Nakase H, Tsuzuki T, Aoki H, et al. Analysis of prognostic and survival factors related to treatment of low-grade astrocytomas in adults. Oncology. 2000;58(2):108–16.
Nicolato A, Gerosa MA, Fina P, Iuzzolino P, Giorgiutti F, Bricolo A. Prognostic factors in low-grade supratentorial astrocytomas: a uni-multivariate statistical analysis in 76 surgically treated adult patients. Surg Neurol. 1995;44(3):208–21.
Scerrati M, Roselli R, Iacoangeli M, Pompucci A, Rossi GF. Prognostic factors in low grade (WHO grade II) gliomas of the cerebral hemispheres: the role of surgery. J Neurol Neurosurg Psychiatry. 1996;61(3):291–6.
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, et al. IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360(8):765–73.
Bauman G, Pahapill P, Macdonald D, Fisher B, Leighton C, Cairncross G. Low grade glioma: a measuring radiographic response to radiotherapy. Can J Neurol Sci. 1999;26(1):18–22.
Claus EB, Horlacher A, Hsu L, Schwartz RB, Dello-Iacono D, Talos F, et al. Survival rates in patients with low-grade glioma after intraoperative magnetic resonance image guidance. Cancer. 2005;103(6):1227–33.
Ito S, Chandler KL, Prados MD, Lamborn K, Wynne J, Malec MK, et al. Proliferative potential and prognostic evaluation of low-grade astrocytomas. J Neurooncol. 1994;19(1):1–9.
Johannesen TB, Langmark F, Lote K. Progress in long-term survival in adult patients with supratentorial low-grade gliomas: a population-based study of 993 patients in whom tumors were diagnosed between 1970 and 1993. J Neurosurg. 2003;99(5):854–62.
Karim AB, Maat B, Hatlevoll R, Menten J, Rutten EH, Thomas DG, et al. A randomized trial on dose-response in radiation therapy of low-grade cerebral glioma: European Organization for Research and Treatment of Cancer (EORTC) Study 22844. Int J Radiat Oncol Biol Phys. 1996;36(3):549–56.
Leighton C, Fisher B, Bauman G, Depiero S, Stitt L, MacDonald D, et al. Supratentorial low-grade glioma in adults: an analysis of prognostic factors and timing of radiation. J Clin Oncol. 1997;15(4):1294–301.
North CA, North RB, Epstein JA, Piantadosi S, Wharam MD. Low-grade cerebral astrocytomas. Survival and quality of life after radiation therapy. Cancer. 1990;66(1):6–14.
Peraud A, Ansari H, Bise K, Reulen HJ. Clinical outcome of supratentorial astrocytoma WHO grade II. Acta Neurochir. 1998;140(12):1213–22.
Philippon JH, Clemenceau SH, Fauchon FH, Foncin JF. Supratentorial low-grade astrocytomas in adults. Neurosurgery. 1993;32(4):554–9.
Rajan B, Pickuth D, Ashley S, Traish D, Monro P, Elyan S, et al. The management of histologically unverified presumed cerebral gliomas with radiotherapy. Int J Radiat Oncol Biol Phys. 1994;28(2):405–13.
Sanai N, Berger MS. Glioma extent of resection and its impact on patient outcome. Neurosurgery. 2008;62(4):753–64.
Shaw E, Arusell R, Scheithauer B, O'Fallon J, O'Neill B, Dinapoli R, et al. Prospective randomized trial of low- versus high-dose radiation therapy in adults with supratentorial low-grade glioma: initial report of a North Central Cancer Treatment Group/Radiation Therapy Oncology Group/Eastern Cooperative Oncology Group study. J Clin Oncol. 2002;20(9):2267–76.
Shibamoto Y, Kitakabu Y, Takahashi M, Yamashita J, Oda Y, Kikuchi H, et al. Supratentorial low-grade astrocytoma. Correlation of computed tomography findings with effect of radiation therapy and prognostic variables. Cancer. 1993;72(1):190–5.
van Veelen ML, Avezaat CJ, Kros JM, van Putten W, Vecht C. Supratentorial low grade astrocytoma: prognostic factors, dedifferentiation, and the issue of early versus late surgery. J Neurol Neurosurg Psychiatry. 1998;64(5):581–7.
Whitton AC, Bloom HJ. Low grade glioma of the cerebral hemispheres in adults: a retrospective analysis of 88 cases. Int J Radiat Oncol Biol Phys. 1990;18(4):783–6.
Yeh SA, Ho JT, Lui CC, Huang YJ, Hsiung CY, Huang EY. Treatment outcomes and prognostic factors in patients with supratentorial low-grade gliomas. Br J Radiol. 2005;78(927):230–5.
McGirt MJ, Chaichana KL, Gathinji M, Attenello FJ, Than K, Olivi A, et al. Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J Neurosurg. 2009;110(1):156–62.
Keles GE, Anderson B, Berger MS. The effect of extent of resection on time to tumor progression and survival in patients with glioblastoma multiforme of the cerebral hemisphere. Surg Neurol. 1999;52(4):371–9.
Pope WB, Sayre J, Perlina A, Villablanca JP, Mischel PS, Cloughesy TF. MR imaging correlates of survival in patients with high-grade gliomas. AJNR Am J Neuroradiol. 2005;26(10):2466–74.
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS. An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg. 2011;115(1):3–8. A retrospective study using volumetric analysis and long-term patient outcomes to determine an extent of resection threshold for patients with glioblastoma.
Capelle L, Fontaine D, Mandonnet E, Taillandier L, Golmard JL, Bauchet L, et al. Spontaneous and therapeutic prognostic factors in adult hemispheric World Health Organization Grade II gliomas: a series of 1097 cases: clinical article. J Neurosurg. 2013;118(6):1157–68. A retrospective study showing 15 year survival for patients with low-grade glioma.
Schomas DA, Laack NN, Rao RD, Meyer FB, Shaw EG, O'Neill BP, et al. Intracranial low-grade gliomas in adults: 30-year experience with long-term follow-up at Mayo Clinic. Neuro Oncol. 2009;11(4):437–45.
Jakola AS, Myrmel KS, Kloster R, Torp SH, Lindal S, Unsgard G, et al. Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA. 2012;308(18):1881–8. A retrospective analysis showing the survival benefit of surgical resection over biopsy with watchful waiting for patients with low-grade glioma.
Duffau H, Moritz-Gasser S, Gatignol P. Functional outcome after language mapping for insular World Health Organization Grade II gliomas in the dominant hemisphere: experience with 24 patients. Neurosurg Focus. 2009;27(2):E7. doi:10.3171/2009.5.FOCUS0938.
Soffietti R, Baumert BG, Bello L, von Deimling A, Duffau H, Frenay M, et al. Guidelines on management of low-grade gliomas: report of an EFNS-EANO Task Force. Eur J Neurol. 2010;17(9):1124–33.
Frazier JL, Johnson MW, Burger PC, Weingart JD, Quinones-Hinojosa A. Rapid malignant transformation of low-grade astrocytomas: report of 2 cases and review of the literature. World Neurosurg. 2010;73(1):53–62.
Recht LD, Lew R, Smith TW. Suspected low-grade glioma: is deferring treatment safe? Ann Neurol. 1992;31(4):431–6.
Piepmeier J, Christopher S, Spencer D, Byrne T, Kim J, Knisel JP, et al. Variations in the natural history and survival of patients with supratentorial low-grade astrocytomas. Neurosurgery. 1996;38(5):872–8.
Ruda R, Bello L, Duffau H, Soffietti R. Seizures in low-grade gliomas: natural history, pathogenesis, and outcome after treatments. Neuro Oncol. 2012;14 Suppl 4:iv55–64.
Englot DJ, Han SJ, Berger MS, Barbaro NM, Chang EF. Extent of surgical resection predicts seizure freedom in low-grade temporal lobe brain tumors. Neurosurgery. 2012;70(4):921–8.
Barker 2nd FG, Prados MD, Chang SM, Gutin PH, Lamborn KR, Larson DA, et al. Radiation response and survival time in patients with glioblastoma multiforme. J Neurosurg. 1996;84(3):442–8.
Bloch O, Han SJ, Cha S, Sun MZ, Aghi MK, McDermott MW, et al. Impact of extent of resection for recurrent glioblastoma on overall survival: clinical article. J Neurosurg. 2012;117(6):1032–8. A retrospective analysis showing the value of extent of re-operation with maximal extent of resection for patients with recurrent glioblastoma.
Brown PD, Ballman KV, Rummans TA, Maurer MJ, Sloan JA, Boeve BF, et al. Prospective study of quality of life in adults with newly diagnosed high-grade gliomas. J Neurooncol. 2006;76(3):283–91.
Buckner JC, Schomberg PJ, McGinnis WL, Cascino TL, Scheithauer BW, O'Fallon JR, et al. A phase III study of radiation therapy plus carmustine with or without recombinant interferon-alpha in the treatment of patients with newly diagnosed high-grade glioma. Cancer. 2001;92(2):420–33.
Curran WJJ, Scott CB, Horton J, Nelson JS, Weinstein AS, Nelson DF, et al. Does extent of surgery influence outcome for astrocytoma with atypical or anaplastic foci (AAF)? A report from three Radiation Therapy Oncology Group (RTOG) trials. J Neurooncol. 1992;12(3):219–27.
Dinapoli RP, Brown LD, Arusell RM, Earle JD, O'Fallon JR, Buckner JC, et al. Phase III comparative evaluation of PCNU and carmustine combined with radiation therapy for high-grade glioma. J Clin Oncol. 1993;11(7):1316–21.
Duncan GG, Goodman GB, Ludgate CM, Rheaume DE. The treatment of adult supratentorial high grade astrocytomas. J Neurooncol. 1992;13(1):63–72.
Hollerhage HG, Zumkeller M, Becker M, Dietz H. Influence of type and extent of surgery on early results and survival time in glioblastoma multiforme. Acta Neurochir. 1991;113(1–2):31–7.
Huber A, Beran H, Becherer A, Prosenc N, Witzmann A. [Supratentorial glioma: analysis of clinical and temporal parameters in 163 cases]. Neurochirurgia. 1993;36(6):189–93.
Jeremic B, Grujicic D, Antunovic V, Djuric L, Stojanovic M, Shibamoto Y. Influence of extent of surgery and tumor location on treatment outcome of patients with glioblastoma multiforme treated with combined modality approach. J Neurooncol. 1994;21(2):177–85.
Kowalczuk A, Macdonald RL, Amidei C, Dohrmann III G, Erickson RK, Hekmatpanah J, et al. Quantitative imaging study of extent of surgical resection and prognosis of malignant astrocytomas. Neurosurgery. 1997;41(5):1028–36.
Lamborn KR, Chang SM, Prados MD. Prognostic factors for survival of patients with glioblastoma: recursive partitioning analysis. Neuro Oncol. 2004;6(3):227–35.
Levin VA, Yung WK, Bruner J, Kyritsis A, Leeds N, Gleason MJ, et al. Phase II study of accelerated fractionation radiation therapy with carboplatin followed by PCV chemotherapy for the treatment of anaplastic gliomas. Int J Radiat Oncol Biol Phys. 2002;53(1):58–66.
Nitta T, Sato K. Prognostic implications of the extent of surgical resection in patients with intracranial malignant gliomas. Cancer. 1995;75(11):2727–31.
Nomiya T, Nemoto K, Kumabe T, Takai Y, Yamada S. Prognostic significance of surgery and radiation therapy in cases of anaplastic astrocytoma: retrospective analysis of 170 cases. J Neurosurg. 2007;106(4):575–81.
Oszvald A, Guresir E, Setzer M, Vatter H, Senft C, Seifert V, et al. Glioblastoma therapy in the elderly and the importance of the extent of resection regardless of age. J Neurosurg. 2012;116(2):357–64.
Phillips TL, Levin VA, Ahn DK, Gutin PH, Davis RL, Wilson CB, et al. Evaluation of bromodeoxyuridine in glioblastoma multiforme: a Northern California Cancer Center Phase II study. Int J Radiat Oncol Biol Phys. 1991;21(3):709–14.
Prados MD, Gutin PH, Phillips TL, Wara WM, Larson DA, Sneed PK, et al. Highly anaplastic astrocytoma: a review of 357 patients treated between 1977 and 1989. Int J Radiat Oncol Biol Phys. 1992;23(1):3–8.
Puduvalli VK, Hashmi M, McAllister LD, Levin VA, Hess KR, Prados M, et al. Anaplastic oligodendrogliomas: prognostic factors for tumor recurrence and survival. Oncology. 2003;65(3):259–66.
Sandberg-Wollheim M, Malmstrom P, Stromblad LG, Anderson H, Borgstrom S, Brun A, et al. A randomized study of chemotherapy with procarbazine, vincristine, and lomustine with and without radiation therapy for astrocytoma grades 3 and/or 4. Cancer. 1991;68(1):22–9.
Shibamoto Y, Yamashita J, Takahashi M, Yamasaki T, Kikuchi H, Abe M. Supratentorial malignant glioma: an analysis of radiation therapy in 178 cases. Radiother Oncol. 1990;18(1):9–17.
Simpson JR, Horton J, Scott C, Curran WJ, Rubin P, Fischbach J, et al. Influence of location and extent of surgical resection on survival of patients with glioblastoma multiforme: results of three consecutive Radiation Therapy Oncology Group (RTOG) clinical trials. Int J Radiat Oncol Biol Phys. 1993;26(2):239–44.
Stark AM, Nabavi A, Mehdorn HM, Blomer U. Glioblastoma multiforme-report of 267 cases treated at a single institution. Surg Neurol. 2005;63(2):162–9.
Ushio Y, Kochi M, Hamada J, Kai Y, Nakamura H. Effect of surgical removal on survival and quality of life in patients with supratentorial glioblastoma. Neurol Med Chir. 2005;45(9):454–60.
Vecht CJ, Avezaat CJ, van Putten WL, Eijkenboom WM, Stefanko SZ. The influence of the extent of surgery on the neurological function and survival in malignant glioma. A retrospective analysis in 243 patients. J Neurol Neurosurg Psychiatry. 1990;53(6):466–71.
Penfield W, Boldrey E. Somatic motor and sensory representation in the cerebral cortex of man as studied by electrical stimulation. Brain. 1937;60(4):389–443. doi:10.1093/brain/60.4.389.
Herholz K, Thiel A, Wienhard K, Pietrzyk U, von Stockhausen HM, Karbe H, et al. Individual functional anatomy of verb generation. Neuroimage. 1996;3(3 Pt 1):185–94.
Ojemann G, Ojemann J, Lettich E, Berger M. Cortical language localization in left, dominant hemisphere. An electrical stimulation mapping investigation in 117 patients. J Neurosurg. 1989;71(3):316–26.
Ojemann GA. Individual variability in cortical localization of language. J Neurosurg. 1979;50(2):164–9.
Ojemann GA. Cortical organization of language. J Neurosci. 1991;11(8):2281–7.
Ojemann GA, Whitaker HA. Language localization and variability. Brain Lang. 1978;6(2):239–60.
Ojemann JG, Miller JW, Silbergeld DL. Preserved function in brain invaded by tumor. Neurosurgery. 1996;39(2):253–8.
Seitz RJ, Huang Y, Knorr U, Tellmann L, Herzog H, Freund HJ. Large-scale plasticity of the human motor cortex. Neuroreport. 1995;6(5):742–4.
Wunderlich G, Knorr U, Herzog H, Kiwit JC, Freund HJ, Seitz RJ. Precentral glioma location determines the displacement of cortical hand representation. Neurosurgery. 1998;42(1):18–26.
Sanai N, Mirzadeh Z, Berger MS. Functional outcome after language mapping for glioma resection. N Engl J Med. 2008;358(1):18–27.
Davies KG, Maxwell RE, Jennum P, Dhuna A, Beniak TE, Destafney E, et al. Language function following subdural grid-directed temporal lobectomy. Acta Neurol Scand. 1994;90(3):201–6.
FitzGerald DB, Cosgrove GR, Ronner S, Jiang H, Buchbinder BR, Belliveau JW, et al. Location of language in the cortex: a comparison between functional MR imaging and electrocortical stimulation. AJNR Am J Neuroradiol. 1997;18(8):1529–39.
Quinones-Hinojosa A, Ojemann SG, Sanai N, Dillon WP, Berger MS. Preoperative correlation of intraoperative cortical mapping with magnetic resonance imaging landmarks to predict localization of the Broca area. J Neurosurg. 2003;99(2):311–8.
Seghier ML, Lazeyras F, Pegna AJ, Annoni JM, Zimine I, Mayer E, et al. Variability of fMRI activation during a phonological and semantic language task in healthy subjects. Hum Brain Mapp. 2004;23(3):140–55.
Turkeltaub PE, Eden GF, Jones KM, Zeffiro TA. Meta-analysis of the functional neuroanatomy of single-word reading: method and validation. Neuroimage. 2002;16(3 Pt 1):765–80.
Tzourio-Mazoyer N, Josse G, Crivello F, Mazoyer B. Interindividual variability in the hemispheric organization for speech. Neuroimage. 2004;21(1):422–35.
Ranck Jr JB. Which elements are excited in electrical stimulation of mammalian central nervous system: a review. Brain Res. 1975;98(3):417–40.
Haglund MM, Berger MS, Shamseldin M, Lettich E, Ojemann GA. Cortical localization of temporal lobe language sites in patients with gliomas. Neurosurgery. 1994;34(4):567–76.
Taylor MD, Bernstein M. Awake craniotomy with brain mapping as the routine surgical approach to treating patients with supratentorial intraaxial tumors: a prospective trial of 200 cases. J Neurosurg. 1999;90(1):35–41.
Skirboll SS, Ojemann GA, Berger MS, Lettich E, Winn HR. Functional cortex and subcortical white matter located within gliomas. Neurosurgery. 1996;38(4):678–84.
Sartorius CJ, Berger MS. Rapid termination of intraoperative stimulation-evoked seizures with application of cold Ringer's lactate to the cortex. Technical note. J Neurosurg. 1998;88(2):349–51.
Sanai N, Berger MS. Mapping the horizon: techniques to optimize tumor resection before and during surgery. Clin Neurosurg. 2008;55:14–9.
Albert FK, Forsting M, Sartor K, Adams HP, Kunze S. Early postoperative magnetic resonance imaging after resection of malignant glioma: objective evaluation of residual tumor and its influence on regrowth and prognosis. Neurosurgery. 1994;34(1):45–60.
Orringer D, Lau D, Khatri S, Zamora-Berridi GJ, Zhang K, Wu C, et al. Extent of resection in patients with glioblastoma: limiting factors, perception of resectability, and effect on survival. J Neurosurg. 2012;117(5):851–9.
Kennedy JC, Pottier RH. Endogenous protoporphyrin IX, a clinically useful photosensitizer for photodynamic therapy. J Photochem Photobiol B. 1992;14(4):275–92.
el-Sharabasy MM, el-Waseef AM, Hafez MM, Salim SA. Porphyrin metabolism in some malignant diseases. Br J Cancer. 1992;65(3):409–12.
Pottier RH, Chow YF, LaPlante JP, Truscott TG, Kennedy JC, Beiner LA. Noninvasive technique for obtaining fluorescence excitation and emission spectra in vivo. Photochem Photobiol. 1986;44(5):679–87.
Stummer W, Novotny A, Stepp H, Goetz C, Bise K, Reulen HJ. Fluorescence-guided resection of glioblastoma multiforme by using 5-aminolevulinic acid-induced porphyrins: a prospective study in 52 consecutive patients. J Neurosurg. 2000;93(6):1003–13.
Stummer W, Stocker S, Wagner S, Stepp H, Fritsch C, Goetz C, et al. Intraoperative detection of malignant gliomas by 5-aminolevulinic acid-induced porphyrin fluorescence. Neurosurgery. 1998;42(3):518–25.
Lilge L, Olivo MC, Schatz SW, MaGuire JA, Patterson MS, Wilson BC. The sensitivity of normal brain and intracranially implanted VX2 tumour to interstitial photodynamic therapy. Br J Cancer. 1996;73(3):332–43.
Diez Valle R, Slof J, Galvan J, Arza C, Romariz C, Vidal C. Observational, retrospective study of the effectiveness of 5-aminolevulinic acid in malignant glioma surgery in Spain (The VISIONA study). Neurologia. 2013. doi:10.1016/j.nrl.2013.05.004.
Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen HJ. Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol. 2006;7(5):392–401.
Stummer W, Reulen HJ, Meinel T, Pichlmeier U, Schumacher W, Tonn JC, et al. Extent of resection and survival in glioblastoma multiforme: identification of and adjustment for bias. Neurosurgery. 2008;62(3):564–76.
Roberts TP, Zusman E, McDermott M, Barbaro N, Rowley HA. Correlation of functional magnetic source imaging with intraoperative cortical stimulation in neurosurgical patients. J Image Guid Surg. 1995;1(6):339–47.
Schucht P, Beck J, Abu-Isa J, Andereggen L, Murek M, Seidel K, et al. Gross total resection rates in contemporary glioblastoma surgery: results of an institutional protocol combining 5-aminolevulinic acid intraoperative fluorescence imaging and brain mapping. Neurosurgery. 2012;71(5):927–35.
Tsugu A, Ishizaka H, Mizokami Y, Osada T, Baba T, Yoshiyama M, et al. Impact of the combination of 5-aminolevulinic acid-induced fluorescence with intraoperative magnetic resonance imaging-guided surgery for glioma. World Neurosurg. 2011;76(1–2):120–7.
Bogomolny DL, Petrovich NM, Hou BL, Peck KK, Kim MJ, Holodny AI. Functional MRI in the brain tumor patient. Top Magn Reson Imaging. 2004;15(5):325–35.
Guggisberg AG, Honma SM, Findlay AM, Dalal SS, Kirsch HE, Berger MS, et al. Mapping functional connectivity in patients with brain lesions. Ann Neurol. 2008;63(2):193–203.
Hirsch J, Ruge MI, Kim KH, Correa DD, Victor JD, Relkin NR, et al. An integrated functional magnetic resonance imaging procedure for preoperative mapping of cortical areas associated with tactile, motor, language, and visual functions. Neurosurgery. 2000;47(3):711–21.
Meyer PT, Sturz L, Schreckenberger M, Spetzger U, Meyer GF, Setani KS, et al. Preoperative mapping of cortical language areas in adult brain tumour patients using PET and individual non-normalised SPM analyses. Eur J Nucl Med Mol Imaging. 2003;30(7):951–60.
Mueller WM, Yetkin FZ, Hammeke TA, Morris III GL, Swanson SJ, Reichert K, et al. Functional magnetic resonance imaging mapping of the motor cortex in patients with cerebral tumors. Neurosurgery. 1996;39(3):515–20.
Schreckenberger M, Spetzger U, Sabri O, Meyer PT, Zeggel T, Zimny M, et al. Localisation of motor areas in brain tumour patients: a comparison of preoperative [18F]FDG-PET and intraoperative cortical electrostimulation. Eur J Nucl Med. 2001;28(9):1394–403.
Tarapore PE, Martino J, Guggisberg AG, Owen J, Honma SM, Findlay A, et al. Magnetoencephalographic imaging of resting-state functional connectivity predicts postsurgical neurological outcome in brain gliomas. Neurosurgery. 2012;71(5):1012–22.
Vlieger EJ, Majoie CB, Leenstra S, Den Heeten GJ. Functional magnetic resonance imaging for neurosurgical planning in neurooncology. Eur Radiol. 2004;14(7):1143–53.
Black PM, Alexander 3rd E, Martin C, Moriarty T, Nabavi A, Wong TZ, et al. Craniotomy for tumor treatment in an intraoperative magnetic resonance imaging unit. Neurosurgery. 1999;45(3):423–31.
Knauth M, Wirtz CR, Tronnier VM, Aras N, Kunze S, Sartor K. Intraoperative MR imaging increases the extent of tumor resection in patients with high-grade gliomas. AJNR Am J Neuroradiol. 1999;20(9):1642–6.
Kowalik K, Truwit C, Hall W, Kucharczyk J. Initial assessment of costs and benefits of MRI-guided brain tumor resection. Eur Radiol. 2000;10(3):S366–7.
Kubben PL, ter Meulen KJ, Schijns OE, ter Laak-Poort MP, van Overbeeke JJ, van Santbrink H. Intraoperative MRI-guided resection of glioblastoma multiforme: a systematic review. Lancet Oncol. 2011;12(11):1062–70.
Lu J, Wu J, Yao C, Zhuang D, Qiu T, Hu X, et al. Awake language mapping and 3-Tesla intraoperative MRI-guided volumetric resection for gliomas in language areas. J Clin Neurosci. 2013;20(9):1280–7.
Nimsky C, Fujita A, Ganslandt O, Von Keller B, Fahlbusch R. Volumetric assessment of glioma removal by intraoperative high-field magnetic resonance imaging. Neurosurgery. 2004;55(2):358–70.
Nimsky C, Ganslandt O, Tomandl B, Buchfelder M, Fahlbusch R. Low-field magnetic resonance imaging for intraoperative use in neurosurgery: a 5-year experience. Eur Radiol. 2002;12(11):2690–703.
Nimsky C, Ganslandt O, Von Keller B, Romstock J, Fahlbusch R. Intraoperative high-field-strength MR imaging: implementation and experience in 200 patients. Radiology. 2004;233(1):67–78.
Ntoukas V, Krishnan R, Seifert V. The new generation polestar n20 for conventional neurosurgical operating rooms: a preliminary report. Neurosurgery. 2008;62(3 Suppl 1):82–9.
Schneider JP, Schulz T, Schmidt F, Dietrich J, Lieberenz S, Trantakis C, et al. Gross-total surgery of supratentorial low-grade gliomas under intraoperative MR guidance. AJNR Am J Neuroradiol. 2001;22(1):89–98.
Schneider JP, Trantakis C, Rubach M, Schulz T, Dietrich J, Winkler D, et al. Intraoperative MRI to guide the resection of primary supratentorial glioblastoma multiforme–a quantitative radiological analysis. Neuroradiology. 2005;47(7):489–500.
Shaikhouni A, Chiocca EA. Editorial: Intraoperative magnetic resonance spectroscopy and gliomas. J Neurosurg. 2013;118(6):1188–9.
Senft C, Franz K, Ulrich CT, Bink A, Szelenyi A, Gasser T, et al. Low field intraoperative MRI-guided surgery of gliomas: a single center experience. Clin Neurol Neurosurg. 2010;112(3):237–43.
Wirtz CR, Knauth M, Staubert A, Bonsanto MM, Sartor K, Kunze S, et al. Clinical evaluation and follow-up results for intraoperative magnetic resonance imaging in neurosurgery. Neurosurgery. 2000;46(5):1112–20.
Enchev Y, Bozinov O, Miller D, Tirakotai W, Heinze S, Benes L, et al. Image-guided ultrasonography for recurrent cystic gliomas. Acta Neurochir. 2006;148(10):1053–63.
Erdogan N, Tucer B, Mavili E, Menku A, Kurtsoy A. Ultrasound guidance in intracranial tumor resection: correlation with postoperative magnetic resonance findings. Acta Radiol. 2005;46(7):743–9.
Le Roux PD, Berger MS, Wang K, Mack LA, Ojemann GA. Low grade gliomas: comparison of intraoperative ultrasound characteristics with preoperative imaging studies. J Neurooncol. 1992;13(2):189–98.
Serra C, Stauffer A, Actor B, Burkhardt JK, Ulrich NH, Bernays RL, et al. Intraoperative high frequency ultrasound in intracerebral high-grade tumors. Ultraschall Med. 2012;33(7):E306–12.
Tortosa A, Vinolas N, Villa S, Verger E, Gil JM, Brell M, et al. Prognostic implication of clinical, radiologic, and pathologic features in patients with anaplastic gliomas. Cancer. 2003;97(4):1063–71.
Compliance with Ethics Guidelines
Conflict of Interest
Shawn L. Hervey-Jumper and Mitchel S. Berger declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Neuro-oncology
Rights and permissions
About this article
Cite this article
Hervey-Jumper, S.L., Berger, M.S. Role of Surgical Resection in Low- and High-Grade Gliomas. Curr Treat Options Neurol 16, 284 (2014). https://doi.org/10.1007/s11940-014-0284-7
Published:
DOI: https://doi.org/10.1007/s11940-014-0284-7