Opinion statement
Restless Legs Syndrome/Willis-Ekbom Disease (RLS/WED) is a common condition characterized by an irresistible urge to move the legs, concomitant with an unpleasant sensation in the lower limbs, which is typically relieved by movement. Symptoms occur predominantly at rest and prevail in the afternoon or evening. Treatment of patients with RLS/WED is indicated for those patients who suffer from clinically relevant symptoms. The management of mild forms of RLS/WED is mainly based on dopamine agonists (DA) therapy (including pramipexole and ropinirole) and α-2-δ calcium-channel ligand. Nevertheless, with passing of time, symptoms tend to become more severe and the patient can eventually develop pharmacoresistance. Furthermore, long-term treatment with dopaminergic agents may be complicated by the development of augmentation, which is defined by an increase in the severity and frequency of RLS/WED symptoms despite adequate treatment. Here, we discuss which are the best therapeutic options when RLS/WED becomes intractable, with a focus on advantages and side effects of the available medications. Prevention strategies include managing lifestyle changes and a good sleep hygiene. Different drug options are available. Switching to longer-acting dopaminergic agents may be a possibility if the patient is well-tolerating DA treatment. An association with α-2-δ calcium-channel ligand is another first-line approach. In refractory RLS/WED, opioids such as oxycodone–naloxone have demonstrated good efficacy. Other pharmacological approaches include IV iron, benzodiazepines such as clonazepam, and antiepileptic drugs, with different level of evidence of efficacy. Therefore, the final decision regarding the agent to use in treating severe RLS/WED symptoms should be tailored to the patient, taking into account the symptomatology, comorbidities, the availability of treatment and the history of the disease.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, et al. International Restless Legs Syndrome Study Group. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria–history, rationale, description, and significance. Sleep Med. 2014;15:860–73. This paper provides an important description and historical overview that brings to the updated diagnostic criteria for RLS/WED.
Manconi M, Ferri R, Zucconi M, Oldani A, Fantini ML, Castronovo V, et al. First night efficacy of pramipexole in restless legs syndrome and periodic leg movements. Sleep Med. 2007;8:491–7. This study demonstrates the immediate efficacy and tolerability of pramipexole in RLS/WED patients.
Mackie S, Winkelman JW. Long-term treatment of restless legs syndrome (RLS): an approach to management of worsening symptoms, loss of efficacy, and augmentation. CNS Drugs. 2015;29:351–7.
Trenkwalder C, Beneš H, Grote L, García-Borreguero D, Högl B, Hopp M, et al. (2013). Prolonged release oxycodone–naloxone for treatment of severe restless legs syndrome after failure of previous treatment: a double-blind, randomised, placebo-controlled trial with an open-label extension. Lancet Neurol. 2013;12:1141–50. This study provides evidence for the employment of opioids in RLS/WED treatment when first-line drugs have no efficacy.
Tzonova D, Larrosa O, Calvo E, Granizo JJ, Williams AM, De la Llave Y, et al. Breakthrough symptoms during the daytime in patients with restless legs syndrome (Willis-Ekbom disease). Sleep Med. 2012;13:151–5.
García-Borreguero D, Allen R, Kohnen R, et al. Loss of response during long-term treatment of restless legs syndrome: guidelines approved by the International Restless Legs Syndrome Study Group for use in clinical trials. Sleep Med. 2010;11(9):956–7.
Winkelman JW, Johnston L. Augmentation and tolerance with long-term pramipexole treatment of restless legs syndrome (RLS). Sleep Med. 2004;5(1):9–14.
Akpinar S. Treatment of restless legs syndrome with levodopa plus benserazide. Arch Neurol. 1982;39:739.
Garcıa-Borreguero D, Kohnen R, Silber MH, et al. The long-term treatment of restless legs syndrome/Willis-Ekbom disease: evidence-based guidelines and clinical consensus best practice guidance: a report from the International Restless Legs Syndrome Study Group. Sleep Med. 2013;14(7):675–84. These guidelines give an evidenced-based approach for long term-treatment of RLS/WE.
Silber MH, Becker PM, Earley C. Garcia-Borreguero D, Ondo WG, Medical Advisory Board of the Willis-Ekbom Disease Foundation. Willis-Ekbom Disease Foundation revised consensus statement on the management of restless legs syndrome. Mayo Clin Proc. 2013;88(9):977–86.
Lisa Klingelhoefer,A Ilaria Cova,B Sheena GuptaC and Kallol Ray ChaudhuriD, A review of current treatment strategies for restless legs syndrome (Willis–Ekbom disease), Royal College of Physicians 2014
Takahashi M, Ikeda J, Tomida T, Hirata K, Hattori N, Inoue Y. Daytime symptoms of restless legs syndrome—clinical characteristics and rotigotine effectiveness. Sleep Med. 2015;16(7):871–6. doi:10.1016/j.sleep.2015.03.006.
Högl B, Garcia-Borreguero D, Kohnen R, et al. Progressive development of augmentation during long-term treatment with levodopa in restless legs syndrome: results of a prospective multi-center study. J Neurol. 2010;257:230–7.
Tings T, Stiens G, Paulus W, Trenkwalder C, Happe S. Treatment of restless legs syndrome with subcutaneous apomorphine in a patient with short bowel syndrome. J Neurol. 2005;252(3):361–3.
Allen RP, Earley CJ. Augmentation of the restless legs syndrome with carbidopa/ levodopa. Sleep. 1996;19:205–13.
Rinaldi F, Galbiati A, Marelli S, Cusmai M, Gasperi A, Oldani A, Zucconi M, Padovani A, Ferini-Strambi L. Defining the phenotype of Restless Legs Syndrome/Willis-Ekbom Disease (RLS/WED): a clinical and polysomnographic study, J Neurol. 2016
Allen RP, Chen C, Garcia-Borreguero D, Polo O, DuBrava S, Miceli J, et al. Comparison of pregabalin with pramipexole for restless legs syndrome. N Engl J Med. 2014;370(7):621–31.
Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165(11):1286–92. To the best of our knowledge this paper is the first large-scale, multinational, population-based profile study that employs the full standard criteria for RLS/WED.
Trenkwalder C, Benesˇ H, Grote L, et al. Prolonged release oxycodone-naloxone for treatment of severe restless legs syndrome after failure of previous treatment: a double-blind, randomised, placebo-controlled trial with an open-label extension. Lancet Neurol. 2013;12(12):1141–50.
Silver N, Allen RP, Senerth J, Earley CJ. A 10-year, longitudinal assessment of dopamine agonists and methadone in the treatment of restless legs syndrome. Sleep Med. 2011;12(5):440–4.
Ondo WG. Methadone for refractory restless legs syndrome. Mov Disord. 2005;20(3):345–8.
Earley CJ, Connor J, Garcia-Borreguero D, et al. Altered brain iron homeostasis and dopaminergic function in restless legs syndrome (Willis-Ekbom Disease). Sleep Med. 2014;15(11):1288–301.
Hornyak M, Kaube H. Long-term treatment of a patient with severe restless legs syndrome using intrathecal morphine. Neurology. 2012;79(24):2361–2. doi:10.1212/WNL.0b013e318278b5e7. Epub 2012 Nov 28.
Ghosh A, Basu D. Restless legs syndrome in opioid dependent patients. Indian J Psychol Med. 2014;36(1):85–7.
Trenkwalder C, Hening WA, Montagna P, et al. Treatment of restless legs syndrome: an evidence-based review and implications for clinical practice. Mov Disord. 2008;23(16):2267–302.
Walters AS, Wagner ML, Hening WA, et al. Successful treatment of the idiopathic restless legs syndrome in a randomized double-blind trial of oxycodone versus placebo. Sleep. 1993;16(4):327–32.
Wang J, O’Reilly B, Venkataraman R, Mysliwiec V, Mysliwiec A. Efficacy of oral iron in patients with restless legs syndrome and a low-normal ferritin: a randomized, double-blind, placebo-controlled study. Sleep Med. 2009;10(9):973–5.
Ondo W. Intravenous iron dextran for severe refractory restless legs syndrome. Sleep Med. 2010;11:494–6. These are two relevant studies investigating respectively oral and intravenous iron efficacy in RLS/WED syndrome.
Auerbach M, Pappadakis J, Bahrain H, et al. Safety and efficacy of rapidly administered (one hour) one gram of low molecular weight iron dextran (INFeD) for the treatment of iron deficient anemia. Am J Hematol. 2011;86:860–2.
Allen R, Auerbach S, Bahrain H, et al. The prevalence and impact of restless legs syndrome n patients with iron deficiency anemia. Am J Hematol. 2013;88:261–4.
Cho Y, Allen R, Earley C. Lower molecular weight intravenous iron dextran for restless legs syndrome. Sleep Med. 2013;14:274–7.
Schneider J, Krafft A, Manconi M, Hübner A, Baumann C, Werth E, et al. Open-label study of the efficacy and safety of intravenous ferric carboxymaltose in pregnant women with restless legs syndrome. Sleep Med. 2015;16(11):1342–7. doi:10.1016/j.sleep.2015.08.006. Epub 2015 Aug 20.
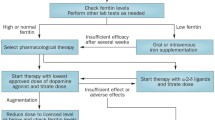
Silber MH, Ehrenberg BL, Allen RP, et al. An algorithm for the management of restless legs syndrome. Mayo Clin Proc. 2004;79(7):916–22.
The International Restless Legs Syndrome Study Group (IRLSSG). White paper summary of recommendations for the prevention and treatment of RLS/WED augmentation, 2015, http://irlssg.org/wp-content/uploads/2015/05/Summary-of-recommendations-RLS-Augmentation-13Aug2015.pdf. These white paper provides new although yet unpublished guidelines for treatment and prevention of augmentation.
Mitler MM, Browman CP, Menn SJ, Gujavarty K, Timms RM. Nocturnal myoclonus: treatment efficacy of clonazepam and temazepam. Sleep. 1986;9(3):385–92.
Schenck CH, Mahowald MW. Long-term, nightly benzodiazepine treatment of injurious parasomnias and other disorders of disrupted nocturnal sleep in 170 adults. Am J Med. 1996;100:333–7.
Della Marca G, Vollono C, Mariotti P, Mazza M, Mennuni GF, Tonali P. Levetiracetam can be effective in the treatment of restless legs syndrome with periodic limb movements in sleep: report of two cases. J Neurol Neurosurg Psychiatry. 2006;77:566–7.
Aukerman MM, Aukerman D, Bayard M, Tudiver F, Thorp L, Bailey B. Exercise and restless legs syndrome: a randomized controlled trial. J Am Board Fam Med. 2006;19:487–93.
Giannaki CD, Sakkas GK, Karatzaferi C, Maridaki MD, Koutedakis Y, Hadjigeorgiou GM, Stefanidis I. Combination of exercise training and dopamine agonists in dialysis patients with RLS: A randomized double-blind placebo controlled study. ASAIO journal (American Society for Artificial Internal Organs: 1992) 2015. This study suggests that exercise training plus low dose DA could represent a valid alternative to high dosage DA in order to reduce symptoms’ severity in RLS/WED.
Hornyak M, Grossmann C, Kohnen R, Schlatterer M, Richter H, Voderholzer U, et al. Cognitive behavioural group therapy to improve patients’ strategies for coping with restless legs syndrome: a proof-of-concept trial. J Neurol Neurosurg Psychiatry. 2008;79:823–5.
Lin YC, Feng Y, Zhan SQ, Li N, Ding Y, Hou Y, et al. Repetitive transcranial magnetic stimulation for the treatment of restless legs syndrome. Chin Med J. 2015;128(13):1728.
Koo YS, Kim SM, Lee C, Lee BU, Moon YJ, Cho YW, et al. Transcranial direct current stimulation on primary sensorimotor area has no effect in patients with drug-naïve restless legs syndrome: a proof-of-concept clinical trial. Sleep Med. 2015;16(2):280–7. This is a well-designed and controlled study that shows the inefficacy of tDCS in reducing RLS/WED symptomatology.
Heide AC, Winkler T, Helms HJ, Nitsche MA, Trenkwalder C, Paulus W, et al. Effects of transcutaneous spinal direct current stimulation in idiopathic restless legs patients. Brain Stimul. 2014;7(5):636–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Fabrizio Rinaldi, Andrea Galbiati, Sara Marelli, Luigi Ferini Strambi and Marco Zucconi each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
About this article
Cite this article
Rinaldi, F., Galbiati, A., Marelli, S. et al. Treatment Options in Intractable Restless Legs Syndrome/Willis-Ekbom Disease (RLS/WED). Curr Treat Options Neurol 18, 7 (2016). https://doi.org/10.1007/s11940-015-0390-1
Published:
DOI: https://doi.org/10.1007/s11940-015-0390-1