Abstract
Background
Greater levels of self-reported pain, pain catastrophizing, and depression have been shown to be associated with persistent pain and functional limitation after surgeries such as TKA. It would be useful for clinicians to be able to measure these factors efficiently.
Questions/purposes
We asked: (1) What is the association of whole-body pain with osteoarthritis (OA)-related knee pain, function, pain catastrophizing, and mental health? (2) What is the sensitivity and specificity for different cutoffs for body pain diagram region categories in relation to pain catastrophizing?
Methods
Patients (n = 267) with knee OA undergoing elective TKA at one academic center and two community orthopaedic centers were enrolled before surgery in a prospective cohort study. Questionnaires included the WOMAC Pain and Function Scales, Pain Catastrophizing Scale (PCS), Mental Health Inventory-5 (MHI-5), and a pain body diagram. The diagram documents pain in 19 anatomic areas. Based on the distribution of the anatomic areas, we established six different body regions. Our analyses excluded the index (surgically treated) knee. Linear regression was used to evaluate the association between the total number of nonindex painful sites on the whole-body pain diagram and measures of OA-related pain and function, mental health, and pain catastrophizing. Generalized linear regression was used to evaluate the association between the number of painful nonindex body regions (categorized as 0; 1–2; or 3–6) with our measures of interest. All models were adjusted for age, sex, and number of comorbid conditions. The cohort included 63% females and the mean age was 66 years (SD, 9 years). With removal of the index knee, the median pain diagram score was 2 (25th, 75th percentiles, 1, 4) with a range of 0 to 15. The median number of painful body regions was 2 (25th, 75th percentiles, 1, 3).
Results
After adjusting for age, sex, and number of comorbid conditions, we found modest associations between painful body region categories and mean scores for WOMAC physical function (r = 0.22, p < 0.001), WOMAC pain (r = 0.20, p = 0.001), MHI-5 (r = −0.31, p < 0.001), and PCS (r = 0.27, p < 0.001). A nonindex body pain region score greater than 0 had 100% (95% CI, 75%–100%) sensitivity for a pain catastrophizing score greater than 30 but a specificity of just 23% (95% CI, 18%–29%) . A score of 3 or greater had greater specificity (73%; 95% CI, 66%–79%) but lower sensitivity (53%; 95% CI, 27%–78%).
Conclusions
We found modest associations between the number of painful sites on a whole-body pain diagram and the number of painful body regions and measures of OA-related pain, function, pain catastrophizing, and mental health. Patients with higher self-reported body pain region scores might benefit from further evaluation for depression and pain catastrophizing.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) of the knee affects more than 9 million adults in the United States [16]. Because there are no effective pharmacologic treatments for stopping or reversing structural progression in patients with OA, management focuses on weight reduction, aerobic exercise, physical therapy, and symptomatic pain relief including corticosteroid injection [8, 19]. Ultimately, as much as 50% of patients with knee OA want a TKA to improve mobility and quality of life [32].
Although most patients who undergo TKA experience substantial pain relief, as much as 20% with OA have persistent pain and functional limitations 6 months after surgery [5, 35, 36]. Studies have shown that pain catastrophizing, greater medical comorbidity, lower educational attainment, depression, fear avoidance, and other psychologic factors are associated with persistent pain and/or enhanced functional limitations after TKA [9, 10, 17, 26, 29, 35]. Pain catastrophizing has been defined as “an exaggerated negative mental set brought to bear during actual or anticipated painful experience” [31]. Prior research on factors associated with persistent OA-related knee pain (lasting more than 6 months) found that pain catastrophizing explained a substantial proportion of variance in measures of pain, psychologic disability, and limitations in walking speed [27, 29, 30]. Similarly, worse mental health (including depression) and greater number of pain problems have been associated with worse THA and TKA outcomes [22, 29, 36]. Given the large number of TKAs performed, poor symptomatic outcomes constitute a prevalent and expensive health problem in the United States [1, 7, 11]. As such, risk factors associated with suboptimal responses to treatment are an area of active investigation.
Body pain diagrams, which have been used for more than 20 years in musculoskeletal pain research, provide a rapid and inexpensive way to measure the extent, distribution, and location of pain [14, 18, 21, 24, 28]. Widespread pain has been recognized as a poor prognostic factor in diseases such as rheumatoid arthritis, cancer, and chronic low back pain, and a poor prognostic factor for outcome of TKA [18, 28].
We investigated whether the pain diagram, which we used to document widespread pain, is associated with established risk factors for persistent symptoms after TKA, including depression, pain severity, and pain catastrophizing. Because widespread pain has been associated with poor outcome in various diseases [4, 12, 13, 24, 28], and because widespread pain is often clinically understood as a sign of psychologic distress [15, 19, 23, 27, 28, 33, 34], we posited that widespread pain, as documented on a pain diagram, would be associated with catastrophizing and depression and poor functional status.
We therefore asked: (1) Are greater numbers of painful body sites, and painful body regions as measured by a widespread body pain diagram, associated with higher levels of catastrophizing and psychologic distress? (2) What are the sensitivity and specificity of different cutoffs for body pain diagram regions in relation to pain catastrophizing?
Patients and Methods
The Study of Total Knee Arthroplasty Responses (STARs) is a prospective cohort study of patients with the primary diagnosis of osteoarthritis of the knee undergoing elective unilateral TKA. STARs was designed to evaluate the prevalence and risk factors for suboptimal outcomes after TKA. Institutional review board approval was obtained for all research sites. We recruited patients at one academic center in New York City (NYU Langone Medical Center) and at two community orthopaedic centers (Orthopaedic Center of the Rockies, Fort Collins, CO, USA, and University of Maryland St. Joseph Medical Center, Towson, MD, USA) between September 2012 and April 2014.
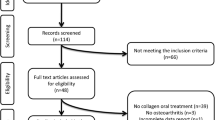
Subjects included English-speaking community-dwelling persons who were at least 40 years old at the time of study entry. At each of the three surgery practices, a local study associate identified all potentially eligible subjects and provided the subject’s contact information to the Brigham and Women’s Hospital research coordinators (KMK, IU). The coordinators contacted all potential subjects to confirm eligibility, explain the study, and determine subject interest in participation. Baseline data collection occurred before surgery. Study participants were reimbursed (USD 25) for returning questionnaires. Of 707 patients referred by the clinical sites for enrollment in the study, 385 agreed to participate and were found to be eligible on phone screening; 267 of these subjects returned questionnaires before surgery and thus were included in these analyses.
The cohort was 63% female with a mean age of 66 years (SD, 9 years). Among the three study enrollment sites, there were no clinically important differences among patients regarding age, sex, or highest level of education.
The baseline questionnaire included a body pain diagram [6] based on the Widespread Pain Index [33, 34], with a list of 19 checkboxes corresponding to anatomic areas throughout the body that study participants were asked to check if they had any current pain at those sites. We delineated six different body regions using the 19 sites on the body pain diagram. These regions included the left upper extremity (left shoulder girdle, left upper arm, and left lower arm), right upper extremity (right shoulder girdle, right upper arm, and right lower arm), left lower extremity (left hip/buttock, left upper leg, and left lower leg), right lower extremity (right hip/buttock, right upper leg, and right lower leg), back or neck (upper back, lower back, and neck), and chest and abdomen. To best capture widespread pain (beyond the index knee), we removed the index knee. The median pain diagram score excluding the index knee was 2 (25th, 75th percentiles, 1, 4) and the range was between 0 and 15. When we aggregate pain sites to regions, the median number of painful body regions, excluding the index knee was 2 (25th, 75th percentiles, 1, 3). The observation that ½ of the subjects reported pain scores of 2 or less reflects the highly right-skewed distributions of the body pain and body region scores. Thus, we grouped subjects in categories based on the number painful body region scores. We found no important differences across body region categories in mean age, median BMI, level of education, health insurance type, or site of study enrollment (Table 1).
Outcome measures included the WOMAC, a widely used questionnaire validated for patients with hip and knee OA that consists of a five-item pain scale, two items for stiffness, and a 17-item functional limitation scale. Subjects responded to each item by checking one of five ordinal Likert responses [2]. We included the WOMAC function and pain scales. In each scale, the responses to questions were summed and scaled from 0 to 100 using a linear transformation with 100 being the worst possible score. We assessed the continuous specification of the WOMAC scales and also categories of scores including 0 to 14, 15 to 39, 40 to 69, and 70 or greater with higher scores indicative of worse OA-related pain or physical function. To assess the degree of pain catastrophizing, including patients’ negative or exaggerated attitudes toward pain, we used the 13-item Pain Catastrophizing Scale (PCS) [30]. In addition to the continuous specification, we used a cutoff of 30 or greater as representing a high degree of pain catastrophizing [15, 23, 30]. The five-item Mental Health Index-5 (MHI-5) [3, 25] was used as a measure of anxiety and depressive feelings. The questions are summed and scaled from 0 to 100 using a linear transformation. We examined the score as a continuous variable and as a dichotomous variable with lower scores (< 68) indicative of worse mental health [3, 25].
Subjects also answered questions regarding their demographic characteristics, their expectations of having a completely successful surgery, and of having a surgical complication (infection of the knee prosthesis, nerve damage, or dislocation of the knee prosthesis), and medical complication (including pneumonia, blood clot, or heart attack). Patients rated the likelihood of these events occurring as 0% to 10%, 11% to 25%, 26% to 50%, 51% to 75%, or 76% to 100%. Subjects also completed items documenting use of medications, assistive devices, and appointments with healthcare providers during the prior 3 months.
Statistical Analysis
We included only baseline data for this analysis. Descriptive statistics either were summarized as means (± SD) or medians (25th and 75th percentiles) for continuous variables, depending on normality, and as percentages for categorical variables. Differences between proportions were assessed by the chi-square test or Fisher’s exact test and continuous variables were compared by Student’s t-tests or Wilcoxon nonparametric tests. Furthermore, the test for trend was assessed using the Jonckheere-Terpstra test for continuous variables and the Cochran-Mantel-Haenszel test of trend for categorical variables. Linear regression was used to evaluate the correlations between body pain scores and continuous measures of OA-related pain and function, mental health, and pain catastrophizing. Furthermore, generalized linear models adjusting for age, sex, and number of comorbid conditions were run to assess the association between body region categories and OA-related pain and function and mental health scores. The model output included adjusted mean values (± standard error [SE]) and pairwise comparisons for the three body pain regions. Pearson correlation analysis was used to examine the associations between the categories of pain-region score and the continuous versions of the WOMAC pain and function scales, MHI-5, and pain catastrophizing.
We evaluated sensitivity and specificity of the nonindex body region pain score in relation to the PCS using a value of 30 as the threshold for high catastrophizing [29]. For these calculations, we categorized the number of painful body regions as either 0 to 2 versus 3 or greater or as 0 versus 1 or greater (Table 2). The second categorization was chosen to investigate any nonindex pain versus none. Contingency tables were used to calculate the sensitivity and specificity and positive and negative predictive values of the body pain categories and accepted cutoffs for the PCS. A PCS score of 30 or greater, recognized as a high catastrophizing score [27, 29] served as the gold standard in these analyses. We used two different cutoffs (0 vs ≥ 1; 1–2 vs ≥ 3) of the body pain category scores to examine tradeoffs between sensitivity and specificity.
All statistical analyses were performed using SAS® software, Version 9.4 (Cary, NC, USA), and a two-sided p value of 0.05 or less was considered to indicate statistical significance.
Results
Overall, we found modest associations between the continuous measure of body region scores and number of painful body sites and worse scores on continuous measures of the MHI-5 score (regions, r = −0.24; sites, r = −0.31), PCS score (regions, r = 0.24; sites, r = 0.27), WOMAC physical function (regions, r = 0.25; sites, r = 0.22), and WOMAC pain (regions, r = 0.20; sites, r = 0.20) (p ≤ 0.001 for all comparisons). Subjects with a greater number of painful body regions were more likely than those were fewer painful body regions to be grouped in the highest PCS score category (≥ 30), indicating more catastrophizing (p = 0.03). MHI-5 scores less than 68 also were more common in the subjects with the greatest number of painful body regions (p = 0.005), as were worse scores on the WOMAC pain and function scales (Table 3). When adjusted for sex, age, and number of medical comorbidities, we observed associations between increasing number of painful body region categories and increasing mean scores for WOMAC physical function, WOMAC pain, and PCS, and decreasing mean scores with the MHI-5 (Table 4). For WOMAC physical function, the adjusted mean (SE) score for participants reporting no body pain, low (1–2 regions) and high (≥ 3 regions) were 43 (3), 48 (2), and 53 (3), respectively. Similarly, for WOMAC pain and the three ordered pain-region categories, the adjusted means (SE) were 40 (3), 43 (2), and 49 (3), and for pain catastrophizing, the adjusted means (SE) were 9 (2), 12 (2), and 16 (2). The adjusted mean MHI-5 scores decreased with each increase in number of painful body region category. The mean (SE) adjusted MHI-5 scores were 68 (4) for participants reporting no pain beyond the index joint, 66 (3) for the low category, and 58 (3) for participants with three or more painful body regions.
The sensitivity and specificity analysis for pain catastrophizing and nonindex body region pain revealed that a nonindex body region pain score of 1 or more had 100% (95% CI, 75%–100%) sensitivity for a pain catastrophizing score greater than 30 but a specificity of just 23% (95% CI, 18%–29%). Furthermore, the positive predictive value was 9% (95% CI, 5%–14%) and negative predictive value was 100% (95% CI, 91%–100%). A nonindex body pain region score of 3 or more had greater specificity for a catastrophizing score greater than 30 (73%; 95% CI, 66%–79%) but lower sensitivity (53%; 95% CI, 27%–78%), with a positive predictive value of 12% (95% CI, 6%–24%) and a negative predictive value of 96% (95% CI, 91%–98%).
Discussion
Pain diagrams have been associated with poor outcomes for numerous disorders [4, 13, 15, 24, 28]. Widespread pain, which can be documented with pain diagrams, has been associated with psychologic distress [24, 28, 33, 34]. These observations suggest that a body pain diagram might be associated with psychologic distress including catastrophizing and depression. Our objective was to determine whether a body pain diagram was associated with measures of pain catastrophizing, depression, and functional status in patients with advanced OA before TKA at three centers.
Limitations of our study include that the body regions delineated on our pain diagram do not correspond directly to joints, which might result in underreporting of joint pain. In addition, in some studies patients were allowed to record out-of-body or external sites of pain on pain diagrams [20]. We could not examine this phenomenon because our diagram did not permit subjects to record out-of-body painful sites.
In a cohort of preoperative patients with knee OA at three orthopaedic centers, we found that more widespread pain as noted by either a greater number of painful body sites or painful body regions documented on a body pain diagram was associated with greater preoperative levels of pain catastrophizing, worse mental health, greater pain scores, and reduced physical function. These modest associations persisted when adjusted for sex, age, and number of medical comorbidities. Several psychologic factors, including anxiety or depression and catastrophizing, are associated with worse outcomes of surgical procedures including TKA [15, 17, 23, 26, 31, 32]. Thus, the association we documented between painful body regions as determined using a body pain diagram and the MHI-5 and PCS scores suggests that the pain diagram may be useful in identifying patients at risk for a poor surgical outcome. This hypothesis will be tested in future work. Future studies also should examine whether the associations documented here between body pain diagram and measures of catastrophizing, depression, pain, and function are mediated by other musculoskeletal conditions, psychologic conditions, or other factors.
The 100% sensitivity of a diagram score of 1 or greater indicates that a normal pain diagram (excluding index joint) will be useful for ruling out catastrophizing. Similarly, for both body region categorizations, a high negative predictive value (96% and 100%, respectively) was reported, indicating that subjects with a low number of painful body regions (0–2) may be expected by the clinician to have low pain catastrophizing.
We found associations between more widespread pain as indicated by a higher number of painful body regions shown on a body pain diagram and measures of pain catastrophizing, mental health, and OA-related pain and function. While patients with 0 to 2 painful body regions had a 96% negative predictive value for pain catastrophizing, patients with higher self-reported pain might benefit from additional evaluation for depression and pain catastrophizing. By limiting evaluation for psychologic predictors of TKA outcome to a smaller subset of preoperative candidates, we anticipate fewer burdens for orthopaedic surgeons and patients. These analyses are cross-sectional; future research should investigate whether the degree of generalized pain as assessed from a body pain diagram is associated with poor surgical outcome.
References
Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project: Nationwide Inpatient Sample. 2011. Available at: http://hcupnet.ahrq.gov. Accessed October 6, 2014.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840.
Berwick DM, Murphy JM, Goldman PA, Ware JE Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29:169–176.
Bessette L, Keller RB, Lew RA, Simmons BP, Fossel AH, Mooney N, Katz JN. Prognostic value of a hand symptom diagram in surgery for carpal tunnel syndrome. J Rheumatol. 1997;24:726–734.
Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open. 2012;2:e000435.
Centro Internacional de Medicina Avanzada – Servicio de Reumatología IfdR. Nuevos criterios preliminares para el diagnóstico clínico de la fibromialgia: indice de dolor generalizado – Widespread Pain Index (WPI). Available at: http://www.institutferran.org/documentos/WPI+SS-PACIENTES.pdf. Accessed April 4, 2011.
Culler SD, Jevsevar DS, Shea KG, Wright KK, Simon AW. The incremental hospital cost and length-of-stay associated with treating adverse events among Medicare beneficiaries undergoing TKA. J Arthroplasty. 2015;30:19–25.
Dowsey MM, Gunn J, Choong PF. Selecting those to refer for joint replacement: who will likely benefit and who will not? Best Pract Res Clin Rheumatol. 2014;28:157–171.
Edwards RR, Haythornthwaite JA, Smith MT, Klick B, Katz JN. Catastrophizing and depressive symptoms as prospective predictors of outcomes following total knee replacement. Pain Res Manag. 2009;14:307–311.
Judge A, Arden NK, Cooper C, Kassim Javaid M, Carr AJ, Field RE, Dieppe PA. Predictors of outcomes of total knee replacement surgery. Rheumatology (Oxford). 2012;51:1804–1813.
Katz JN. Editorial: appropriateness of total knee arthroplasty. Arthritis Rheumatol. 2014;66:1979–1981.
Katz JN, Simmons BP. Clinical practice: carpal tunnel syndrome. N Engl J Med. 2002;346:1807–1812.
Katz JN, Stirrat CR, Larson MG, Fossel AH, Eaton HM, Liang MH. A self-administered hand symptom diagram for the diagnosis and epidemiologic study of carpal tunnel syndrome. J Rheumatol. 1990;17:1495–1498.
Khanna V, Caragianis A, Diprimio G, Rakhra K, Beaule PE. Incidence of hip pain in a prospective cohort of asymptomatic volunteers: is the cam deformity a risk factor for hip pain? Am J Sports Med. 2014;42:793–797.
Kleiman V, Clarke H, Katz J. Sensitivity to pain traumatization: a higher-order factor underlying pain-related anxiety, pain catastrophizing and anxiety sensitivity among patients scheduled for major surgery. Pain Res Manag. 2011;16:169–177.
Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis Rheum. 2008;58:26–35.
Lewis GN, Rice DA, McNair PJ, Kluger M. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth. 2015;114:551–561.
Margolis RB, Tait RC, Krause SJ. A rating system for use with patient pain drawings. Pain. 1986;24:57–65.
McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, Hawker GA, Henrotin Y, Hunter DJ, Kawaguchi H, Kwoh K, Lohmander S, Rannou F, Roos EM, Underwood M. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:363–388.
Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1:277–299.
Post WR, Fulkerson J. Knee pain diagrams: correlation with physical examination findings in patients with anterior knee pain. Arthroscopy. 1994;10:618–623.
Riddle DL, Jiranek WA, Hayes CW. Use of a validated algorithm to judge the appropriateness of total knee arthroplasty in the United States: a multicenter longitudinal cohort study. Arthritis Rheumatol. 2014;66:2134–2143.
Riddle DL, Wade JB, Jiranek WA, Kong X. Preoperative pain catastrophizing predicts pain outcome after knee arthroplasty. Clin Orthop Relat Res. 2010;468:798–806.
Rombaut L, Scheper M, De Wandele I, De Vries J, Meeus M, Malfait F, Engelbert R, Calders P. Chronic pain in patients with the hypermobility type of Ehlers-Danlos syndrome: evidence for generalized hyperalgesia. Clin Rheumatol. 2014.
Rumpf HJ, Meyer C, Hapke U, John U. Screening for mental health: validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Res. 2001;105:243–253.
Singh JA, Lewallen DG. Depression in primary TKA and higher medical comorbidities in revision TKA are associated with suboptimal subjective improvement in knee function. BMC Musculoskelet Disord. 2014;15:127.
Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Waters SJ, Riordan PA, Blumenthal JA, McKee DC, LaCaille L, Tucker JM, Schmitt D, Caldwell DS, Kraus VB, Sims EL, Shelby RA, Rice JR. Pain catastrophizing and pain-related fear in osteoarthritis patients: relationships to pain and disability. J Pain Symptom Manage. 2009;37:863–872.
Southerst D, Cote P, Stupar M, Stern P, Mior S. The reliability of body pain diagrams in the quantitative measurement of pain distribution and location in patients with musculoskeletal pain: a systematic review. J Manipulative Physiol Ther. 2013;36:450–459.
Sullivan M, Tanzer M, Stanish W, Fallaha M, Keefe FJ, Simmonds M, Dunbar M. Psychological determinants of problematic outcomes following total knee arthroplasty. Pain. 2009;143:123–129.
Sullivan MJ, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–532.
Walker BF, Losco CD, Armson A, Meyer A, Stomski NJ. The association between pain diagram area, fear-avoidance beliefs, and pain catastrophising. Chiropr Man Therap. 2014;22:5.
Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, Wright J, Katz JN, Losina E. Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am. 2013;95:385–392.
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol. 2011;38:1113–1122.
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MB. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010;62:600–610.
Wylde V, Dieppe P, Hewlett S, Learmonth ID. Total knee replacement: is it really an effective procedure for all? Knee. 2007;14:417–423.
Wylde V, Hewlett S, Learmonth ID, Dieppe P. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566–572.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by NIAMS grants T32 AR055885 (AJD) and K24AR057827 (EL) One of the authors (AJD) was supported by a National Institutes of Health T32 grant (AR055885) outside the submitted work. One of the authors (DFD) has received personal fees and nonfinancial support from DePuy Orthopaedics (Warsaw, IN, USA) outside the submitted work. One of the authors (KK) has received personal fees from DePuy Orthopaedics outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study was done at the Orthopaedic and Arthritis Center for Outcomes Research, Department of Orthopedic Surgery, Brigham and Women’s Hospital, Boston, MA, USA.
About this article
Cite this article
Dave, A.J., Selzer, F., Losina, E. et al. Is There an Association Between Whole-body Pain With Osteoarthritis-related Knee Pain, Pain Catastrophizing, and Mental Health?. Clin Orthop Relat Res 473, 3894–3902 (2015). https://doi.org/10.1007/s11999-015-4575-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4575-4