Abstract
Background
Severe headache is a hallmark clinical feature of spontaneous subarachnoid hemorrhage (SAH), affecting nearly 90% of patients during index hospitalization, regardless of the SAH severity or presence of a culprit aneurysm. Up to 1 in 4 survivors of SAH experience chronic headaches, which may be severe and last for years. Data guiding the optimal management of post-SAH headache are lacking. Opioids, often in escalating doses, remain the guideline-recommended mainstay of acute therapy, but pain relief remains suboptimal.
Methods
This study is a case series of adult patients who received bilateral pterygopalatine fossa (PPF) blockade for the management of refractory headaches after spontaneous SAH (aneurysmal and non-aneurysmal) at a single tertiary care center. We examined pain scores and analgesic requirements before and after block placement.
Results
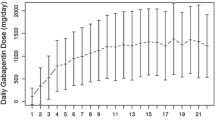
Seven patients (median age 54 years, 3 men, four aneurysmal and three non-aneurysmal) received a PPF-block between post-bleed day 6–11 during index hospitalization in the neurointensive care unit. The worst pain recorded in the 24-h period before the block was significantly higher than in the period 4 h after the block (9.1 vs. 3.1; p = 0.0156), and in the period 8 h after the block (9.1 vs. 2.8; p = 0.0313). The only complication was minor oozing from the needle insertion sites, which subsided completely with gauze pressure within 1 min.
Conclusions
PPF blockade might constitute a promising opioid-sparing therapeutic strategy for the management of post-SAH headache that merits further prospective controlled randomized studies.



Similar content being viewed by others
References
Zacharia BE, Hickman ZL, Grobelny BT, et al. Epidemiology of aneurysmal subarachnoid hemorrhage. Neurosurg Clin North Am. 2010;21:221–33.
Morad AH, Tamargo RJ, Gottschalk A. The longitudinal course of pain and analgesic therapy following aneurysmal subarachnoid hemorrhage: a cohort study. Headache. 2016;56:1617–25.
Glisic EK, Gardiner L, Josti L, et al. Inadequacy of headache management after subarachnoid hemorrhage. Am J Crit Care. 2016;25:136–43.
Magalhaes JE, Azevedo-Filho HR, Rocha-Filho PA. The risk of headache attributed to surgical treatment of intracranial aneurysms: a cohort study. Headache. 2013;53:1613–23.
Canhao P, Ferro JM, Pinto AN, Melo TP, Campos JG. Perimesencephalic and nonperimesencephalic subarachnoid haemorrhages with negative angiograms. Acta Neurochir (Wien). 1995;132:14–9.
Huckhagel T, Klinger R, Schmidt NO, Regelsberger J, Westphal M, Czorlich P. The burden of headache following aneurysmal subarachnoid hemorrhage: a prospective single-center cross-sectional analysis. Acta Neurochir (Wien). 2020;162:893–903.
Gerner ST, Reichl J, Custal C, et al. Long-term complications and influence on outcome in patients surviving spontaneous subarachnoid hemorrhage. Cerebrovasc Dis. 2020;49:307–15.
Steiner T, Juvela S, Unterberg A, et al. European stroke organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 2013;35:93–112.
Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263–306.
Martyn JAJ, Mao J, Bittner EA. Opioid tolerance in critical illness. N Engl J Med. 2019;380:365–78.
Chen EY, Marcantonio A, Tornetta P 3rd. Correlation between 24-hour predischarge opioid use and amount of opioids prescribed at hospital discharge. JAMA Surg. 2018;153:e174859.
Terakado T, Nakai Y, Ikeda G, et al. Effectiveness of low-dose intravenous fentanyl for postoperative headache management after neck clipping of ruptured intracranial aneurysms. World Neurosurg. 2020;134:e339–45.
Iwanaga J, Wilson C, Simonds E, et al. Clinical anatomy of blockade of the pterygopalatine ganglion: literature review and pictorial tour using cadaveric images. Kurume Med J. 2018;65:1–5.
Chiono J, Raux O, Bringuier S, et al. Bilateral suprazygomatic maxillary nerve block for cleft palate repair in children: a prospective, randomized, double-blind study versus placebo. Anesthesiology. 2014;120:1362–9.
Binfalah M, Alghawi E, Shosha E, Alhilly A, Bakhiet M. Sphenopalatine ganglion block for the treatment of acute migraine headache. Pain Res Treat. 2018;2018:2516953.
Cady RK, Saper J, Dexter K, Cady RJ, Manley HR. Long-term efficacy of a double-blind, placebo-controlled, randomized study for repetitive sphenopalatine blockade with bupivacaine vs. saline with the Tx360 device for treatment of chronic migraine. Headache. 2015;55:529–42.
Ho KWD, Przkora R, Kumar S. Sphenopalatine ganglion: block, radiofrequency ablation and neurostimulation—a systematic review. J Headache Pain. 2017;18:118.
Nair AS, Rayani BK. Sphenopalatine ganglion block for relieving postdural puncture headache: technique and mechanism of action of block with a narrative review of efficacy. Korean J Pain. 2017;30:93–7.
Frontera JA, Fernandez A, Schmidt JM, et al. Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke. 2009;40:1963–8.
Boezaart APS, Smith CR, Reyneke JP. Pterygopalatine ganglion block: for effective treatment of migraine, cluster headache, postdural puncture headache and postoperative pain. Gainesville: LLC Publications; 2018.
Samagh N, Bhagat H, Jangra K. Monitoring cerebral vasospasm: how much can we rely on transcranial Doppler. J Anaesthesiol Clin Pharmacol. 2019;35:12–8.
Kwon OK. Headache and aneurysm. Neuroimaging Clin North Am. 2019;29:255–60.
May A, Buchel C, Turner R, Goadsby PJ. Magnetic resonance angiography in facial and other pain: neurovascular mechanisms of trigeminal sensation. J Cereb Blood Flow Metab. 2001;21:1171–6.
Drug Overdose Death Data. (2018). Accessed Feb 1, 2019.
Schaffer JT, Hunter BR, Ball KM, Weaver CS. Noninvasive sphenopalatine ganglion block for acute headache in the emergency department: a randomized placebo-controlled trial. Ann Emerg Med. 2015;65:503–10.
Mehta D, Leary MC, Yacoub HA, et al. The effect of regional anesthetic sphenopalatine ganglion block on self-reported pain in patients with status migrainosus. Headache. 2019;59:69–76.
Melinosky CMD. Sphenopalatine ganglion blockade as a novel treatment for aneurysmal subarachnoid hemorrhage associated intractable headache. In: 17th annual meeting neurocritical care society. Vancouver: Springer; 2019, p. S258.
Marston AP, Merritt G, Morris JM, Cofer SA. Impact of age on the anatomy of the pediatric pterygopalatine fossa and its relationship to the suprazygomatic maxillary nerve block. Int J Pediatr Otorhinolaryngol. 2018;105:85–9.
Piagkou M, Demesticha T, Troupis T, et al. The pterygopalatine ganglion and its role in various pain syndromes: from anatomy to clinical practice. Pain Pract. 2012;12:399–412.
Piagkou MN, Skandalakis P, Piagkos G, Demesticha T. Trigeminal pain and its distribution in different trigeminal nerve branches. Anesth Pain Med. 2012;1:271–2.
Takahashi M, Zhang ZD, Macdonald RL. Sphenopalatine ganglion stimulation for vasospasm after experimental subarachnoid hemorrhage. J Neurosurg. 2011;114:1104–9.
Bornstein NM, Saver JL, Diener HC, et al. Sphenopalatine ganglion stimulation to augment cerebral blood flow. Stroke 2019:STROKEAHA118024582.
Althaus A, Arranz Becker O, Moser KH, et al. Postoperative pain trajectories and pain chronification-an empirical typology of pain patients. Pain Med. 2018;19:2536–45.
Dhakal LP, Hodge DO, Nagel J, et al. Safety and tolerability of gabapentin for aneurysmal subarachnoid hemorrhage (sah) headache and meningismus. Neurocrit Care. 2015;22:414–21.
Lionel KR, Sethuraman M, Abraham M, Vimala S, Prathapadas U, Hrishi AP. Effect of pregabalin on perioperative headache in patients with aneurysmal subarachnoid hemorrhage: a randomized double-blind placebo-controlled trial. J Neurosci Rural Pract. 2019;10:438–43.
Dhakal LP, Turnbull MT, Jackson DA, et al. Safety, tolerability, and efficacy of pain reduction by gabapentin for acute headache and meningismus after aneurysmal subarachnoid hemorrhage: a pilot study. Front Neurol. 2020;11:744.
Acknowledgments
Dr. Carolina B. Maciel has received the Claude D. Pepper Older Americans Independence Center Junior Scholar award that supports preclinical studies of mechanisms of secondary brain injury in a rodent cardiac arrest model. Gerard Garvan produced the graphs using R software.
Author information
Authors and Affiliations
Contributions
Cameron R. Smith and Katharina M. Busl: Conception and design of the study, data interpretation, drafting of the article, critical revision of the article, final approval of the version to be published. Cynthia Garvan: Data analysis and interpretation, critical revision of the article. W. Christopher Fox and Carolina Maciel: conception of the study, data interpretation, critical revision of the article. Marc-Alain Babi, Michael A. Pizzi, Christopher P. Robinson: data interpretation, critical revision of the article. Erica Lobmeyer, Alberto Bursian: data collection, data interpretation, critical revision of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical Approval
This study adheres to ethical guidelines and has approval from the local Institutional Review Board (IRB 201901207) including waiver of consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Smith, C.R., Fox, W.C., Robinson, C.P. et al. Pterygopalatine Fossa Blockade as Novel, Narcotic-Sparing Treatment for Headache in Patients with Spontaneous Subarachnoid Hemorrhage. Neurocrit Care 35, 241–248 (2021). https://doi.org/10.1007/s12028-020-01157-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01157-1