Abstract
Background
Surgical resection plays an integral part in the curative treatment of esophageal (EC) and gastric cancer (GC). The impact of the allocation of surgeons at the county level on these cancer outcomes is unclear. Our aims were to examine the effect of surgeon density on EC and GC mortality and to compare the relative roles of thoracic and general surgeons on outcomes.
Methods
Using county-level data from the Area Resource File, we constructed multivariate regression models to explore the effect of thoracic and general surgeon density on EC and GC mortality, adjusting for cancer incidence rate, county-level, socioeconomic factors and health care resource metrics.
Results
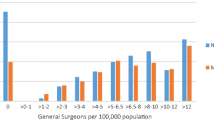
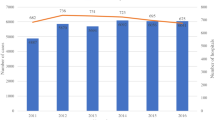
In total, 663 and 539 counties were analyzed for EC and GC, respectively: Mean EC and GC mortality rates were 4.95 and 4.07; mean thoracic and general surgeon density were 6 and 50 per 100,000 people, respectively. When compared to counties with no thoracic surgeons, those with at least one thoracic surgeon had reduced EC mortality. For GC, counties with one or more general surgeons also had decreased deaths when compared with those without any general surgeons. While increasing the density of surgeons beyond ten only yielded minimal improvements in EC mortality, this resulted in significant further reductions in GC mortality.
Conclusions
Mortality from GC appears to be more susceptible to the benefits of increased surgeon density. For EC, a strategic policy of allocating health resources and distributing the surgical workforce proportionally across counties will be best able to optimize outcomes at the population-based level.


Similar content being viewed by others
References
US Census Bureau. Population projections. Available at: http://www.census.gov/population/www/projection/index.html.
Cooper RA. The future of specialty care in the US. Nat Clin Pract Rheumatol. 2008;4:333.
Cooper RA. The coming era of too few physicians. Bull Am Coll Surg. 2008;93:11–8.
Starfield B, Shi L, Grover A, Macinko J. The effects of specialist supply on populations’ health: assessing the evidence. Health Aff Millwood. 2005;Suppl Web Exclusives:W5-97-W5-107.
Chang RK, Halfon N. Geographic distribution of pediatricians in the United States: an analysis of the fifty states and Washington, DC. Pediatrics. 1997;100:172–9.
Rasell ME. Cost sharing in health insurance—a reexamination. N Engl J Med. 1995;332:1164–8.
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–27.
Cooper RA. States with more physicians have better-quality health care. Health Aff Millwood. 2009;28:w91–102.
Van Durme DJ, Ullman R, Campbell RJ, Roetzheim R. Effects of physician supply on melanoma incidence and mortality in Florida. South Med J. 2003;96:656–60.
Fleisher JM, Lou JQ, Farrell M. Relationship between physician supply and breast cancer survival: a geographic approach. J Community Health. 2008;33:179–82.
Gorey KM, Luginaah IN, Fung KY, Bartfay E, Hamm C, Wright FC, et al. Physician supply and breast cancer survival. J Am Board Fam Med. 2010;23:104–8.
Wright CD, Kucharczuk JC, O’Brien SM, Grab JD, Allen MS, Society of Thoracic Surgeons General Thoracic Surgery Database. Predictors of major morbidity and mortality after esophagectomy for esophageal cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database risk adjustment model. J Thorac Cardiovasc Surg. 2009;137:587–95. discussion 596.
National Cancer Institute, US Centers for Disease Control and Prevention. State cancer profiles. Available at: http://statecancerprofiles.cancer.gov. 2013.
US Department of Health and Human Services, Health Resources and Services Administration: Area Resource File ARF. National county-level health resource information database. Available at: http://www.arfsys.com.
US Department of Agriculture, Economic Research Service. Rural–urban continuum codes.
Hollenbeck BK, Wei Y, Birkmeyer JD. Volume, process of care, and operative mortality for cystectomy for bladder cancer. Urology. 2007;69:871–5.
Porter GA, Soskolne CL, Yakimets WW, Newman SC. Surgeon-related factors and outcome in rectal cancer. Ann Surg. 1998;227:157–67.
Martling A, Cedermark B, Johansson H, Rutqvist LE, Holm T. The surgeon as a prognostic factor after the introduction of total mesorectal excision in the treatment of rectal cancer. Br J Surg. 2002;89:1008–13.
Smith JA, King PM, Lane RH, Thompson MR. Evidence of the effect of ‘specialization’ on the management, surgical outcome and survival from colorectal cancer in Wessex. Br J Surg. 2003;90:583–92.
McArdle CS, Hole DJ. Influence of volume and specialization on survival following surgery for colorectal cancer. Br J Surg. 2004;9:610–7.
Bilimoria KY, Phillips JD, Rock CE, Hayman A, Prystowsky JB, Bentrem DJ. Effect of surgeon training, specialization, and experience on outcomes for cancer surgery: a systematic review of the literature. Ann Surg Oncol. 2009;16:1799–808.
Borowski DW, Kelly SB, Bradburn DM, Wilson RG, Gunn A, Ratcliffe AA, et al. Impact of surgeon volume and specialization on short-term outcomes in colorectal cancer surgery. Br J Surg. 2007;94:880–9.
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37.
Wibe A, Eriksen MT, Syse A, Tretli S, Myrvold HE, Soreide O, et al. Effect of hospital caseload on long-term outcome after standardization of rectal cancer surgery at a national level. Br J Surg. 2005;92:217–24.
Rabeneck L, Davila JA, Thompson M, El-Serag HB. Surgical volume and long-term survival following surgery for colorectal cancer in the Veterans Affairs Health-Care System. Am J Gastroenterol. 2004;99:668–75.
Birkmeyer JD, Sun Y, Wong SL, Stukel TA. Hospital volume and late survival after cancer surgery. Ann Surg. 2007;245:777–83.
van Gijn W, Gooiker GA, Wouters MW, Post PN, Tollenaar RA, van de Velde CJ. Volume and outcome in colorectal cancer surgery. Eur J Surg Oncol. 2010;36 Suppl 1:S55–63.
Krakauer H, Jacoby I, Millman M, Lukomnik JE. Physician impact on hospital admission and on mortality rates in the Medicare population. Health Serv Res. 1996;31:191–211.
Goodman DC, Fisher ES, Little GA, Stukel TA, Chang CH, Schoendorf KS. The relation between the availability of neonatal intensive care and neonatal mortality. N Engl J Med. 2002;346:1538–44.
Odisho AY, Cooperberg MR, Fradet V, Ahmad AE, Carroll PR. Urologist density and county-level urologic cancer mortality. J Clin Oncol. 2010;28:2499–504.
Lee W, Nelson R, Mailey B, Duldulao MP, Garcia-Aguilar J, Kim J. Socioeconomic factors impact colon cancer outcomes in diverse patient populations. J Gastrointest Surg. 2012;16:692–704.
Aarts MJ, Lemmens VE, Louwman MW, Kunst AE, Coebergh JW. Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer. 2010;46:2681–95.
Ferrer RL. Pursuing equity: contact with primary care and specialist clinicians by demographics, insurance, and health status. Ann Fam Med. 2007;5:492–502.
Acknowledgments
The authors would like to acknowledge the Canadian Cancer Society Research Institute and the British Columbia Cancer Foundation for their support.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ho, M.Y., Al-barrak, J., Peixoto, R.D. et al. The Association Between County-Level Surgeon Density and Esophageal and Gastric Cancer Mortality. J Gastrointest Canc 45, 487–493 (2014). https://doi.org/10.1007/s12029-014-9661-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-014-9661-4