Abstract
Introduction
To compare the impact of non-mechanical excimer-assisted (EXCIMER) and femtosecond laser-assisted (FEMTO) trephination on outcomes after penetrating keratoplasty (PK).
Methods
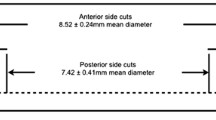
In this retrospective study, 68 eyes from 23 females and 45 males (mean age at time of surgery, 53.3 ± 19.8 years) were included. Inclusion criteria were one surgeon (BS), primary central PK, Fuchs’ dystrophy (FUCHS) or keratoconus (KC), no previous intraocular surgery, graft oversize 0.1 mm and 16-bite double running suture. Trephination was performed using a manually guided 193-nm Zeiss Meditec MEL70 excimer laser (EXCIMER group: 18 FUCHS, 17 KC) or 60-kHz IntraLase™ femtosecond laser (FEMTO group: 16 FUCHS, 17 KC). Subjective refractometry (trial glasses) and corneal topography analysis (Pentacam HR; Casia SS-1000 AS-OCT; TMS-5) were performed preoperatively, before removal of the first suture (11.4 ± 1.9 months) and after removal of the second suture (22.6 ± 3.8 months).
Results
Before suture removal, mean refractive/AS-OCT topographic astigmatism did not differ significantly between EXCIMER and FEMTO. After suture removal, mean refractive/Pentacam/AS-OCT topographic astigmatism was significantly higher in the FEMTO (6.2 ± 2.9 D/7.1 ± 3.2 D/7.4 ± 3.3 D) than in the EXCIMER patients (4.3 ± 3.0 D/4.4 ± 3.1 D/4.0 ± 2.9 D) (p ≤ 0.005). Mean corrected distance visual acuity increased from 0.22 and 0.23 preoperatively to 0.55 and 0.53 before or 0.7 and 0.6 after suture removal in the EXCIMER and FEMTO groups, respectively. Differences between EXCIMER and FEMTO were only pronounced in the KC subgroup.
Conclusion
Non-mechanical EXCIMER trephination seems to have advantages regarding postoperative corneal astigmatism and visual acuity compared with FEMTO trephination, especially in KC. A bigger sample size and longer follow-up are needed to evaluate the long-term impact of EXCIMER and FEMTO trephination on postoperative topographic and visual outcomes.
Similar content being viewed by others
References
Wang J, Hasenfus A, Schirra F, Bohle RM, Szentmáry N. Changing indications for penetrating keratoplasty in Homburg/Saar from 2001 to 2010—histopathology of 1200 corneal buttons. Graefes Arch Clin Exp Ophthalmol. 2013;251(3):797–802.
Seitz B, Hager T, Langenbucher A, Naumann GOH. Reconsidering sequential double running suture removal after penetrating keratoplasty: a prospective randomized study comparing excimer laser and motor trephination. Cornea. 2018;37(3):301–6.
Hoppenreijs VPT, van Rij G, Beekhuis WH, et al. Causes of high astigmatism after keratoplasty. Doc Ophthalmol. 1993;85:21–34.
Seitz B, Szentmáry N, Langenbucher A, et al. PKP for keratoconus—from hand/motor trephine to excimer laser and back to femtosecond. Klin Monatsbl Augenheilkd. 2016;233:727–36.
Naumann GOH, Seitz B, Lang GK, et al. 193 nm excimer laser trephination in penetrating keratoplasty. Klin Monatsbl Augenheilkd. 1993;203:252–61.
Steinert RF, Ignacio TS, Sarayba MA. “Top hat”-shaped penetrating keratoplasty using the femtosecond laser. Am J Ophthalmol. 2007;143:689–91.
Price FW, Price MO. Femtosecond laser shaped penetrating keratoplasty: one-year results utilizing a top-hat configuration. Am J Ophthalmol. 2008;145:210–4.
Seitz B, Langenbucher A, Kus MM, et al. Nonmechanical corneal trephination with the excimer laser improves outcome after penetrating keratoplasty. Ophthalmology. 1999;106:1156–64.
Birnbaum F, Wiggermann A, Maier PC, et al. Clinical results of 123 femtosecond laser-assisted penetrating keratoplasties. Graefe’s Arch Clin Exp Ophthalmol. 2013;251:95–103.
Szentmáry N, Langenbucher A, Naumann GOH, et al. Intra-individual variability of penetrating keratoplasty outcome after excimer laser versus motorized corneal trephination. J Refract Surg. 2006;22:804–10.
Chamberlain WD, Rush SW, Mathers WD, et al. Comparison of femtosecond laser-assisted keratoplasty versus conventional penetrating keratoplasty. Ophthalmology. 2011;118:486–91.
Gaster RN, Dumitrascu O, Rabinowitz YS. Penetrating keratoplasty using femtosecond laser-enabled keratoplasty with zig–zag incisions versus a mechanical trephine in patients with keratoconus. Br J Ophthalmol. 2012;96:1195–9.
Daniel MC, Böhringer D, Maier P, et al. Comparison of long-term outcomes of femtosecond laser-assisted keratoplasty with conventional keratoplasty. Cornea. 2016;35:293–8.
Resch MD, Zemova E, Marsovszky L, et al. In vivo confocal microscopic imaging of the cornea after femtosecond and excimer laser-assisted penetrating keratoplasty. J Refract Surg. 2015;31:620–6.
Tóth G, Butskhrikidze, Seitz B, et al. Endothelial cell density and corneal graft thickness following excimer laser vs. femtosecond laser-assisted penetrating keratoplasty—a prospective randomized study. Graefes Arch Clin Exp Ophthalmol. 2019;257:975–81.
El-Husseiny M, Seitz B, Langenbucher A, et al. Excimer versus femtosecond laser assisted penetrating keratoplasty in keratoconus and Fuchs dystrophy: intraoperative pitfalls. J Ophthalmol. 2015;2015:645830.
Hoffmann F. Suture technique for penetrating keratoplasty. Klin Monbl Augenheilkd. 1976;169:584–90.
Olson RJ. Modulation of postkeratoplasty astigmatism by surgical and suturing techniques. Int Ophthalmol Clin. 1983;23:137–51.
Naumann GOH. Corneal transplantation in anterior segment diseases. The Bowman lecture. Eye. 1995;9:395–421.
Seitz B, Langenbucher A, Hager T, et al. Penetrating keratoplasty for keratoconus—excimer versus femtosecond laser trephination. Open Ophthalmol J. 2017;11:225–40.
Perl T, Charlton KH, Binder PS. Disparate diameter grafting. Astigmatism, intraocular pressure, and visual acuity. Ophthalmology. 1981;88:774–81.
Seitz B, Langenbucher A. Naumann GOH [Perspectives of excimer laser-assisted keratoplasty]. Ophthalmologe. 2011;108:817–24.
Van Rij G, Waring GO III. Configuration of corneal trephine opening using five different trephines in human donor eyes. Arch Ophthalmol. 1988;106:1228–33.
Farid M, Steinert RF, Gaster RN, et al. Comparison of penetrating keratoplasty performed with a femtosecond laser zig-zag incision versus conventional blade trephanation. Ophthalmology. 2009;116:1638–43.
Shumway CL, Aggrawal S, Farid M, et al. Penetrating keratoplasty using the femtosecond laser: a comparison of postoperative visual acuity and astigmatism by suture pattern. Cornea. 2018;37:1490–6.
Mader TH, Yuan R, Lynn MJ, et al. Changes in keratometric astigmatism after suture removal more than 1 year after penetrating keratoplasty. Ophthalmology. 1993;100:119–27.
Lin DTC, Wilson SE, Reidy JJ, et al. Topographic changes that occur with 10-0 running suture removal following penetrating keratoplasty. Refract Corneal Surg. 1990;6:21–5.
Acknowledgements
We hereby thank all the participants of the study.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the University of Saarland.
Medical Writing Assistance
Language editing and assistance for this article were provided by San Francisco Edit (San Francisco, USA) and funded by the University of Saarland.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Gábor Tóth, Nóra Szentmáry, Achim Langenbucher, Elina Akhmedova, Moatasem El-Husseiny and Berthold Seitz have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the Ethics Committee of Saarland University, Germany (no. 201/11). All procedures performed in our study involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent for participation and publication of patient data was obtained from all individual participants included in the study.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.9929915.
Rights and permissions
About this article
Cite this article
Tóth, G., Szentmáry, N., Langenbucher, A. et al. Comparison of Excimer Laser Versus Femtosecond Laser Assisted Trephination in Penetrating Keratoplasty: A Retrospective Study. Adv Ther 36, 3471–3482 (2019). https://doi.org/10.1007/s12325-019-01120-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-019-01120-3