Abstract
Objective
The objective of the study was to assess the efficacy of propofol and midazolam as an intravenous sedative agent in minor oral surgical procedures in terms of: (a) the onset of action, (b) heart rate, (c) oxygen saturation, (d) systolic and diastolic blood pressure, (e) respiratory rate, (f) pain during the injection of sedative agent, (g) recovery period, (h) side effects, (i) patient’s cooperation during the surgery.
Methodology
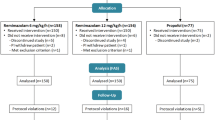
This was a double blind randomized study in which one group of 20 patients received propofol with the induction dose of 0.5 mg/kg and 50 μg/kg/min which was administered by syringe infusion pump as a maintenance dose and the other group received midazolam in a single dose of 75 μg/kg and no maintenance dose was given, instead 5 % dextrose was administered by syringe infusion pump at the rate of 50 μg/kg/min. Since propofol was milky white in colour, a green cloth was covered over the infusion pump in all cases. The surgeon, assistants and observers were blind about the medications which would be given to the patient for sedation. After the administration of the sedative, local anesthesia was achieved with 2 % lignocaine hydrochloride.
Results
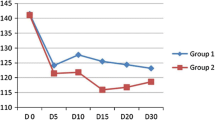
The onset of action in propofol group was significant as onset of action was faster. The maximum increase in heart rate in propofol group was at 10 min intraoperatively (Mean ± 80.40 ± 12.73) and that in midazolam group was at 15 min intraoperatively (Mean 79.25 ± 13.44). Post operatively the heart rate decreased near to the baseline value in both the groups. The average oxygen saturation before induction in propofol group was 99.7 ± 0.73 % and that of midazolam group was 99.15 ± 01.31 P = 0.314. None of the patients in this study developed apnea. The systolic blood pressure (Mean ± SD) before induction in both the groups decreased from the baseline value after the administration of sedatives. The diastolic blood pressure (Mean ± SD) before induction in both the groups decreased from the baseline value after the administration of sedatives and the decreased diastolic blood pressure was maintained throughout the procedure. The respiratory rate (Mean ± SD) before induction in both the groups decreased from the baseline value after the administration of sedatives. The decreased respiratory rate remained throughout the surgical procedure. Pain during the injection of the sedatives was reported by nine patients (45 %) in the propofol group whereas none of the patients in midazolam group complained of pain during the injection. This is statistically significant (P = 0.001). The recovery time (Mean ± SD) in propofol group was 22.50 ± 3.04 (range 15–25 min) and that in midazolam group was 33.75 ± 3.93 (range 30–40 min), which was statistically significant (P < 0.001). Patients in the propofol group were significantly less co-operative than midazolam group at both 10 and 25 min intra operatively.
Conclusion
The design of the present study permitted qualitative assessment of propofol and midazolam as sedative agents in minor oral surgical procedures. The ideal anesthetic agent should provide rapid onset of action, profound intra operative amnesia while ensuring rapid recovery without much complications. There were no significant differences in either patient demographics or surgical characteristics between the two groups. The propofol group was less co-operative than midazolam group. Pain during the injection of sedative was a significant adverse effect in the propofol group. Cardiovascular parameters remained stable throughout the procedure in both study groups and no intervention was required. However recovery and onset of action was faster in the propofol group as compared with the midazolam group.








Similar content being viewed by others
References
Milgrom P, Weinstein P, Fiset L, Beirne R (1994) The anxiolytic effects of intravenous sedation using midazolam alone or in multiple drug techniques. J Oral Maxillofac Surg 52:219–224
Parworth LP, Frost DE, Zuniga JR, Bennet T (1998) Propofol and fentanyl compared with midazolam and fentanyl during third molar surgery. J Oral Maxillofac Surg 56:447–453
Bennet J (1999) Intravenous anesthesia for oral and maxillofacial office practice. Clin N Am 11(4):601–610
Hass DA (2001) Pharmacology of agents used for intravenous sedation. Oral Maxillofac Surg Clin North Am 13(1):75–84
Dembo JB (1995) Methohexital versus propofol for outpatient anesthesia part II. J Oral Maxillofac Surg 53:816–820
Fuji Y, Uemura A, Nakano M (2002) Small dose of propofol for preventing nausea and vomiting after third molar extraction. J Oral Maxillofac Surg 60:1246–1249
Kevin JM (1998) Incremental bolus versus a continuous infusion of propofol for deep sedation/general anesthesia during dentoalveolar surgery. J Oral Maxillofac Surg 46:1053–1054
Candelaria LM, Kuhen S (1995) Propofol infusion technique for outpatient general anesthesia. J Oral Maxillofac Surg 53:124–128
Mackenze N, Grant IS (1987) Propofol for intravenous sedation. Anesth Analog 42:3–6
Cook LB, Lockwood GG, Moore CM, Whitwam JG (1993) True patient-controlled sedation. Anaesthesia 48:1039–1044
Tucker MR, Ochs MW, White RP (1986) Arterial blood gas levels after midazolam or diazepam administered with or without fentanyl as an intravenous sedative for outpatient surgical procedures. J Oral Maxillofac Surg 44:688–692
Rodrigo C, Chow K-C (1995) A comparison of 1- and 3- minute lockout periods during patient-controlled sedation with midazolam. J Oral Maxillofac Surg 53:406–408
Rudkin GE, Osborne GA, Finn BP, Vickers D (1992) Intra-operative patient-controlled sedation. Anaesthesia 47:376–381
Rodrigo C, Irwin MG, Wong MH (2004) Patient-controlled sedation with propofol in minor oral surgery. J Oral Maxillofac Surg 62:52–56
Meyers CJ, Eisig SB, Kraut RA (1994) Comparison of propofol and methohexital for deep sedation. J Oral Maxillofac Surg 52:449–452
Rodrigo C, Rosenquist JB (1998) Effect of conscious sedation with midazolam on oxygen saturation. J Oral Maxillofac Surg 46:746–750
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hari Keerthy, P., Balakrishna, R., Srungeri, K.M. et al. Comparitive Evaluation of Propofol and Midazolam as Conscious Sedatives in Minor Oral Surgery. J. Maxillofac. Oral Surg. 14, 773–783 (2015). https://doi.org/10.1007/s12663-014-0676-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-014-0676-y