Abstract
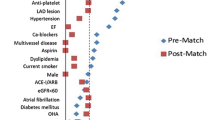
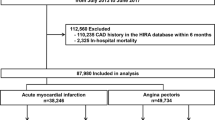
The effect of β-blockers in ST-elevation myocardial infarction (STEMI) patients who have undergone primary percutaneous coronary intervention (PCI) has not been adequately evaluated. Using a large multi-center registry in Japan, we identified 3,692 patients who underwent PCI within 24 h from onset of STEMI and were discharged alive from 2005 to 2007. Three-year cardiovascular outcomes were compared between the 2 groups of patients with (N = 1,614) or without (N = 2,078) β-blocker prescription at discharge. Compared with patients in the no-β group, patients in the β group were younger, more frequently male, more often had hypertension and atrial fibrillation but less often had chronic obstructive pulmonary disease than in the no-β group. Statins and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers were more frequently prescribed in the β group. Crude incidence of cardiac death and/or recurrent myocardial infarction (cardiac death/MI) tended to be higher in the β group (7.6 vs. 6.2 %, log-rank p = 0.1). After adjusting for potential confounders, β-blockers were associated with significantly higher risk for cardiac death/MI (hazard ratio 1.43, 95 % CI: 1.06–1.94, p = 0.01). β-Blocker prescription at discharge was not associated with better cardiovascular outcomes in patients who underwent PCI after STEMI. Large-scale randomized controlled trials are needed to evaluate the role of β-blocker therapy in these patients.


Similar content being viewed by others
References
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction–executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation. 2004;110:588–636.
Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909–45.
Beta-blocker Heart Attack Study Group. The Βeta-blocker heart-attack trial. JAMA. 1981;246:2073–4.
Freemantle N, Cleland J, Young P, Mason J, Harrison J. β blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318:1730–7.
Kernis SJ, Harjai KJ, Stone GW, Grines LL, Boura JA, O’Neill WW, et al. Does β-blocker therapy improve clinical outcomes of acute myocardial infarction after successful primary angioplasty? J Am Coll Cardiol. 2004;43:1773–9.
Ozasa N, Kimura T, Morimoto T, Hou H, Tamura T, Shizuta S, et al. Lack of effect of oral β-blocker therapy at discharge on long-term clinical outcomes of ST-segment elevation acute myocardial infarction after primary percutaneous coronary intervention. Am J Cardiol. 2010;106:1225–33.
Serruys PW, Ong ATL, van Herwerden LA, Sousa JE, Jatene A, Bonnier JJRM, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease—the final analysis of the arterial revascularization therapies study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575–81.
Kimura T, Morimoto T, Nakagawa Y, Tamura T, Kadota K, Yasumoto H, et al. Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation. 2009;119:U120–987.
Ghali WA, Quan H, Brant R, van Melle G, Norris CM, Faris PD, et al. Comparison of 2 methods for calculating adjusted survival curves from proportional hazards models. JAMA. 2001;286:1494–7.
Parsons LS. Reducing bias in a propensity score matched pair sample using greedy matching techniques. In: Proceedings of the 26th Annual SAS Users Group International Conference. Cary: SAS Institute Inc.; 2001.
Kohro T, Hayashi D, Yamazaki T, JCAD Investigators. Beta-blocker prescription among Japanese cardiologists and its effect on various outcomes. Circ J. 2010;74:962–9.
Kasanuki H, Honda T, Haze K, Sumiyoshi T, Horie T, Yagi M, et al. A large-scale prospective cohort study on the current status of therapeutic modalities for acute myocardial infarction in Japan: rationale and initial results of the HIJAMI Registry. Am Heart J. 2005;150:411–8.
The Japanese β-blockers and Calcium Antagonists Myocardial Infarction (JBCMI) Investigators. Comparison of the effects of β blockers and calcium antagonists on cardiovascular events after acute myocardial infarction in Japanese subjects. Am J Cardiol. 2004;93:969–73.
Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:995–1003.
Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005;366:895–906.
Lindholm LH, Carlberg B, Samuelsson O. Should β blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366:1545–53.
Kopecky SL. Effect of β blockers, particularly carvedilol, on reducing the risk of events after acute myocardial infarction. Am J Cardiol. 2006;98:1115–9.
Cimmino G, Ibanez B, Giannarelli C, Prat-Gonzalez S, Hutter R, Garcia M, Sanz J, Fuster V, Badimon JJ. Carvedilol administration in acute myocardial infarction results in stronger inhibition of early markers of left ventricular remodeling than metoprolol. Int J Cardiol. 2011;153:256–61.
Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001;357:1385–90.
Bristow MR, Gilbert EM, Abraham WT, Adams KF, Fowler MB, Hershberger RE, MOCHA Investigators, et al. Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. Circulation. 1996;94:2807–16.
Mehta RH, Starr AZ, Lopes RD, Hochman JS, Widimsky P, Pieper KS, et al. Incidence of and outcomes associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention. JAMA. 2009;301:1779–89.
Xie HG, Kim RB, Wood AJ, Stein CM. Molecular basis of ethnic differences in drug disposition and response. Annu Rev Pharmacol Toxicol. 2001;41:815–50.
Hori M, Sasayama S, Kitabatake A, Toyo-oka T, Handa S, Yokoyama M, et al. Low-dose carvedilol improves left ventricular function and reduces cardiovascular hospitalization in Japanese patients with chronic heart failure: the Multicenter Carvedilol Heart Failure Dose Assessment (MUCHA) trial. Am Heart J. 2004;147:324–30.
Ho PM, Spertus JA, Masoudi FA, Reid KJ, Peterson ED, Magid DJ, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166:1842–7.
Butler J, Arbogast PG, BeLue R, Daugherty J, Jain MK, Ray WA, et al. Outpatient adherence to β-blocker therapy after acute myocardial infarction. J Am Coll Cardiol. 2002;40:1589–95.
Acknowledgments
All authors have contributed to the design of the study, interpretation of results, revising the manuscript, and approve the final version of the manuscript. We thank the members of the cardiac catheterization laboratories of the participating centers and the clinical research coordinators (Supplemental Appendix). This study was supported by the Pharmaceuticals and Medical Devices Agency (PMDA) in Japan.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the CREDO-Kyoto AMI registry investigators.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bao, B., Ozasa, N., Morimoto, T. et al. β-Blocker therapy and cardiovascular outcomes in patients who have undergone percutaneous coronary intervention after ST-elevation myocardial infarction. Cardiovasc Interv and Ther 28, 139–147 (2013). https://doi.org/10.1007/s12928-012-0137-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-012-0137-9