Abstract
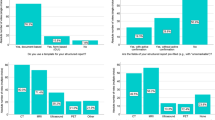
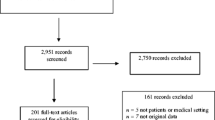
Using the standardized ASCO Quality Oncology Practice Initiative (QOPI) guidelines for assessing quality cancer care, we identified communication about intent of chemotherapy as an area needing improvement in our program at the University of Arkansas for Medical Sciences (UAMS) and the Central Arkansas Veterans Healthcare System (CAVHS). We organized training in communications on intent of treatment (palliative vs curative) and added optional checkboxes to our electronic templates for progress notes. Afterwards, we conducted a retrospective review of electronic medical records of initially often randomly selected patient charts. The first 10 patient charts after 1 month of implementation showed intent of treatment in 80 % of charts compared to 74 % at baseline. We then changed checkboxes from mandatory to optional and reviewed 30 randomly selected patient charts. Intent of treatment was documented in 96.7 % of cases compared to 74 % at baseline. We also assessed patient satisfaction through surveys distributed in clinic. Patient satisfaction scores were close to 100 % for receiving clear information, understanding the reason for which they were receiving chemotherapy, and willingness of oncologists to listen carefully, to take time to answer questions, to explain things clearly, and to spend adequate time with them. In this study, we showed that training in communication of intent of chemotherapy and use of checkboxes in progress note templates could improve competency in communication of intent of therapy in cancer patients.





Similar content being viewed by others
References
McNiff K (2006) The quality oncology practice initiative: assessing and improving care within the medical oncology practice. J Oncol Pract 2(1):26–30
http://www.iom.edu/About-IOM.aspx. The Institute of Medicine of the National Academics
American Society of Clinical Oncology: The Quality Oncology Practice Initiative, 2009. http://qopi.asco.org/32
Moen R, Norman C (2006) Evolution of the PDCA cycle
Speroff T, O’Connor GT (2004) Study designs for PDSA quality improvement research. Qual Manag Health Care 13:17–32
Cushing A, Abbott S, Lothian D, Hall A, Westwood OM (2011) Peer feedback as an aid to learning--what do we want? Feedback. When do we want it? Now! Med Teach 33(2):e105–e112. doi:10.3109/0142159X.2011.542522
Hill E, Liuzzi F, Giles J (2010) Peer-assisted learning from three perspectives: student, tutor and co-ordinator. Clin Teach 7(4):244–246. doi:10.1111/j.1743-498X.2010.00399.x
Buckman R, Kason Y (1992) How to break bad news: a guide for health care professionals. The John Hopkins University Press, Baltimore, Maryland
Conflict of Interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bansal, M., Abdallah, AO., Pennisi, A. et al. Improving Communication on Intent of Chemotherapy Using QOPI Scores and PDSA Cycles. J Canc Educ 31, 736–741 (2016). https://doi.org/10.1007/s13187-015-0897-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-015-0897-x