Abstract
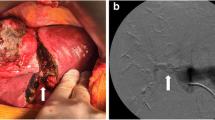
The limit to surgical treatment of patients with hepatic tumors is represented by the proportion of residual hepatic parenchyma at the end of surgery (FLR, future liver remnant) that provides an estimation of the risk of postoperative liver failure. Recently, a new two-stage technique has been developed with the acronym (ALPPS) associating liver partitioning and portal vein ligation for staged hepatectomy with the aim of obtaining a more rapid and effective increase in FLR, even though indications are not clear yet. Between January and December 2012, eight patients were candidates to ALPPS at the Hepatobiliary Surgery Unit of San Raffaele Hospital, Milan. The first three patients (Series 1) underwent right trisectionectomy and were affected by tumors infiltrating biliary confluence, while the others (Series 2) were candidates to right hepatectomy for colorectal liver metastases. Two patients were then excluded from Series 2 because intraoperative finding of irresectable disease. Intra- and postoperative outcome was evaluated with the aim of defining indications to ALPPS. All patients reached an adequate FLR after a median of 7.5 days from the first procedure (rate of program completion 100 %). In Series 1 two patients developed complications related to bile leakage from the raw surface of the liver to be resected and septic events secondary to ischemic necrosis of the liver segment IV. One patient died following multi-organ failure secondary to sepsis. In Series 2 postoperative course was uneventful in all the patients, and in particular no patient showed disease progression between the two procedures or signs of postoperative liver failure. ALPPS approach was initially considered suitable for patients affected by Klatskin tumors who require, despite a small tumor volume, extended hepatectomies associated with surgery of the biliary tract: the analysis of this first series of patients has led to a re-evaluation of the indication to this strategy, as a consequence of encountered criticisms. Actually only a subset of patients affected by colorectal liver metastases are candidates to ALPPS.


Similar content being viewed by others
References
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH (2002) Improvement in perioperative outcome after hepatic resection: analysis of 1.803 consecutive cases over the past decade. Ann Surg 236(4):397–406
Garcea G, Ong SL, Maddern GJ (2009) Predicting liver failure following major hepatectomy. Dig Liver Dis 41(11):798–806
Shoup M, Gonen M, D’Angelica M, Jarnagin WR, DeMatteo RP, Schwartz LH, Tuorto S, Blumgart LH, Fong Y (2003) Volumetric analysis predicts hepatic dysfunction in patients undergoing major liver resection. J Gastrointest Surg 7:325–330
Ferrero A, Vigano L, Polastri R, Muratore A, Eminefendic H, Regge D, Capussotti L (2007) Postoperative liver dysfunction and future remnant liver: where is the limit? results of a prospective study. World J Surg 31:1643–1651
Ratti F, Soldati C, Catena M, Paganelli M, Ferla G, Aldrighetti L (2010) Role of portal vein embolization in liver surgery: single centre experience in sixty two patients. Updates Surg 62(3–4):153–159
de Baere T, Roche A, Elias D, Lasser P, Lagrange C, Bousson V (1996) Preoperative portal vein embolization for extension of hepatectomy indications. Hepatology 24:1386–1391
Abulkhir A, Limongelli P, Healey AJ, Damrah O, Tait P, Jackson J, Habib N, Jiao L (2008) Preoperative portal vein embolization for major liver resection. A meta-analysis. Ann Surg 247:49–57
Van Liended KP, van den Esschert JW, de Graaf W, Bipat S, Lameris JS, van Gulik TM, van Delden OM (2013) Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol 36(1):25–34
De Santibanes E, Clavien PA (2012) Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg 255(3):415–417
Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T, Goralcyk A, Horbelt R, Kroemer A, Loss M, Rummele P, Scherer MN, Padberg W, Konigsrainer A, Lang H, Obed A, Schlitt HJ (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small for size settings. Ann Surg 255(3):405–414
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F (2005) The “50-50 criteria” on postoperative day 5:an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242(6):824–828
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan ST, Nimura Y, Figueras J, Capussotti L, Buchler MW, Weitz J (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149(5):713–724
Fürst G, Schulte am Esch J, Poll LW, Hosch SB, Fritz LB, Klein M, Godehardt E, Krieg A, Wecker B, Stoldt V, Stockschläder M, Eisenberger CF, Mödder U, Knoefel WT (2007) Portal vein embolization and autologous CD133 + bone marrow stem cells for liver regeneration: initial experience. Radiology 243:171–179
Lam VW, Laurence JM, Johnston E, Hollands MJ, Pleass HC, Richardson AJ (2013) A systematic review of two-stage hepatectomy in patients with initially unresectable colorectal liver metastases. HPB 15(7):483–491
De Santibanes E, Alvarez FA, Ardiles V (2012) How to avoid postoperative liver failure: a novel method. World J Surg 36:125–128
Adam R, Laurent A, Azoulay D, Castaing D, Bismuth H (2000) Two stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann Surg 232(6):777–785
Jaeck D, Oussoultzoglou E, Rosso E, Greget M, Weber JC, Bachellier P (2004) A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple an bilobar liver metastases. Ann Surg 240(6):1037–1049
Sala S, Ardiles V, Ulla M, Alvarez F, Pekoli J, de Santibanes E (2012) Our initial experience with ALPPS technique: encouraging results. Updates Surg 64(3):167–172
Knoefel WT, Gabor I, Rehders A, Alexander A, Krausch M, Schukte am Esch J, Fürst G, Topp SA (2013) In situ liver transection with portal vein ligation for rapid growth of the future liver remnant in two-stage liver resection. Br J Surg 100(3):388–394
Alvarez FA, Ardiles V, Sanchez Claria R, Pekoli J, de Santibanes E (2012) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS):tips and tricks. J Gastrointest Surg 17(4):814–821
Li J, Girotti P, Konigsrainer I, Ladurner R, Konigsrainer A, Nadalin S (2013) ALPPS in right trisectionectomy: a safe procedure to avoid postoperative liver failure? J Gastrointest Surg 17(5):956–961
Kokudo N, Tada K, Seki M, Ohta H, Azekura K, Ueno M, Ohta K, Yamaguchi T, Matsubara T, Takahashi T, Nakajima T, Muto T, Ikari T, Yanagisawa A, Kato Y (2001) Proliferative activity of intrahepatic colorectal metastases after preoperative hemihepatic portal vein embolization. Hepatology 34(2):267–272
Andriani OC (2012) Long-term results with associating liver partition and portal vein ligation for staged hepatectomy (ALPPS). Ann Surg 256(3):e5
Aloia TA, Vauthey JN (2012) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): what is gained and what is lost? Ann Surg 256(3):e9
Neuhaus P, Thelen A, Jonas S, Puhl G, Denecke T, Veltzke-Schlieker W, Seehofer D (2012) Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann Surg Oncol 19(5):1602–1608
Yagi S, Uemoto S (2012) Small-for-size syndrome in living donor liver transplantation. Hepatobiliary Pancreat Dis Int 11(6):570–576
Hammond JS, guha IN, Beckingham IJ, Lobo DN (2011) Prediction, prevention and management of postresection liver failure. Br J Surg 98(9):1188–1200
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ratti, F., Cipriani, F., Gagliano, A. et al. Defining indications to ALPPS procedure: technical aspects and open issues. Updates Surg 66, 41–49 (2014). https://doi.org/10.1007/s13304-013-0243-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-013-0243-y