Abstract
Objective
The aim of this retrospective analysis is to evaluate the role of stereotactic radiosurgery (SRS) in treating multiple myeloma (MM) of the spine.
Methods
Medical records of MM patients who underwent single fraction spine SRS between 6/2001 and 12/2014 at our institution were retrospectively reviewed in this institutional review board-approved analysis. Post-treatment radiographic, neurologic, and pain response were the primary endpoints. Endpoints were evaluated with periodic clinical exams and imaging studies (magnetic resonance imaging and computed tomography).
Results
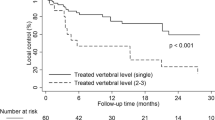
Median SRS dose was 16 Gy (10–18) in a single fraction. Seventy-eight patients (121 treatment sites) were treated. Clinical follow-up was available for 71 patients. Radiographic follow-up was available for 94 treatment sites. Median follow-up was 27.8 months (24 days–12.1 years). Radiographic control was observed in 89.4% of the treated sites. Pain relief occurred in 88.3% of the patients that presented with pain; pain progression occurred in 3.3%. Neurological improvement was observed in 63.6% of the patients that presented with a deficit. In sites where MM approached or compressed the epidural canal or the thecal sac, after SRS, evidence of radiographic regression was observed in 87.1%. Toxicities observed included one patient who experienced a tracheoesophageal fistula 2 years after SRS. After SRS, there were 39 VCFs that were potentially SRS-induced.
Conclusion
SRS appears to be effective in the treatment of MM of the spine. To the best of our knowledge, this is the largest such experience reported.

Similar content being viewed by others
References
Coleman RE (2006) Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 12(20 Pt 2):6243s–6249s
Frosch MP, Anthony DC, De Girolami U (2010) The central nervous system. In: Kumar V, Abbas AK, Fausto N, Aster JC (eds) Robbins and cotran pathologic basis of disease, 8th edn. Saunders, Philadelphia, pp 1279–1344
Loblaw DA, Laperriere NJ (1998) Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol 16(4):1613–1624
Mak KS, Lee LK, Mak RH, Wang S, Pile-Spellman J, Abrahm JL, Prigerson HG, Balboni TA (2011) Incidence and treatment patterns in hospitalizations for malignant spinal cord compression in the United States, 1998–2006. Int J Radiat Oncol Biol Phys 80(3):824–831
Loblaw DA, Laperriere NJ, Mackillop WJ (2003) A population-based study of malignant spinal cord compression in Ontario. Clin Oncol (Royal College of Radiologists (Great Britain)) 15(4):211–217
Schiff D, O'Neill BP, Suman VJ (1997) Spinal epidural metastasis as the initial manifestation of malignancy: clinical features and diagnostic approach. Neurology 49(2):452–456
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66(1):7–30
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67(1):7–30
Talamo G, Dimaio C, Abbi KK, Pandey MK, Malysz J, Creer MH, Zhu J, Mir MA, Varlotto JM (2015) Current role of radiation therapy for multiple myeloma. Front Oncol 5:40
Featherstone C, Delaney G, Jacob S, Barton M (2005) Estimating the optimal utilization rates of radiotherapy for hematologic malignancies from a review of the evidence: part II-leukemia and myeloma. Cancer 103(2):393–401
Rades D, Huttenlocher S, Dunst J, Bajrovic A, Karstens JH, Rudat V, Schild SE (2010) Matched pair analysis comparing surgery followed by radiotherapy and radiotherapy alone for metastatic spinal cord compression. J Clin Oncol 28(22):3597–3604
Rades D, Veninga T, Stalpers LJ, Basic H, Rudat V, Karstens JH, Dunst J, Schild SE (2007) Outcome after radiotherapy alone for metastatic spinal cord compression in patients with oligometastases. J Clin Oncol 25(1):50–56
Maranzano E, Latini P (1995) Effectiveness of radiation therapy without surgery in metastatic spinal cord compression: final results from a prospective trial. Int J Radiat Oncol Biol Phys 32(4):959–967
Lutz S, Berk L, Chang E, Chow E, Hahn C, Hoskin P, Howell D, Konski A, Kachnic L, Lo S, Sahgal A, Silverman L, von Gunten C, Mendel E, Vassil A, Bruner DW, Hartsell W, American Society for Radiation Oncology (2011) Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys 79(4):965–976
Ryu S, Fang Yin F, Rock J, Zhu J, Chu A, Kagan E, Rogers L, Ajlouni M, Rosenblum M, Kim JH (2003) Image-guided and intensity-modulated radiosurgery for patients with spinal metastasis. Cancer 97(8):2013–2018
Gerszten PC, Ozhasoglu C, Burton SA, Vogel WJ, Atkins BA, Kalnicki S, Welch WC (2004) CyberKnife frameless stereotactic radiosurgery for spinal lesions: clinical experience in 125 cases. Neurosurgery 55(1):89–98 discussion 98-89
Guckenberger M, Mantel F, Gerszten PC, Flickinger JC, Sahgal A, Letourneau D, Grills IS, Jawad M, Fahim DK, Shin JH, Winey B, Sheehan J, Kersh R (2014) Safety and efficacy of stereotactic body radiotherapy as primary treatment for vertebral metastases: a multi-institutional analysis. Radiat Oncol (London, England) 9(1):226
Jin R, Rock J, Jin JY, Janakiraman N, Kim JH, Movsas B, Ryu S (2009) Single fraction spine radiosurgery for myeloma epidural spinal cord compression. J Exp Ther Oncol 8(1):35–41
Schipani S, Wen W, Jin JY, Kim JK, Ryu S (2012) Spine radiosurgery: a dosimetric analysis in 124 patients who received 18 Gy. Int J Radiat Oncol Biol Phys 84(5):e571–e576
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer (Oxford, England: 1990) 45(2):228–247
Ropper AH, Samuels MA, Klein JP (2014) Approach to the patient with neurologic disease. In: Ropper AH, Samuels MA, Klein JP (eds) Adams and Victor's principles of neurology, 10th edn. McGraw-Hill, New York
Bilsky MH, Laufer I, Fourney DR, Groff M, Schmidt MH, Varga PP, Vrionis FD, Yamada Y, Gerszten PC, Kuklo TR (2010) Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine 13(3):324–328
Boyce-Fappiano D, Elibe E, Schultz L, Ryu S, Siddiqui MS, Chetty I, Lee I, Rock J, Movsas B, Siddiqui F (2017) Analysis of the factors contributing to vertebral compression fractures after spine stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 97(2):236–245
Ryu S, Jin JY, Jin R, Rock J, Ajlouni M, Movsas B, Rosenblum M, Kim JH (2007) Partial volume tolerance of the spinal cord and complications of single-dose radiosurgery. Cancer 109(3):628–636
Ryu S, Rock J, Jain R, Lu M, Anderson J, Jin JY, Rosenblum M, Movsas B, Kim JH (2010) Radiosurgical decompression of metastatic epidural compression. Cancer 116(9):2250–2257
Choi CY, Adler JR, Gibbs IC, Chang SD, Jackson PS, Minn AY, Lieberson RE, Soltys SG (2010) Stereotactic radiosurgery for treatment of spinal metastases recurring in close proximity to previously irradiated spinal cord. Int J Radiat Oncol Biol Phys 78(2):499–506
Garg AK, Wang XS, Shiu AS, Allen P, Yang J, McAleer MF, Azeem S, Rhines LD, Chang EL (2011) Prospective evaluation of spinal reirradiation by using stereotactic body radiation therapy: the University of Texas MD Anderson Cancer Center experience. Cancer 117(15):3509–3516
Mahadevan A, Floyd S, Wong E, Jeyapalan S, Groff M, Kasper E (2011) Stereotactic body radiotherapy reirradiation for recurrent epidural spinal metastases. Int J Radiat Oncol Biol Phys 81(5):1500–1505
Boyce-Fappiano D, Elibe E, Zhao B, Siddiqui MS, Lee I, Rock J, Ryu S, Siddiqui F (2017) Reirradiation of the spine with stereotactic radiosurgery: efficacy and toxicity. Pract Radiat Oncol. https://doi.org/10.1016/j.prro.2017.05.007
Osborne TR, Ramsenthaler C, de Wolf-Linder S, Schey SA, Siegert RJ, Edmonds PM, Higginson IJ (2014) Understanding what matters most to people with multiple myeloma: a qualitative study of views on quality of life. BMC Cancer 14:496
Miller JA, Balagamwala EH, Chao ST, Emch T, Suh JH, Djemil T, Angelov L (2016) Spine stereotactic radiosurgery for the treatment of multiple myeloma. J Neurosurg Spine 26(3):1–9. https://doi.org/10.3171/2016.8.SPINE16412
Rades D, Hoskin PJ, Stalpers LJ, Schulte R, Poortmans P, Veninga T, Dahm-Daphi J, Obralic N, Wildfang I, Bahrehmand R, Engenhart-Cabilic R, Schild SE (2006) Short-course radiotherapy is not optimal for spinal cord compression due to myeloma. Int J Radiat Oncol Biol Phys 64(5):1452–1457
Brown JM, Carlson DJ, Brenner DJ (2014) The tumor radiobiology of SRS and SBRT: are more than the 5 Rs involved? Int J Radiat Oncol Biol Phys 88(2):254–262
Bate BG, Khan NR, Kimball BY, Gabrick K, Weaver J (2015) Stereotactic radiosurgery for spinal metastases with or without separation surgery. J Neurosurg Spine 22(4):409–415
Ejima Y, Matsuo Y, Sasaki R (2015) The current status and future of radiotherapy for spinal bone metastases. J Orthop Sci 20(4):585–592
Terpos E, Berenson J, Raje N, Roodman GD (2014) Management of bone disease in multiple myeloma. Expert Rev Hematol 7(1):113–125
Al-Omair A, Smith R, Kiehl TR, Lao L, Yu E, Massicotte EM, Keith J, Fehlings MG, Sahgal A (2013) Radiation-induced vertebral compression fracture following spine stereotactic radiosurgery: clinicopathological correlation. J Neurosurg Spine 18(5):430–435
Cunha MV, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, Yu E, Howard P, Lochray F, da Costa LB, Fehlings MG, Sahgal A (2012) Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): analysis of predictive factors. Int J Radiat Oncol Biol Phys 84(3):e343–e349
Rose PS, Laufer I, Boland PJ, Hanover A, Bilsky MH, Yamada J, Lis E (2009) Risk of fracture after single fraction image-guided intensity-modulated radiation therapy to spinal metastases. J Clin Oncol 27(30):5075–5079
Sahgal A, Atenafu EG, Chao S, Al-Omair A, Boehling N, Balagamwala EH, Cunha M, Thibault I, Angelov L, Brown P, Suh J, Rhines LD, Fehlings MG, Chang E (2013) Vertebral compression fracture after spine stereotactic body radiotherapy: a multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol 31(27):3426–3431
Sung SH, Chang UK (2014) Evaluation of risk factors for vertebral compression fracture after stereotactic radiosurgery in spinal tumor patients. Korean J Spine 11(3):103–108
Kumar V, Abbas AK, Fausto N, Aster JC (2010) Diseases of white blood cells, lymph nodes, spleen, and thymus. In: Scmitt W, Gruliow R, Sinclair J, Philadelphia ZE (eds) Robbins and Cotran pathologic basis of disease. Elsevier, Saunders, pp 608–611
Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A, Fonseca R, Rajkumar SV, Offord JR, Larson DR, Plevak ME, Therneau TM, Greipp PR (2003) Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 78(1):21–33
Miller JA, Bowen A, Morisada MV, Margetis K, Lubelski D, Lieberman IH, Benzel EC, Mroz TE (2015) Radiologic and clinical characteristics of vertebral fractures in multiple myeloma. Spine J 15(10):2149–2156
Melton LJ 3rd, Kyle RA, Achenbach SJ, Oberg AL, Rajkumar SV (2005) Fracture risk with multiple myeloma: a population-based study. J Bone Miner Res 20(3):487–493
Gibbs IC, Patil C, Gerszten PC, Adler JR Jr, Burton SA (2009) Delayed radiation-induced myelopathy after spinal radiosurgery. Neurosurgery 64(2 Suppl):A67–A72
Sahgal A, Ma L, Gibbs I, Gerszten PC, Ryu S, Soltys S, Weinberg V, Wong S, Chang E, Fowler J, Larson DA (2010) Spinal cord tolerance for stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 77(2):548–553
Sahgal A, Weinberg V, Ma L, Chang E, Chao S, Muacevic A, Gorgulho A, Soltys S, Gerszten PC, Ryu S, Angelov L, Gibbs I, Wong CS, Larson DA (2013) Probabilities of radiation myelopathy specific to stereotactic body radiation therapy to guide safe practice. Int J Radiat Oncol Biol Phys 85(2):341–347
Haley ML, Gerszten PC, Heron DE, Chang YF, Atteberry DS, Burton SA (2011) Efficacy and cost-effectiveness analysis of external beam and stereotactic body radiation therapy in the treatment of spine metastases: a matched-pair analysis. J Neurosurg Spine 14(4):537–542
Acknowledgements
An abstract of a variation of this paper was previously presented as a poster at the American Society of Therapeutic Radiation Oncology 57th Annual Meeting in San Antonio, TX, October 18–21, 2015. The abstract was published in the conference proceedings (Elibe E, Boyce-Fappiano D, Ryu S, Siddiqui MSU, Wen N, Lee I, et al.: Efficacy of spine stereotactic radiosurgery for multiple myeloma epidural cord compression. Int J Radiat Oncol Biol Phys: 93(3):E456, 2015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Dr. M. Salim Siddiqui, Dr. Ning Wen, and Dr. Farzan Siddiqui are employed by the Henry Ford Hospital Department of Radiation Oncology. The Henry Ford Hospital Department of Radiation Oncology receives research funding from Philips Medical and Varian Medical Systems, Inc. entitled “SRS Education and Research Grant” grant number M60287. The funding sources had no direct involvement with the content or analysis of the material presented in this manuscript.
Conflict of interest
Dr. Ian Lee serves as a consultant for Medtronic and a speaker honorarium for Varian Medical Systems, Inc. For the remaining authors (Ms. Erinma Elibe, Dr. David Boyce-Fappiano, Dr. Samuel Ryu, and Dr. Jack Rock), no conflict of interest was declared.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Elibe, E., Boyce-Fappiano, D., Ryu, S. et al. Stereotactic radiosurgery for multiple myeloma of the spine. J Radiat Oncol 7, 37–44 (2018). https://doi.org/10.1007/s13566-017-0333-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-017-0333-4