Abstract
Objective
Fluoroquinolones and 3rd-generation cephalosporins that are prescribed for pneumonia may be avoided and replaced by a penicillin in some cases. We aimed to determine if the proportion of patients treated for pneumonia with a cephalosporin, a fluoroquinolone or both varies among Emergency Departments (EDs), and to estimate the proportion of avoidable prescriptions.
Methods
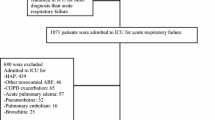
This was a retrospective study of patients treated for pneumonia in eight French EDs, and subsequently hospitalized in non-ICU wards. Third-generation cephalosporins or respiratory fluoroquinolones were presumed unavoidable if they met both criteria: (1) age ≥65 years or comorbid condition; and (2) allergy or intolerance to penicillin, or failure of penicillin, or previous treatment with penicillin, or for fluoroquinolones only, suspected legionellosis.
Results
We included 832 patients. Thirty-four percent (95 % CI, 31–38 %) of patients were treated with a cephalosporin, a respiratory fluoroquinolone or both (range among EDs 19–44 %). Four EDs were independent risk factors for prescription of a cephalosporin, a fluoroquinolone or both [adjusted OR, 2.27 (1.64–3.15)], as were immune compromise [aOR 2.54 (1.56–4.14)], antibacterial therapy started before arrival in the ED [aOR 3.32 (2.30–4.81)], REA-ICU class III or IV [aOR 1.93 (1.15–3.23)], PSI class V [aOR 1.49 (1.00–2.20)], fluid ressuscitation [aOR 3.98 (2.49–6.43)] and non-invasive ventilation in the ED [aOR, 7.18 (1.7–50.1)]. Treatment with a cephalosporin, a fluoroquinolone or both was avoidable in 67 % (62–73 %) of patients.
Conclusion
Cephalosporins and fluoroquinolones use in pneumonia is highly variable among EDs. The majority of these prescriptions are avoidable. Antibiotic stewardship programs should be implemented to restrict their use in EDs.
Similar content being viewed by others
References
Kaier K, Frank U, Hagist C, Conrad A, Meyer E. The impact of antimicrobial drug consumption and alcohol-based hand rub use on the emergence and spread of extended-spectrum beta-lactamase-producing strains: a time-series analysis. J Antimicrob Chemother. 2009;63:609–14.
Kanafani ZA, Mehio-Sibai A, Araj GF, Kanaan M, Kanj SS. Epidemiology and risk factors for extended-spectrum beta-lactamase-producing organisms: a case control study at a tertiary care center in Lebanon. Am J Infect Control. 2005;33:326–32.
Colodner R, Rock W, Chazan B, Keller N, Guy N, Sakran W, et al. Risk factors for the development of extended-spectrum beta-lactamase-producing bacteria in nonhospitalized patients. Eur J Clin Microbiol Infect Dis. 2004;23:163–7.
Rodriguez-Bano J, Alcala JC, Cisneros JM, Grill F, Oliver A, Horcajada JP, et al. Community infections caused by extended-spectrum beta-lactamase-producing Escherichia coli. Arch Intern Med. 2008;168:1897–902.
Aldeyab MA, Harbarth S, Vernaz N, Kearney MP, Scott MG, Darwish Elhajji FW, et al. The impact of antibiotic use on the incidence and resistance pattern of extended-spectrum beta-lactamase-producing bacteria in primary and secondary healthcare settings. Br J Clin Pharmacol. 2012;74:171–9.
Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52:e103–20.
Paterson DL. “Collateral damage” from cephalosporin or quinolone antibiotic therapy. Clin Infect Dis. 2004;38(Suppl 4):S341–5.
Roson B, Carratala J, Tubau F, Dorca J, Linares J, Pallares R, et al. Usefulness of betalactam therapy for community-acquired pneumonia in the era of drug-resistant Streptococcus pneumoniae: a randomized study of amoxicillin–clavulanate and ceftriaxone. Microb Drug Resist. 2001;7:85–96.
Sanchez ME, Gomez J, Gomez Vargas J, Banos V, Ruiz Gomez J, Munoz L, et al. Prospective and comparative study between cefuroxime, ceftriaxone and amoxicillin-clavulanic acid in the treatment of community-acquired pneumonia. Rev Esp Quimioter. 1998;11:132–8.
Paterson DL, Playford EG. Should third-generation cephalosporins be the empirical treatment of choice for severe community-acquired pneumonia in adults? Med J Aust. 1998;168:344–8.
Woodhead M, Blasi F, Ewig S, Garau J, Huchon G, Ieven M, et al. Guidelines for the management of adult lower respiratory tract infections—full version. Clin Microbiol Infect. 2011;17(Suppl 6):E1–59.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–72.
Goffinet N, Lecadet N, Cousin M, Peron C, Hardouin JB, Batard E, et al. Increasing use of third-generation cephalosporins for pneumonia in the emergency department: may some prescriptions be avoided? Eur J Clin Microbiol Infect Dis. 2014;33:1095–9.
Blasi F, Garau J, Medina J, Avila M, McBride K, Ostermann H. Current management of patients hospitalized with community-acquired pneumonia across Europe: outcomes from REACH. Resp Res. 2013;14:44.
Neuman MI, Ting SA, Meydani A, Mansbach JM, Camargo CA Jr. National study of antibiotic use in emergency department visits for pneumonia, 1993 through 2008. Acad Emerg Med. 2012;19:562–8.
Trinh HT, Hoang PH, Cardona-Morrell M, Nguyen HT, Vu DH, Dong PT, et al. Antibiotic therapy for inpatients with community-acquired pneumonia in a developing country. Pharmacoepidemiol Drug Saf. 2014;24:129–36.
Torres A, Blasi F, Peetermans WE, Viegi G, Welte T. The aetiology and antibiotic management of community-acquired pneumonia in adults in Europe: a literature review. Eur J Clin Microbiol Infect Dis. 2014;33:1065–79.
Kohlhammer Y, Raspe H, Marre R, Suttorp N, Welte T, Schafer T, et al. Antibiotic treatment of community acquired pneumonia varies widely across Germany. J Infect. 2007;54:446–53.
Koller D, Hoffmann F, Maier W, Tholen K, Windt R, Glaeske G. Variation in antibiotic prescriptions: is area deprivation an explanation? Analysis of 1.2 million children in Germany. Infection. 2013;41:121–7.
SPILF, AFSSAPS. Antibiothérapie par voie générale dans les infections respiratoires basses de l’adulte. Pneumonie aigue communautaire, exacerbations de bronchopneumopathie chronique obstructive 2010. http://ansm.sante.fr/var/ansm_site/storage/original/application/b33b6936699f3fefdd075316c40a0734.pdf. Last access 16 Nov 2014.
Sorde R, Falco V, Lowak M, Domingo E, Ferrer A, Burgos J, et al. Current and potential usefulness of pneumococcal urinary antigen detection in hospitalized patients with community-acquired pneumonia to guide antimicrobial therapy. Arch Intern Med. 2011;171:166–72.
Matta M, Kerneis S, Day N, Lescat M, Hoi AB, Varon E, et al. Do clinicians consider the results of the BinaxNOW Streptococcus pneumoniae urinary antigen test when adapting antibiotic regimens for pneumonia patients? Clin Microbiol Infect. 2010;16:1389–93.
Engel MF, van Velzen M, Hoepelman AI, Thijsen S, Oosterheert JJ. Positive urinary antigen tests for Streptococcus pneumoniae in community-acquired pneumonia: a 7-year retrospective evaluation of health care cost and treatment consequences. Eur J Clin Microbiol Infect Dis. 2013;32:485–92.
Duchene E, Montassier E, Boutoille D, Caillon J, Potel G, Batard E. Why is antimicrobial de-escalation under-prescribed for urinary tract infections? Infection. 2013;41:211–4.
Khasawneh FA, Karim A, Mahmood T, Ahmed S, Jaffri SF, Tate ME, et al. Antibiotic de-escalation in bacteremic urinary tract infections: potential opportunities and effect on outcome. Infection. 2014;42:829–34.
Cavalié P, Djeraba A. L’évolution des consommations d’antibiotiques en France entre 2000 et 2013. Paris: ANSM; 2014. http://ansm.sante.fr/S-informer/Actualite/Evolution-des-consommations-d-antibiotiques-en-France-entre-2000-et-2013-nouveau-rapport-d-analyse-de-l-ANSM-Point-d-Information. Last access 16 Nov 2014.
Borde JP, Litterst S, Ruhnke M, Feik R, Hubner J, deWith K, et al. Implementing an intensified antibiotic stewardship programme targeting cephalosporin and fluoroquinolone use in a 200-bed community hospital in Germany. Infection. 2015;43:45–50.
May L, Cosgrove S, L’Archeveque M, Talan DA, Payne P, Jordan J, et al. A call to action for antimicrobial stewardship in the emergency department: approaches and strategies. Ann Emerg Med. 2013;62:69–77.
Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64 Suppl 3:1–55.
Singanayagam A, Chalmers JD. Severity assessment scores to guide empirical use of antibiotics in community acquired pneumonia. Lancet Respir Med. 2013;1:653–62.
Acknowledgments
The authors acknowledge Jacques Choukroun, Philippe Fradin, Christophe Legal, Betty Mazet, Amélie Pichot, Bruno Poujol and Rachid Yousfi for helping local investigators.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the ethics committee of Centre Hospitalier Universitaire de Nantes (Number 2014-04-01).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The CEFPU1 Study Group is: Magali Croguennec, Antoine Ducongé, Anne-Marie Esnault, Juliette Foucher, Marie Olivier, Gaëlle Penhouet, Charlotte Vieillard.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Batard, E., Lecadet, N., Goffinet, N. et al. High variability among Emergency Departments in 3rd-generation cephalosporins and fluoroquinolones use for community-acquired pneumonia. Infection 43, 681–689 (2015). https://doi.org/10.1007/s15010-015-0793-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-015-0793-7