Abstract
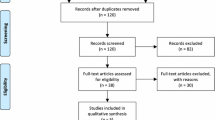
Life-threatening and benign drug reactions occur frequently in the skin, affecting 8 % of the general population and 2–3 % of all hospitalized patients, emphasizing the need for physicians to effectively recognize and manage patients with drug-induced eruptions. Neurologic medications represent a vast array of drug classes with cutaneous side effects. Approximately 7 % of the United States (US) adult population is affected by adult-onset neurological disorders, reflecting a large number of patients on neurologic drug therapies. This review elucidates the cutaneous reactions associated with medications approved by the US Food and Drug Administration (FDA) to treat the following neurologic pathologies: Alzheimer disease, amyotrophic lateral sclerosis, epilepsy, Huntington disease, migraine, multiple sclerosis, Parkinson disease, and pseudobulbar affect. A search of the literature was performed using the specific FDA-approved drug or drug classes in combination with the terms ‘dermatologic,’ ‘cutaneous,’ ‘skin,’ or ‘rash.’ Both PubMed and the Cochrane Database of Systematic Reviews were utilized, with side effects ranging from those cited in randomized controlled trials to case reports. It behooves neurologists, dermatologists, and primary care physicians to be aware of the recorded cutaneous adverse reactions and their severity for proper management and potential need to withdraw the offending medication.







Similar content being viewed by others
References
International drug monitoring: the role of national centres. Report of a WHO meeting. World Health Organ. Tech Rep Ser. 1972;498:1–25.
Mockenhaupt M. Epidemiology of cutaneous adverse drug reactions. Chem Immunol Allergy. 2012;97:1–17.
Ahmed AM, Pritchard S, Reichenberg J. A review of cutaneous drug eruptions. Clin Geriatr Med. 2013;29:527–45.
Turk BG, Gunaydin A, Ertam I, Ozturk G. Adverse cutaneous drug reactions among hospitalized patients: five year surveillance. Cutan Ocul Toxicol. 2013;32:41–5.
Svensson CK, Cowen EW, Gaspari AA. Cutaneous drug reactions. Pharmacol Rev. 2001;53:357–79.
Bork K. Cutaneous adverse drug reactions. In: Burgdorf W, Plewig G, Wolff H, Landthaler M, editors. Braun-Falcos dermatol. 3rd ed. Heidelberg: Springer; 2009. p. 456–72.
Johansson SGO, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: report of the nomenclature review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004;113:832–6.
Roujeau JC, Kelly JP, Naldi L, Rzany B, Stern RS, Anderson T, et al. Medication use and the risk of Stevens–Johnson syndrome or toxic epidermal necrolysis. N Engl J Med. 1995;333:1600–7.
Borlongan CV, Burns J, Tajiri N, Stahl CE, Weinbren NL, Shojo H, et al. Epidemiological survey-based formulae to approximate incidence and prevalence of neurological disorders in the United States: a meta-analysis. PloS One. 2013;8:e78490.
Hirtz D, Thurman DJ, Gwinn-Hardy K, Mohamed M, Chaudhuri AR, Zalutsky R. How common are the “common” neurologic disorders? Neurology. 2007;68:326–37.
Tarazona MJ, Mota AN, Gripp AC, Unterstell N, Bressan AL. Bullous pemphigoid and neurological disease: statistics from a dermatology service. An Bras Dermatol. 2015;90:280–2.
Chen YJ, Wu CY, Lin MW, Chen TJ, Liao KK, Chen YC, et al. Comorbidity profiles among patients with bullous pemphigoid: a nationwide population-based study. Br J Dermatol. 2011;165:593–9.
Langan SM, Groves RW, West J. The relationship between neurological disease and bullous pemphigoid: a population-based case-control study. J Invest Dermatol. 2011;131:631–6.
Chosidow O, Doppler V, Bensimon G, Joly P, Salachas F, Lacomblez L, et al. Bullous pemphigoid and amyotrophic lateral sclerosis: a new clue for understanding the bullous disease? Arch Dermatol. 2000;136:521–4.
Birks J, Harvey RJ. Donepezil for dementia due to Alzheimer’s disease. Cochrane Database Syst Rev. 2006;(1):CD001190. doi:10.1002/14651858.CD001190.pub2.
Bryant CA, Ouldred E, Jackson SHD, Kinirons MT. Purpuric rash with donepezil treatment. Br Med J. 1998;19:787.
Rogers SL, Friedhoff LT. The efficacy and safety of donepezil in patients with Alzheimer’s disease: results of a US multicentre, randomized, double-blind, placebo-controlled trial. The Donepezil Study Group. Dement Basel Switz. 1996;7:293–303.
Jones RW. A review comparing the safety and tolerability of memantine with the acetylcholinesterase inhibitors. Int J Geriatr Psychiatry. 2010;25:547–53.
Darreh-Shori T, Jelic V. Safety and tolerability of transdermal and oral rivastigmine in Alzheimer’s disease and Parkinson’s disease dementia. Expert Opin Drug Saf. 2010;9:167–76.
Golüke NMS, van Strien AM, Dautzenberg PJL, Jessurun N, Keijsers CJPW. Skin lesions after oral acetylcholinesterase inhibitor therapy: a case report. J Am Geriatr Soc. 2014;62:2012–3.
Makris M, Koulouris S, Koti I, Aggelides X, Kalogeromitros D. Maculopapular eruption to rivastigmine’s transdermal patch application and successful oral desensitization. Allergy. 2010;65:925–6.
Grieco T, Rossi M, Faina V, De Marco I, Pigatto P, Calvieri S. An atypical cutaneous reaction to rivastigmine transdermal patch. J Allergy. 2011;2011:1–2.
Allain-Veyrac G, Lebreton A, Collonnier C, Jolliet P. First case of symmetric drug-related intertriginous and flexural exanthema (sdrife) due to rivastigmine? Am J Clin Dermatol. 2011;12:210–3.
McShane R, Areosa Sastre A, Minakaran N. Memantine for dementia. Cochrane Database Syst Rev. 2006;(2):CD003154. doi:10.1002/14651858.CD003154.pub5.
Grossberg GT, Manes F, Allegri RF, Gutiérrez-Robledo LM, Gloger S, Xie L, et al. The safety, tolerability, and efficacy of once-daily memantine (28 mg): a multinational, randomized, double-blind, placebo-controlled trial in patients with moderate-to-severe alzheimer’s disease taking cholinesterase inhibitors. CNS Drugs. 2013;27:469–78.
Miller RG, Mitchell JD, Moore DH. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database Syst Rev. 2012;(3):CD001447. doi:10.1002/14651858.CD001447.pub3.
Sorenson EJ. An acute, life-threatening, hypersensitivity reaction to riluzole. Neurology. 2006;67:2260–1.
Błaszczyk B, Lasoń W, Czuczwar SJ. Antiepileptic drugs and adverse skin reactions: an update. Pharmacol Rep. 2015;67:426–34.
Arif H, Buchsbaum R, Weintraub D, Koyfman S, Salas-Humara C, Bazil CW, et al. Comparison and predictors of rash associated with 15 antiepileptic drugs. Neurology. 2007;68:1701–9.
Błaszczyk B, Szpringer M, Czuczwar SJ, Lasoń W. Single centre 20 year survey of antiepileptic drug-induced hypersensitivity reactions. Pharmacol Rep PR. 2013;65:399–409.
Alvestad S, Lydersen S, Brodtkorb E. Rash from antiepileptic drugs: influence by gender, age, and learning disability. Epilepsia. 2007;48:1360–5.
Perucca P, Gilliam FG. Adverse effects of antiepileptic drugs. Lancet Neurol. 2012;11:792–802.
Shear N, Knowles S, Sullivan J. Cutaneous reactions to drugs. In: Freedburg I, Eisen A, Wolff K, editors. Fitzpatrick’s dermatology in general medicine. 6th ed. New York: McGraw-Hill; 2003. p. 1330-7.
Yawalkar N. Drug-induced exanthems. Toxicology. 2005;209:131–4.
McKenna JK, Leiferman KM. Dermatologic drug reactions. Immunol Allergy Clin North Am. 2004;24:399–423 (vi).
Chan HL, Stern RS, Arndt KA, Langlois J, Jick SS, Jick H, et al. The incidence of erythema multiforme, Stevens–Johnson syndrome, and toxic epidermal necrolysis. A population-based study with particular reference to reactions caused by drugs among outpatients. Arch Dermatol. 1990;126:43–7.
Mockenhaupt M. Severe drug-induced skin reactions: clinical pattern, diagnostics and therapy. J Dtsch Dermatol Ges J Ger Soc Dermatol JDDG. 2009;7:142–60 (quiz 161–2).
Barvaliya M, Sanmukhani J, Patel T, Paliwal N, Shah H, Tripathi C. Drug-induced Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and SJS-TEN overlap: a multicentric retrospective study. J Postgrad Med. 2011;57:115–9.
Valeyrie-Allanore L, Sassolas B, Roujeau J-C. Drug-induced skin, nail and hair disorders. Drug Saf. 2007;30:1011–30.
Yang C-Y, Dao R-L, Lee T-J, Lu C-W, Yang C-H, Hung S-I, et al. Severe cutaneous adverse reactions to antiepileptic drugs in Asians. Neurology. 2011;77:2025–33.
Di Pascuale MA, Espana EM, Liu DT-S, Kawakita T, Li W, Gao YY, et al. Correlation of corneal complications with eyelid cicatricial pathologies in patients with Stevens–Johnson syndrome and toxic epidermal necrolysis syndrome. Ophthalmology. 2005;112:904–12.
Sharma VK, Sethuraman G. Adverse cutaneous reactions to drugs: an overview. J Postgrad Med. 1996;42:15–22.
Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: part I. Clinical perspectives. J Am Acad Dermatol. 2013;68:693.e1–14 (quiz 706–8).
Kardaun SH, Sekula P, Valeyrie-Allanore L, Liss Y, Chu CY, Creamer D, et al. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169:1071–80.
Schlienger RG, Shear NH. Antiepileptic drug hypersensitivity syndrome. Epilepsia. 1998;39(Suppl 7):S3–7.
Wong IC, Mawer GE, Sander JW. Factors influencing the incidence of lamotrigine-related skin rash. Ann Pharmacother. 1999;33:1037–42.
Roquin G, Peres M, Lerolle N, Dib N, Mercat A, Croue A, et al. First report of lamotrigine-induced drug rash with eosinophilia and systemic symptoms syndrome with pancreatitis. Ann Pharmacother. 2010;44:1998–2000.
Hebert AA, Ralston JP. Cutaneous reactions to anticonvulsant medications. J Clin Psychiatry. 2001;62(Suppl 14):22–6.
Arroyo S, Sander JW. Carbamazepine in comparative trials: pharmacokinetic characteristics too often forgotten. Neurology. 1999;53:1170–4.
Chopra S, Levell NJ, Cowley G, Gilkes JJ. Systemic corticosteroids in the phenytoin hypersensitivity syndrome. Br J Dermatol. 1996;134:1109–12.
Lafzi A, Farahani RMZ, Shoja MAM. Phenobarbital-induced gingival hyperplasia. J Contemp Dent Pract. 2007;8:50–6.
Levy R, Mattson R, Meldrum B, Perucca E. Antiepileptic drugs. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2002.
Jones RT, Evans W, Mersfelder TL, Kavanaugh K. Rare red rashes: a case report of levetiracetam-induced cutaneous reaction and review of the literature. Am J Ther. 2014. doi:10.1097/MJT.0000000000000105.
Duong TA, Haddad C, Valeyrie-Allanore L, Sbidian E, Chosidow O, Wolkenstein P. Levetiracetam: a possible new inducer of toxic epidermal necrolysis and Stevens–Johnson syndrome in 2 cases. JAMA Dermatol. 2013;149:113–5.
Zou L-P, Ding C-H, Song Z-J, Li X-F. Stevens–Johnson syndrome induced by levetiracetam. Seizure. 2012;21:823–5.
Yesilova Y, Turan E, Sonmez A, Ozardali I. A case of erythema multiforme developing after levetiracetam therapy. Dermatol Online J. 2013;19:12.
Beswick TC, Cohen JB. Dose-related levetiracetam-induced reticulated drug eruption. J Drugs Dermatol JDD. 2010;9:409–10.
Gómez-Zorrilla S, Ferraz AV, Pedrós C, Lemus M, Peña C. Levetiracetam-induced drug reaction with eosinophilia and systemic symptoms syndrome. Ann Pharmacother. 2012;46:e20.
Cerminara C, Seri S, Bombardieri R, Pinci M, Curatolo P. Hypohidrosis during topiramate treatment: a rare and reversible side effect. Pediatr Neurol. 2006;34:392–4.
Guglani L, Sitwat B, Lower D, Kurland G, Weiner DJ. Elevated sweat chloride concentration in children without cystic fibrosis who are receiving topiramate therapy. Pediatr Pulmonol. 2012;47:429–33.
Castela E, Thomas P, Bronsard V, Lacour J-P, Ortonne J-P, Passeron T. Blue pseudochromhidrosis secondary to topiramate treatment. Acta Derm Venereol. 2009;89:538–9.
Aggarwal A, Kumar R, Sharma RC, Sharma DD. Topiramate induced pruritus in a patient with alcohol dependence. Indian J Dermatol. 2011;56:421–2.
Ochoa JG. Pruritus, a rare but troublesome adverse reaction of topiramate. Seizure. 2003;12:516–8.
Scheinfeld N, Spahn C. Palmar erythema due to topiramate. J Drugs Dermatol JDD. 2004;3:321–2.
Chen Y-C, Chu C-Y, Hsiao C-H. Oxcarbazepine-induced Stevens–Johnson syndrome in a patient with HLA-B*1502 genotype. J Eur Acad Dermatol Venereol JEADV. 2009;23:702–3.
Cornell SL, DiBlasi D, Arora NS. drug reaction with eosinophilia and systemic symptoms: DRESS following initiation of oxcarbazepine with elevated human herpesvirus-6 titer. Case Rep Dermatol Med. 2014;2014:853281.
He N, Min F-L, Shi Y-W, Guo J, Liu X-R, Li B-M, et al. Cutaneous reactions induced by oxcarbazepine in Southern Han Chinese: incidence, features, risk factors and relation to HLA-B alleles. Seizure. 2012;21:614–8.
Massot A, Gimenez-Arnau A. Cutaneous adverse drug reaction type erythema multiforme major induced by eslicarbazepine. J Pharmacol Pharmacother. 2014;5:271–4.
Baulac M, Patten A, Giorgi L. Long-term safety and efficacy of zonisamide versus carbamazepine monotherapy for treatment of partial seizures in adults with newly diagnosed epilepsy: results of a phase III, randomized, double-blind study. Epilepsia. 2014;55:1534–43.
Okumura A, Ishihara N, Kato T, Hayakawa F, Kuno K, Watanabe K. Predictive value of acetylcholine stimulation testing for oligohidrosis caused by zonisamide. Pediatr Neurol. 2000;23:59–61.
Knudsen JF, Thambi LR, Kapcala LP, Racoosin JA. Oligohydrosis and fever in pediatric patients treated with zonisamide. Pediatr Neurol. 2003;28:184–9.
Low PA, James S, Peschel T, Leong R, Rothstein A. Zonisamide and associated oligohidrosis and hyperthermia. Epilepsy Res. 2004;62:27–34.
Kaliyadan F, Manoj J, Venkitakrishnan S. Xerosis and pityriasis alba-like changes associated with zonisamide. Indian J Dermatol Venereol Leprol. 2008;74:165–6.
Shibuya R, Tanizaki H, Nakajima S, Koyanagi I, Kataoka TR, Miyachi Y, et al. DIHS/DRESS with remarkable eosinophilic pneumonia caused by zonisamide. Acta Derm Venereol. 2015;95:229–30.
Uhara H, Saiki M, Kawachi S, Ashida A, Oguchi S, Okuyama R. Clinical course of drug-induced hypersensitivity syndrome treated without systemic corticosteroids. J Eur Acad Dermatol Venereol JEADV. 2013;27:722–6.
Tohyama M, Hashimoto K, Yasukawa M, Kimura H, Horikawa T, Nakajima K, et al. Association of human herpesvirus 6 reactivation with the flaring and severity of drug-induced hypersensitivity syndrome. Br J Dermatol. 2007;157:934–40.
Murata T, Endo Y, Katoh M, Miyachi Y, Kabashima K. Case of drug rash with eosinophilia and systemic symptoms induced by zonisamide and reactivation of human herpes virus 7. J Dermatol. 2011;38:918–20.
Fujita Y, Hasegawa M, Nabeshima K, Tomita M, Murakami K, Nakai S, et al. Acute kidney injury caused by zonisamide-induced hypersensitivity syndrome. Intern Med Tokyo Jpn. 2010;49:409–13.
Neuman MG, Shear NH, Malkiewicz IM, Kessas M, Lee AW, Cohen L. Predicting possible zonisamide hypersensitivity syndrome. Exp Dermatol. 2008;17:1045–51.
Teraki Y, Murota H, Izaki S. Toxic epidermal necrolysis due to zonisamide associated with reactivation of human herpesvirus 6. Arch Dermatol. 2008;144:232–5.
Kaniwa N, Sugiyama E, Saito Y, Kurose K, Maekawa K, Hasegawa R, et al. Specific HLA types are associated with antiepileptic drug-induced Stevens–Johnson syndrome and toxic epidermal necrolysis in Japanese subjects. Pharmacogenomics. 2013;14:1821–31.
Biton V, Gil-Nagel A, Isojarvi J, Doty P, Hebert D, Fountain NB. Safety and tolerability of lacosamide as adjunctive therapy for adults with partial-onset seizures: Analysis of data pooled from three randomized, double-blind, placebo-controlled clinical trials. Epilepsy Behav EB. 2015;52:119–27.
Koubeissi MZ, Vismer M, Ehrlich A. Lacosamide-induced rash. Epileptic Disord Int Epilepsy J Videotape. 2014;16:380–3.
Yapici AK, Fidanci MK, Kilic S, Balamtekin N, Mutluay Arslan M, Yavuz ST, et al. Stevens–Johnson Syndrome triggered by a combination of clobazam, lamotrigine and valproic acid in a 7-year-old child. Ann Burns Fire Disasters. 2014;27:121–5.
Dang CD, Beets-Shay L, Kahn EC. Toxic epidermal necrolysis triggered by clobazam: a case report in a 13-year-old girl. Pediatr Dermatol. 2015;32:e102–3.
Redondo P, Vicente J, España A, Subira ML, De Felipe I, Quintanilla E. Photo-induced toxic epidermal necrolysis caused by clobazam. Br J Dermatol. 1996;135:999–1002.
Setterfield JF, Robinson R, MacDonald D, Calonje E. Coma-induced bullae and sweat gland necrosis following clobazam. Clinical dermatology. Concise report. Clin Exp Dermatol. 2000;25:215–8.
Amichai B, Grunwald MH. Erythema multiforme due to clonazepam—supportive evidence from the macrophage migration inhibition factor test. Clin Exp Dermatol. 1998;23:206–7.
Lee M-C, Su C-P, Wang C-H, Lan C-C, Wu T-W. Suspected clonazepam-induced bullous dermatosis in a patient with respiratory failure. J Clin Pharmacol. 2012;52:1607–9.
Gordon KB, Guitart J, Kuzel T, Salard D, Bakouche O, Domer P, et al. Pseudo-mycosis fungoides in a patient taking clonazepam and fluoxetine. J Am Acad Dermatol. 1996;34:304–6.
Munoli RN, Praharaj SK, Bhatt SM. Localized exfoliating rash with paresthesia possibly due to clonazepam. J Child Adolesc Psychopharmacol. 2012;22:320–1.
Schmidt D, Gram L, Brodie M, Krämer G, Perucca E, Kälviäinen R, et al. Tiagabine in the treatment of epilepsy—a clinical review with a guide for the prescribing physician. Epilepsy Res. 2000;41:245–51.
Bauer J, Cooper-Mahkorn D. Tiagabine: efficacy and safety in partial seizures—current status. Neuropsychiatr Dis Treat. 2008;4:731–6.
Adkins JC, Noble S. Tiagabine. A review of its pharmacodynamic and pharmacokinetic properties and therapeutic potential in the management of epilepsy. Drugs. 1998;55:437–60.
Iorio ML, Moretti U, Colcera S, Magro L, Meneghelli I, Motola D, et al. Use and safety profile of antiepileptic drugs in Italy. Eur J Clin Pharmacol. 2007;63:409–15.
Xiao Y, Gan L, Wang J, Luo M, Luo H. Vigabatrin versus carbamazepine monotherapy for epilepsy. Cochrane Database Syst Rev. 2015;11:CD008781.
Kälviäinen R, Aikiä M, Saukkonen AM, Mervaala E, Riekkinen PJ. Vigabatrin vs carbamazepine monotherapy in patients with newly diagnosed epilepsy. A randomized, controlled study. Arch Neurol. 1995;52:989–96.
Chadwick D. Safety and efficacy of vigabatrin and carbamazepine in newly diagnosed epilepsy: a multicentre randomised double-blind study. Vigabatrin European Monotherapy Study Group. Lancet Lond Engl. 1999;354:13–9.
Zaccara G, Gangemi P, Perucca P, Specchio L. The adverse event profile of pregabalin: a systematic review and meta-analysis of randomized controlled trials. Epilepsia. 2011;52:826–36.
Smith TL, Baldwin A, Cunningham LL, Cook AM. Rash associated with pregabalin use. Ann Pharmacother. 2008;42:1899–902.
Bamanikar A, Dhobale S, Lokwani S. Pregabalin hypersensitivity in a patient treated for postherpetic neuralgia. Indian J Pharmacol. 2013;45:522–3.
Wilton LV, Shakir S. A postmarketing surveillance study of gabapentin as add-on therapy for 3,100 patients in England. Epilepsia. 2002;43:983–92.
Lopez PR, Rachael T, Leicht S, Smalligan RD. Gabapentin-induced delusions of parasitosis. South Med J. 2010;103:711–2.
Gijsen VMGJ, de Wildt SN, Ito S. Probability of rash related to gabapentin therapy in a child. Ann Pharmacother. 2009;43:387–9.
Ragucci MV, Cohen JM. Gabapentin-induced hypersensitivity syndrome. Clin Neuropharmacol. 2001;24:103–5.
Sahin S, Comert A, Akin O, Ayalp S, Karsidag S. Cutaneous drug eruptions by current antiepileptics: case reports and alternative treatment options. Clin Neuropharmacol. 2008;31:93–6.
Wollina U, Koch A, Krönert C, Köstler E. Gabapentin-induced generalized cutaneous small-vessel leukocytoclastic vasculitis. Int J Low Extrem Wounds. 2004;3:123–4.
Poon DYH, Law NM. A case of cutaneous leukocytoclastic vasculitis associated with gabapentin. Singap Med J. 2003;44:42–4.
DeToledo JC, Minagar A, Lowe MR, Ramsay RE. Skin eruption with gabapentin in a patient with repeated AED-induced Stevens–Johnson’s syndrome. Ther Drug Monit. 1999;21:137–8.
Schulze-Bonhage A, Hintz M. Perampanel in the management of partial-onset seizures: a review of safety, efficacy, and patient acceptability. Patient Prefer Adherence. 2015;9:1143–51.
Shimabukuro K, Gibbon F, Kerstetter J, Tinsley C, Ashwal S. DRESS associated with perampanel administration in a child with drug-resistant epilepsy. Neurology. 2014;83:2188.
Clark S, Antell A, Kaufman K. New antiepileptic medication linked to blue discoloration of the skin and eyes. Ther Adv Drug Saf. 2015;6:15–9.
Garin Shkolnik T, Feuerman H, Didkovsky E, Kaplan I, Bergman R, Pavlovsky L, et al. Blue-gray mucocutaneous discoloration: a new adverse effect of ezogabine. JAMA Dermatol. 2014;150:984–9.
Shahbaz S, Sivamani RK, Konia T, Burrall B. A case of Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) related to rufinamide. Dermatol Online J. 2013;19:4.
Chambel M, Mascarenhas MI, Regala J, Gouveia C, Prates S. Clinical Stevens–Johnson syndrome and rufinamide: a clinical case. Allergol Immunopathol (Madr). 2013;41:68–9.
Ide M, Kato T, Nakata M, Saito K, Yoshida T, Awaya T, et al. A granulocytosis associated with rufinamide: a case report. Brain Dev. 2015;37:825–8.
Shen V, Clarence-Smith K, Hunter C, Jankovic J. Safety and efficacy of tetrabenazine and use of concomitant medications during long-term, open-label treatment of chorea associated with huntington’s and other diseases. Tremor Hyperkinetic Mov. 2013;3. doi:10.7916/D8BK1B2D.
Fasano A, Cadeddu F, Guidubaldi A, Piano C, Soleti F, Zinzi P, et al. The long-term effect of tetrabenazine in the management of Huntington disease. Clin Neuropharmacol. 2008;31:313–8.
Olesen J, Steiner TJ. The International classification of headache disorders, 2nd edn (ICDH-II). J Neurol Neurosurg Psychiatry. 2004;75:808–11.
Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the american headache society evidence assessment of migraine pharmacotherapies. Headache. 2015;55:3–20.
Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF. Migraine diagnosis and treatment: results from the American Migraine Study II. Headache. 2001;41:638–45.
Siegel SJ, O’Neill C, Dubé LM, Kaldeway P, Morris R, Jackson D, et al. A unique iontophoretic patch for optimal transdermal delivery of sumatriptan. Pharm Res. 2007;24:1919–26.
Goldstein J, Smith TR, Pugach N, Griesser J, Sebree T, Pierce M. A sumatriptan iontophoretic transdermal system for the acute treatment of migraine. Headache. 2012;52:1402–10.
Merck Sharp & Dohme Corp. A randomized, placebo-controlled, parallel-groups, outpatient study to examine the safety, tolerability, and efficacy of single oral doses of MK0462 5 mg, MK0462 10 mg, and Sumatriptan 100 mg for acute treatment of migraine. In: ClinicalTrials.gov [Internet]. Bethesda: National Library of Medicine (US); Available from: https://clinicaltrials.gov/ct2/show/study/NCT00898677. Accessed 20 Aug 2015.
Sanford M. Frovatriptan: a review of its use in the acute treatment of migraine. CNS Drugs. 2012;26:791–811.
Silberstein SD, Kori SH. Dihydroergotamine: a review of formulation approaches for the acute treatment of migraine. CNS Drugs. 2013;27:385–94.
Drago F, Cogorno L, Agnoletti AF, Ciccarese G, Parodi A. A retrospective study of cutaneous drug reactions in an outpatient population. Pharm: Int. J. Clin; 2015.
Grando LR, Schmitt TAB, Bakos RM. Severe cutaneous reactions to drugs in the setting of a general hospital. An Bras Dermatol. 2014;89:758–62.
Ward KE, Archambault R, Mersfelder TL. Severe adverse skin reactions to nonsteroidal antiinflammatory drugs: a review of the literature. Am J Health Syst Pharm. 2010;67:206–13.
Freitag FG, Shumate D. Current and investigational drugs for the prevention of migraine in adults and children. CNS Drugs. 2014;28:921–7.
Halevy S, Feuerman EJ. Psoriasiform eruption induced by propranolol. Cutis. 1979;24:95–8.
Jensen HA, Mikkelsen HI, Wadskov S, Sondergaard J. Cutaneous reactions to propranolol (Inderal). Acta Med Scand. 1976;199:363–7.
Neumann HA, van Joost T. Adverse reactions of the skin to metoprolol and other beta-adrenoreceptor-blocking agents. Dermatologica. 1981;162:330–5.
Sondergaard J, Wadskov S, Jensen HA, Mikkelsen HI. Aggravation of psoriasis and occurrence of psoriasiform cutaneous eruptions induced by practolol (Eraldin). Acta Derm Venereol. 1976;56:239–43.
Heng MC, Heng MK. Beta-adrenoceptor antagonist-induced psoriasiform eruption. Clinical and pathogenetic aspects. Int J Dermatol. 1988;27:619–27.
Halevy S, Livni E. Psoriasis and psoriasiform eruptions associated with propranolol—the role of an immunological mechanism. Arch Dermatol Res. 1991;283:472–3.
Gold MH, Holy AK, Roenigk HH. Beta-blocking drugs and psoriasis. A review of cutaneous side effects and retrospective analysis of their effects on psoriasis. J Am Acad Dermatol. 1988;19:837–41.
Stanford CW, Kollipara R, Melookaran AM, Hall JC. Palmoplantar pustular psoriasis following initiation of a beta-blocker: disease control with low-dose methotrexate. Cutis. 2014;94:153–5.
Perry A, Sparling JD, Pennington M. Bullous pemphigoid following therapy with an oral beta-blocker. J Drugs Dermatol JDD. 2005;4:746–8.
Stage AH, Humeniuk JM, Easley WK. Bullous pemphigoid of the vulva: a case report. Am J Obstet Gynecol. 1984;150:169–70.
Bajwa ZH, Sami N, Flory C. Severe acne as a side effect of propranolol and nadolol in a migraineur. Headache. 1999;39:758–60.
Szok D, Csáti A, Vécsei L, Tajti J. Treatment of chronic migraine with onabotulinumtoxinA: mode of action. Efficacy and safety. Toxins. 2015;7:2659–73.
Brin MF, Boodhoo TI, Pogoda JM, James LM, Demos G, Terashima Y, et al. Safety and tolerability of onabotulinumtoxinA in the treatment of facial lines: a meta-analysis of individual patient data from global clinical registration studies in 1678 participants. J Am Acad Dermatol. 2009;61(961–70):e1–11.
Mezaki T, Sakai R. Botulinum toxin and skin rash reaction. Mov Disord. 2005;20:770.
Roehm PC, Perry JD, Girkin CA, Miller NR. Prevalence of periocular depigmentation after repeated botulinum toxin A injections in African American patients. J Neuro Ophthalmol. 1999;19:7–9.
Khan TT, Herne K, Dayan SH, Woodward JA. Facial blanching due to neurotoxins: proposed mechanisms. Dermatol Surg. 2013;39:24–9.
Gadient PM, Smith JH, Ryan SJ. Herpes zoster ophthalmicus following onabotulinumtoxinA administration for chronic migraine: a case report and literature review. Cephalalgia Int J Headache. 2015;35:443–8.
Graber EM, Dover JS, Arndt KA. Two cases of herpes zoster appearing after botulinum toxin type a injections. J Clin Aesthetic Dermatol. 2011;4:49–51.
Frohman EM, Racke MK, Raine CS. Multiple sclerosis—the plaque and its pathogenesis. N Engl J Med. 2006;354:942–55.
Compston A, Coles A. Multiple sclerosis. Lancet Lond Engl. 2008;372:1502–17.
Brinkmann V, Billich A, Baumruker T, Heining P, Schmouder R, Francis G, et al. Fingolimod (FTY720): discovery and development of an oral drug to treat multiple sclerosis. Nat Rev Drug Discov. 2010;9:883–97.
Costello K, Halper J, Kalb R, Skutnik L, Rapp R. The use of disease-modifying therapies in multiple sclerosis: principles and current evidence. A consensus paper by the multiple sclerosis coalition. Mult Scler Coalit. 2015;1–37.
Balak DMW, Hengstman GJD, Hajdarbegovic E, van den Brule RJP, Hupperts RMM, Thio HB. Prevalence of cutaneous adverse events associated with long-term disease-modifying therapy and their impact on health-related quality of life in patients with multiple sclerosis: a cross-sectional study. BMC Neurol. 2013;13:146.
Balak DMW, Hengstman GJD, Çakmak A, Thio HB. Cutaneous adverse events associated with disease-modifying treatment in multiple sclerosis: a systematic review. Mult Scler. 2012;18:1705–17.
Mancardi GL, Murialdo A, Drago F, Brusati C, Croce R, Inglese M, et al. Localized lipoatrophy after prolonged treatment with copolymer 1. J Neurol. 2000;247:220–1.
Edgar CM, Brunet DG, Fenton P, McBride EV, Green P. Lipoatrophy in patients with multiple sclerosis on glatiramer acetate. Can J Neurol Sci. 2004;31:58–63.
Ball NJ, Cowan BJ, Moore GRW, Hashimoto SA. Lobular panniculitis at the site of glatiramer acetate injections for the treatment of relapsing-remitting multiple sclerosis. A report of two cases. J Cutan Pathol. 2008;35:407–10.
Webster GF, Knobler RL, Lublin FD, Kramer EM, Hochman LR. Cutaneous ulcerations and pustular psoriasis flare caused by recombinant interferon beta injections in patients with multiple sclerosis. J Am Acad Dermatol. 1996;34:365–7.
Elgart GW, Sheremata W, Ahn YS. Cutaneous reactions to recombinant human interferon beta-1b: the clinical and histologic spectrum. J Am Acad Dermatol. 1997;37:553–8.
Ozden MG, Erel A, Erdem O, Oztas MO. Dermal fibrosis and cutaneous necrosis after recombinant interferon-beta1a injection in a multiple sclerosis patient. J Eur Acad Dermatol Venereol JEADV. 2005;19:112–3.
Casoni F, Merelli E, Bedin R, Martella A, Cesinaro A, Bertolotto A. Necrotizing skin lesions and NABs development in a multiple sclerosis patient treated with IFNbeta 1b. Mult Scler. 2003;9:420–3.
Yang C-H, Chen CH, Chan H-L. Skin necrosis following a recombinant interferon-beta-1b injection. Chang Gung Med J. 2002;25:774–7.
García-F-Villalta M, Daudén E, Sánchez J, Fraga J, Ramo C, García-Díez A. Local reactions associated with subcutaneous injections of both beta-interferon 1a and 1b. Acta Derm Venereol. 2001;81:152.
Albani C, Albani G. A case of cutaneous necrosis during interferon-beta 1b (B-IFN) therapy in multiple sclerosis. J Neurol Neurosurg Psychiatry. 1997;62:418.
Créange A, Lefaucheur JP. Focal neuropathy associated with cutaneous necrosis at the site of interferon-beta injection for multiple sclerosis. J Neurol Neurosurg Psychiatry. 2000;68:395.
Sheremata WA, Taylor JR, Elgart GW. Severe necrotizing cutaneous lesions complicating treatment with interferon beta-1b. N Engl J Med. 1995;332:1584.
Ohata U, Hara H, Yoshitake M, Terui T. Cutaneous reactions following subcutaneous beta-interferon-1b injection. J Dermatol. 2010;37:179–81.
Feldmann R, Löw-Weiser H, Duschet P, Gschnait F. Necrotizing cutaneous lesions caused by interferon beta injections in a patient with multiple sclerosis. Dermatol Basel Switz. 1997;195:52–3.
Weinberg JM, Wolfe JT, Sood S, Saruk M, Rook AH, Spiers EM. Cutaneous necrosis associated with recombinant interferon injection. Report of three cases with interferon beta-1b and review of the literature. Acta Derm Venereol. 1997;77:146–8.
Bosca I, Bosca M, Belenguer A, Evole M, Hernandez M, Casanova B, et al. Necrotising cutaneous lesions as a side effect of glatiramer acetate. J Neurol. 2006;253:1370–1.
Koontz D, Alshekhlee A. Embolia cutis medicamentosa following interferon beta injection. Mult Scler. 2007;13:1203–4.
Feldmann R, Schierl M, Rauschka H, Sator P-G, Breier F, Steiner A. Necrotizing skin lesions with involvement of muscle tissue after subcutaneous injection of glatiramer acetate. Eur J Dermatol EJD. 2009;19:385.
Harde V, Schwarz T. Embolia cutis medicamentosa following subcutaneous injection of glatiramer acetate. J Dtsch Dermatol Ges. 2007;5:1122–3.
Gaudez C, Regnier S, Aractingi S, Heinzlef O. Livedo-like dermatitis (Nicolau’s syndrome) after injection of Copolymer-1 (Glatiramer acetate). Rev Neurol (Paris). 2003;159:571–3.
Somani A-K, Swick AR, Cooper KD, McCormick TS. Severe dermatomyositis triggered by interferon beta-1a therapy and associated with enhanced type I interferon signaling. Arch Dermatol. 2008;144:1341–9.
Thouvenot E, Hillaire-Buys D, Bos-Thompson MA, Rigau V, Durand L, Guillot B, et al. Erythema nodosum and glatiramer acetate treatment in relapsing-remitting multiple sclerosis. Mult Scler. 2007;13:941–4.
Kumar N, Rodriguez M. Scleromyxedema in a patient with multiple sclerosis and monoclonal gammopathy on interferon beta-1a. Mult Scler. 2004;10:85–6.
Gono T, Matsuda M, Shimojima Y, Kaneko K, Murata H, Ikeda S. Lupus erythematosus profundus (lupus panniculitis) induced by interferon-beta in a multiple sclerosis patient. J Clin Neurosci. 2007;14:997–1000.
Kocer B, Nazliel B, Oztas M, Batur HZ. Vitiligo and multiple sclerosis in a patient treated with interferon beta-1a: a case report. Eur J Neurol. 2009;16:e78–9.
Nolden S, Casper C, Kuhn A, Petereit HF. Jessner–Kanof lymphocytic infiltration of the skin associated with glatiramer acetate. Mult Scler. 2005;11:245–8.
Bayerl C, Bohland P, Jung EG. Systemic reaction to glatiramer acetate. Contact Dermatitis. 2000;43:62–3.
Rauschka H, Farina C, Sator P, Gudek S, Breier F, Schmidbauer M. Severe anaphylactic reaction to glatiramer acetate with specific IgE. Neurology. 2005;64:1481–2.
Mazzeo L, Ricciardi L, Fazio MC, Fogliani O, Fedele R, Ferlazzo E, et al. Severe urticaria due to recombinant interferon beta-1a. Br J Dermatol. 2003;148:172.
Fusun Kalpaklioglu A, Baccioglu Kavut A, Erdemoglu AK. Desensitization in interferon-beta1a allergy: a case report. Int. Arch Allergy Immunol. 2009;149:178–80.
Guijarro C, Benito-León J, Bermejo-Pareja F. Widespread urticaria due to intramuscular interferon beta-1a therapy for multiple sclerosis. Neurol Sci. 2011;32:309–11.
Brown DL, Login IS, Borish L, Powers PL. An urticarial IgE-mediated reaction to interferon beta-1b. Neurology. 2001;56:1416–7.
Cohen JA, Barkhof F, Comi G, Hartung H-P, Khatri BO, Montalban X, et al. Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N Engl J Med. 2010;362:402–15.
Fruland JE, Sandermann S, Snow SN, Friedl A, Sharata HH. Skin necrosis with subsequent formation of squamous cell carcinoma after subcutaneous interferon beta injection. J Am Acad Dermatol. 1997;37:488–9.
Calabresi PA, Radue E-W, Goodin D, Jeffery D, Rammohan KW, Reder AT, et al. Safety and efficacy of fingolimod in patients with relapsing-remitting multiple sclerosis (FREEDOMS II): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:545–56.
Gasperini C, Ruggieri S, Mancinelli CR, Pozzilli C. Advances in the treatment of relapsing-remitting multiple sclerosis - critical appraisal of fingolimod. Ther Clin Risk Manag. 2013;9:73–85.
Kappos L, Radue E-W, O’Connor P, Polman C, Hohlfeld R, Calabresi P, et al. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N Engl J Med. 2010;362:387–401.
Conzett KB, Kolm I, Jelcic I, Kamarachev J, Dummer R, Braun R, et al. Melanoma occurring during treatment with fingolimod for multiple sclerosis: a case report. Arch Dermatol. 2011;147:991.
Cohen JA, Khatri B, Barkhof F, Comi G, Hartung H-P, Montalban X, et al. Long-term (up to 4.5 years) treatment with fingolimod in multiple sclerosis: results from the extension of the randomised TRANSFORMS study. J Neurol Neurosurg Psychiatry. 2015 (jnnp-2015-310597).
Madray MM, Greene JF, Butler DF. Glatiramer acetate-associated, CD30+, primary, cutaneous, anaplastic large-cell lymphoma. Arch Neurol. 2008;65:1378–9.
Tai YJ, Tam M. Fixed drug eruption with interferon-beta-1b. Australas J Dermatol. 2005;46:154–7.
Serarslan G, Okuyucu E, Melek I, Hakverdi S, Duman T. Widespread maculopapular rash due to intramuscular interferon beta-1a during the treatment of multiple sclerosis. Mult Scler. 2008;14:259–61.
Mehta CL, Tyler RJ, Cripps DJ. Granulomatous dermatitis with focal sarcoidal features associated with recombinant interferon beta-1b injections. J Am Acad Dermatol. 1998;39:1024–8.
Ziegler VR, Kränke B, Soyer P, Aberer W. Extensive cutaneous-subcutaneous infiltration as a side-effect of interferon-beta injection. Hautarzt Z Für Dermatol Venerol Verwandte Geb. 1998;49:310–2.
Macbeth AE, Kendall BR, Smith A, Saldanha G, Harman KE. Calcified subcutaneous nodules: a long-term complication of interferon beta-1a therapy. Br J Dermatol. 2007;157:624–5.
Pacheco MF, Jacobe H, Eagar TN, Stüve O. Reversible alopecia associated with glatiramer acetate. Arch Neurol. 2010;67:1154.
Bar-Or A, Pachner A, Menguy-Vacheron F, Kaplan J, Wiendl H. Teriflunomide and its mechanism of action in multiple sclerosis. Drugs. 2014;74:659–74.
Miller AE, Wolinsky JS, Kappos L, Comi G, Freedman MS, Olsson TP, et al. Oral teriflunomide for patients with a first clinical episode suggestive of multiple sclerosis (TOPIC): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:977–86.
Gerschenfeld G, Servy A, Valeyrie-Allanore L, de Prost N, Cecchini J. Fatal toxic epidermal necrolysis in a patient on teriflunomide treatment for relapsing multiple sclerosis. Mult Scler. 2015;21(11):1476–7.
Xu Z, Zhang F, Sun F, Gu K, Dong S, He D. Dimethyl fumarate for multiple sclerosis. Cochrane Database Syst Rev. 2015;4:CD011076.
Cohen JA, Chun J. Mechanisms of fingolimod’s efficacy and adverse effects in multiple sclerosis. Ann Neurol. 2011;69:759–77.
Jain N, Bhatti MT. Fingolimod-associated macular edema: incidence, detection, and management. Neurology. 2012;78:672–80.
Masera S, Chiavazza C, Mattioda A, Superti G, Beggiato E, Crosasso P, et al. Occurrence of ecchymotic angioedema-like cutaneous lesions as a possible side effect of fingolimod. Mult Scler. 2014;20:1666–7.
Samaraweera AP, Cohen SN, Akay EM, Evangelou N. Lymphomatoid papulosis: a cutaneous lymphoproliferative disorder in a patient on fingolimod for multiple sclerosis. Mult Scler. 2015;22(1):122–4.
Ruck T, Bittner S, Wiendl H, Meuth SG. Alemtuzumab in multiple sclerosis: mechanism of action and beyond. Int J Mol Sci. 2015;16:16414–39.
Cohen JA, Coles AJ, Arnold DL, Confavreux C, Fox EJ, Hartung H-P, et al. Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing-remitting multiple sclerosis: a randomised controlled phase 3 trial. Lancet Lond Engl. 2012;380:1819–28.
Wray S, Arnold DL, Cohen J, Coles A, Fox E, Hartung H. Herpes infection risk reduced with acyclovir prophylaxis after alemtuzumab. In: Poster presented at the 2013 Annual Meeting of the Consortium for Multiple Sclerosis Centers, May 29-June 1, 2013, Orlando, FL. 2013.
Havrdova E, Horakova D, Kovarova I. Alemtuzumab in the treatment of multiple sclerosis: key clinical trial results and considerations for use. Ther Adv Neurol Disord. 2015;8:31–45.
Menge T, Stüve O, Kieseier BC, Hartung H-P. Alemtuzumab: the advantages and challenges of a novel therapy in MS. Neurology. 2014;83:87–97.
Planas R, Martin R, Sospedra M. Long-term safety and efficacy of natalizumab in relapsing-remitting multiple sclerosis: impact on quality of life. Patient Relat Outcome Meas. 2014;5:25–33.
O’Connor P, Goodman A, Kappos L, Lublin F, Polman C, Rudick RA, et al. Long-term safety and effectiveness of natalizumab redosing and treatment in the STRATA MS Study. Neurology. 2014;83:78–86.
Gutwinski S, Erbe S, Münch C, Janke O, Müller U, Haas J. Severe cutaneous Candida infection during natalizumab therapy in multiple sclerosis. Neurology. 2010;74:521–3.
Krumbholz M, Pellkofer H, Gold R, Hoffmann LA, Hohlfeld R, Kümpfel T. Delayed allergic reaction to natalizumab associated with early formation of neutralizing antibodies. Arch Neurol. 2007;64:1331–3.
Cornblath DR, Bienen EJ, Blight AR. The safety profile of dalfampridine extended release in multiple sclerosis clinical trials. Clin Ther. 2012;34:1056–69.
Turnbull K, Caslake R, Macleod AD, Ives N, Stowe R, Counsell C. Monoamine oxidase B inhibitors for early Parkinson's disease. Cochrane Database Syst Rev. 2005;(3):CD004898. doi:10.1002/14651858.CD004898.pub2.
Montastruc JL, Chaumerliac C, Desboeuf K, Manika M, Bagheri H, Rascol O, et al. Adverse drug reactions to selegiline: a review of the French pharmacovigilance database. Clin Neuropharmacol. 2000;23:271–5.
Parkinson Study Group. A controlled trial of rasagiline in early Parkinson disease: the TEMPO Study. Arch Neurol. 2002;59:1937–43.
Parkinson Study Group. A randomized placebo-controlled trial of rasagiline in levodopa-treated patients with Parkinson disease and motor fluctuations: the PRESTO study. Arch Neurol. 2005;62:241–8.
Teva Pharmaceutical Industries Ltd. Azilect(R) package insert. Kfar Saba, Israel: Teva Pharmaceutical Industries Ltd; 2006.
Boehringer Ingelheim International GmbH. Mirapex(R) package insert. Ridgefield: Boehringer Ingelheim International GmbH; 2006.
GlaxoSmithKline. Requip(R) package insert. Research Triangle Park: GlaxoSmithKline; 2005.
Valeant Pharmaceuticals International. Zelapar(R) package insert. Costa Mesa: Valeant Pharmaceuticals International; 2006.
Ferreira JJ, Neutel D, Mestre T, Coelho M, Rosa MM, Rascol O, et al. Skin cancer and Parkinson’s disease. Mov Disord. 2010;25:139–48.
Vermeij J-D, Winogrodzka A, Trip J, Weber WEJ. Parkinson’s disease, levodopa-use and the risk of melanoma. Parkinsonism Relat. Disord. 2009;15:551–3.
Fleischer AB, Resnick SD. Livedo reticularis. Dermatol Clin. 1990;8:347–54.
Gibbs MB, English JC, Zirwas MJ. Livedo reticularis: an update. J Am Acad Dermatol. 2005;52:1009–19.
Strowd LC, Lee AD, Yosipovitch G. Livedo reticularis associated with rasagiline (azilect). J Drugs Dermatol JDD. 2012;11:764–5.
Quaresma MV, Gomes ACD, Serruya A, Vendramini DL, Braga L, Buçard AM. Amantadine-induced livedo reticularis—case report. An Bras Dermatol. 2015;90:745–7.
Singer C, Papapetropoulos S, Gonzalez MA, Roberts EL, Lieberman A. Rimantadine in Parkinson’s disease patients experiencing peripheral adverse effects from amantadine: report of a case series. Mov Disord. 2005;20:873–7.
Vollum DI, Parkes JD, Doyle D. Livedo reticularis during amantadine treatment. Br Med J. 1971;2:627–8.
Sladden MJ, Nicolaou N, Johnston GA, Hutchinson PE. Livedo reticularis induced by amantadine. Br J Dermatol. 2003;149:656–8.
Rana AQ, Masroor MS. Patient perception of Levido reticularis due to amantadine. Int J Neurosci. 2012;122:363–6.
Eggert K, Oertel WH, Lees AJ. German competence network on Parkinson’s disease. Safety and efficacy of tolcapone in the long-term use in Parkinson disease: an observational study. Clin Neuropharmacol. 2014;37:1–5.
Olanow CW, Watkins PB. Tolcapone: an efficacy and safety review (2007). Clin Neuropharmacol. 2007;30:287–94.
Olanow CW, Kieburtz K, Stern M, Watts R, Langston JW, Guarnieri M, et al. Double-blind, placebo-controlled study of entacapone in levodopa-treated patients with stable Parkinson disease. Arch Neurol. 2004;61:1563.
Foti C, Cassano N, De Mari M, Sorino M, Vena GA. Bullous skin eruption associated with entacapone. Int J Dermatol. 2004;43:471–2.
Marsala SZ, Gioulis M, Ceravolo R, Tinazzi M. A systematic review of catechol-O-methyltransferase inhibitors: efficacy and safety in clinical practice. Clin Neuropharmacol. 2012;35:185–90.
Kuoppamäki M, Vahteristo M, Ellmén J, Kieburtz K. Pooled analysis of phase III with entacapone in Parkinson’s disease. Acta Neurol Scand. 2014;130:239–47.
Elahmed HH. Phototoxic rash during therapy with pramipexole in a patient with restless Legs syndrome. Sultan Qaboos Univ Med J. 2013;13:190–1.
Tan EK, Ondo W. Clinical characteristics of pramipexole-induced peripheral edema. Arch Neurol. 2000;57:729–32.
Makumi CW, Asgharian A, Ellis J, Shaikh S, Jimenez T, VanMeter S. Long-term, open-label, safety study of once-daily ropinirole extended/prolonged release in early and advanced Parkinson’s disease. Int J Neurosci. 2016;126(1):30–8.
Fahn S, Oakes D, Shoulson I, Kieburtz K, Rudolph A, Lang A, et al. Levodopa and the progression of Parkinson’s disease. N Engl J Med. 2004;351:2498–508.
Holloway RG, Shoulson I, Fahn S, Kieburtz K, Lang A, Marek K, et al. Pramipexole vs levodopa as initial treatment for Parkinson disease: a 4-year randomized controlled trial. Arch Neurol. 2004;61:1044–53.
Rascol O, Brooks DJ, Korczyn AD, De Deyn PP, Clarke CE, Lang AE. A five-year study of the incidence of dyskinesia in patients with early Parkinson’s disease who were treated with ropinirole or levodopa. N Engl J Med. 2000;342:1484–91.
Goetz CG. Skin rash associated with Sinemet 25/100. N Engl J Med. 1983;309:1387–8.
Chou KL, Stacy MA. Skin rash associated with Sinemet does not equal levodopa allergy. Neurology. 2007;68:1078–9.
Liu R, Gao X, Lu Y, Chen H. Meta-analysis of the relationship between Parkinson disease and melanoma. Neurology. 2011;76:2002–9.
Pioro EP. Review of dextromethorphan 20 mg/quinidine 10 mg (NUEDEXTA®) for Pseudobulbar affect. Neurol Ther. 2014;3:15–28.
Schoedel KA, Morrow SA, Sellers EM. Evaluating the safety and efficacy of dextromethorphan/quinidine in the treatment of pseudobulbar affect. Neuropsychiatr Dis Treat. 2014;10:1161–74.
Cohen IS, Jick H, Cohen SI. Adverse reactions to quinidine in hospitalized patients: findings based on data from the Boston Collaborative Drug Surveillance Program. Prog Cardiovasc Dis. 1977;20:151–63.
Conroy EA, Liranzo MO, McMahon J, Steck WD, Tuthill RJ. Quinidine-induced pigmentation. Cutis. 1996;57:425–7.
Mahler R, Sissons W, Watters K. Pigmentation induced by quinidine therapy. Arch Dermatol. 1986;122:1062–4.
Birek C, Main JH. Two cases of oral pigmentation associated with quinidine therapy. Oral Surg Oral Med Oral Pathol. 1988;66:59–61.
Chang C, Gershwin ME. Drug-induced lupus erythematosus: incidence, management and prevention. Drug Saf. 2011;34:357–74.
Shalit M, Flugelman MY, Harats N, Galun E, Ackerman Z, Kopolovic J, et al. Quinidine-induced vasculitis. Arch Intern Med. 1985;145:2051–2.
Holt RJ. Uncharacteristic cutaneous reactions induced by quinidine. Drug Intell Clin Pharm. 1982;16:615–6.
Adornato MC. Toxic epidermal necrolysis associated with quinidine administration. N Y State Dent J. 2000;66:38–40.
Otero Rivas MM, Sánchez Sambucety P, García-Ruiz de Morales JM, Pérez Paredes G, Rodríguez Prieto MA. Acute generalized exanthematous pustulosis due to dextromethorphan. Dermatol Online J. 2013;19:20030.
Pattee GL, Wymer JP, Lomen-Hoerth C, Appel SH, Formella AE, Pope LE. An open-label multicenter study to assess the safety of dextromethorphan/quinidine in patients with pseudobulbar affect associated with a range of underlying neurological conditions. Curr Med Res Opin. 2014;30:2255–65.
Dodiuk-Gad RP, Chung W-H, Valeyrie-Allanore L, Shear NH. Stevens–Johnson syndrome and toxic epidermal necrolysis: an update. Am J Clin Dermatol. 2015;16(6):475–93.
Bruno TF, Grewal P. Erythroderma: a dermatologic emergency. CJEM. 2009;11:244–6.
Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: part II. Management and therapeutics. J Am Acad Dermatol. 2013;68:709.e1–9 (quiz 718–20).
Szatkowski J, Schwartz RA. Acute generalized exanthematous pustulosis (AGEP): a review and update. J Am Acad Dermatol. 2015;73:843–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used in the preparation of this manuscript.
Conflicts of interest
Eman Bahrani, Chloe E. Nunneley, Sylvia Hsu, and Joseph S. Kass have no financial or other relationships that might lead to a conflict of interest.
Rights and permissions
About this article
Cite this article
Bahrani, E., Nunneley, C.E., Hsu, S. et al. Cutaneous Adverse Effects of Neurologic Medications. CNS Drugs 30, 245–267 (2016). https://doi.org/10.1007/s40263-016-0318-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-016-0318-7