Abstract
Skeletal scintigraphy is one of the most frequent in vivo procedures in the field of nuclear medicine. Visualizing bone metabolism, it exhibits a fairly high sensitivity to detect skeletal lesions, but has limitations in terms of specificity and spatial resolution, even when single-photon emission computed tomography (SPECT) is used. Combining SPECT with X-ray computed tomography helps overcome these limitations. This has, in particular, been shown when diagnosing bone involvement in malignant tumors. Emerging evidence indicates the benefit of hybrid imaging for bone scintigraphy during the workup of painful conditions affecting the back and the extremities. Methodological advances holding considerable promise for further improving its value are the quantitation of skeletal tracer uptake in absolute units, as well as multimodal image reconstruction techniques that have recently become available for use in clinical routine.
Similar content being viewed by others
Introduction
The quantification of bone metabolism was among the first applications of tracers in biology. The letter to Nature published in 1935 by George de Hevesy, which earned him the Nobel Prize in 1943, described the use of radioactive phosphorus to investigate bone metabolism in rats [1]. De Hevesy concluded from his results that “the formation of bones is a dynamic process”, thus laying the foundation for many approaches to the study of bone metabolism that nuclear medicine developed over the following decades.
The 99mTc-labeled polyphosphonates that are used today were introduced approximately 40 years ago [2]. Scintigraphic images acquired early after their intravenous injection provide information on perfusion and floridity of skeletal lesions (for a general review, see [3]). Scintigraphy performed several hours after tracer injection therefore allows insight into bone metabolism or, more specifically, osteoblastic activity, since the polyphosphonates are adsorbed on freshly built bone tissue [4, 5]. Initially, bone scintigrams were planar images, acquired either as spot views or as whole-body images. Due to the sensitivity of this examination to detect osseous lesions, skeletal scintigraphy has been widely used as a screening tool, e.g., for staging malignant disease. In the late 1980s, single-photon emission computed tomography (SPECT) became widely available, allowing three-dimensional visualization of the distribution of radioactivity within the human body. This technology considerably improved the diagnostic accuracy of bone scintigraphy by allowing better localization of areas exhibiting pathological tracer uptake (for a review, see [6]). Nevertheless, due to limitations in the spatial resolution of skeletal SPECT, which ranges from ca. 8 to 10 mm in the reconstructed images, the specificity of skeletal scintigraphy is still limited. This is true particularly when it is compared to radiological techniques such as X-ray computerized tomography (CT) or magnetic resonance imaging (MRI), the latter technique also allowing visualization of soft-tissue structures associated with bone, such as tendons, ligaments and cartilage, that elude bone scintigraphy for obvious methodological reasons.
Approximately 12 years ago, the first hybrid system integrating a SPECT camera with a CT scanner into a single gantry became commercially available (for a review, see [7]). The CT component of this system utilized a low-dose, non-spiral CT scanner, whose images lacked diagnostic quality but allowed fairly precise localization of SPECT foci of abnormal tracer uptake, CT diagnosis of gross morphological abnormalities, and attenuation correction of the SPECT images as well. Since then, these technologies have considerably advanced, with current SPECT/CT systems offering a wide array of diagnostic quality, multislice spiral CT scanners (for review, see [8]).
This article reviews scientific evidence on the utility of SPECT/CT for bone scintigraphy following intravenous injection of Tc-99m-labeled polyphosphonates. As regards its value in imaging osteomyelitis with tracers concentrating in infectious and inflammatory lesions, the reader is referred to the review article specifically covering this topic, published in this issue of Clinical and Translational Imaging [9].
Using the terms SPECT/CT, SPECT-CT and skeletal, we conducted an electronic search of the PubMed database without language restrictions. The list of articles generated was augmented by retrieving further pertinent publications from the reference lists of the papers found in PubMed. Due to heterogeneities in study design, we did not perform meta-analyses or any evidence-based quality assessment of the available evidence.
Technical considerations
The SPECT portion of a SPECT/CT examination is, in principle, no different from SPECT performed using a stand-alone system. For skeletal CT, the intravenous injection of contrast medium is not usually necessary. With the hybrid systems featuring a multislice spiral CT scanner, a CT examination of the skeleton of full diagnostic quality is possible, at least in principle. A literature survey shows, however, that even when such CT scanners are available, low-dose CT protocols with tube current–time products ranging from 15 to 60 mAs are generally used [10]. Furthermore, and contrary to the practice encountered in radiology, in a significant proportion of the studies so far published, the CT field of view is restricted to the region of the body harboring abnormalities of tracer uptake visible on the planar scintigraphic images. With this so-called SPECT-guided low-dose CT, as introduced by Römer et al. [11], the average radiation doses delivered to the patient are reduced between 2 and 3 mSv in most cases and thus correspond to doses incurred by patients having planar radiographs or non-diagnostic CT scans with SPECT/CT cameras not equipped with a spiral CT.
When SPECT/CT is used for staging, the results reported for the SPECT/non-diagnostic CT systems, as well as those obtained using SPECT-guided low-dose CT protocols, do not seem to be inferior to those obtained with the SPECT/diagnostic CT methodology (see below). Direct proof in support of this thesis is, however, lacking. In the case of staging, the major advantage of hybrid imaging resides in its potential to differentiate degenerative from neoplastic tracer-avid lesions in the axial skeleton (see below) where the bones involved are usually quite large and the anatomy less complex than in the peripheral skeleton. Furthermore, hot spots related to joint and spinal degeneration, as opposed to osseous metastases, typically project to the bony interfaces in question; thus, the foci localization capability provided by SPECT/non-diagnostic CT would, in principle, suffice for differential diagnosis. Therefore, the assumption of nearly equivalent performance of non-diagnostic and diagnostic CT protocols when using skeletal SPECT/CT for staging seems plausible.
This may, however, not necessarily be the case when SPECT/CT is performed for the workup of pain occurring in anatomically more complex regions of the body such as the wrists or the feet. Using SPECT/high-resolution flat-panel CT, Lohrmann et al. [12] have indeed demonstrated that diagnostic confidence scores and inter-observer agreement, as well as diagnostic accuracy, are all significantly higher with high-resolution CT images than with low-resolution ones, the latter being generated in their study by filtering the former.
The advantage of SPECT/CT, compared to the side-by-side evaluation of datasets acquired independently of each other, is the possibility of integrating the information from both modalities at pixel level. The average anatomical accuracy of alignment between the two sets of images is usually better than 2 mm in the lumbar spine and 5 mm in the neck and in organs affected by respiration [13, 14]. This error can be further reduced by applying additional image fusion software to the preregistered images. The greater SPECT/CT misalignment encountered in parts of the body subject to respiratory motion is due to the longer acquisition times of SPECT compared to spiral CT which generally captures these body regions in one phase of the respiratory cycle. Contrary to positron emission tomography (PET)/CT, respiratory gating protocols are not yet commercially available for SPECT/CT, rendering routine correction for these artifacts, at the time of writing, unfeasible.
On the basis of CT information, which is directly related to photon tissue absorption, the SPECT images of SPECT/CT can be attenuation corrected to yield a more realistic and homogeneous image of tracer distribution (for reviews, see [15, 16]). In this case, an important prerequisite is, however, that the alignment between CT and SPECT images is well below the SPECT pixel width; otherwise, attenuation artifacts may lead to false interpretation of the images [17].
For image interpretation, both image datasets are displayed simultaneously, with one overlaid on top of the other. As is also the case when interpreting stand-alone SPECT images, care should be taken to standardize SPECT windowing and color tables when assessing the significance of uptake in lesions. CT images should primarily be viewed using a window optimized for bone viewing centered on 500 Hounsfield units (HU) with a window width of 1,500 HU. In order not to miss extraosseous pathology, CT scans should subsequently also be analyzed using windowing similarly optimized for lung and soft-tissue viewing. A SPECT/CT pattern-oriented approach to diagnosis has recently been published [18], providing some guidance on how to integrate the information from both modalities and arrive at a specific diagnosis.
SPECT/CT for staging malignant bone disease
Skeletal lesions most frequently arise as a result of metastatic disease from primary tumors in other organs. Metastatic disease to the skeleton occurs in about 30 % of cancer patients, and identification of bone involvement is mandatory for correct staging and subsequent therapy. Skeletal metastases are frequently amenable to detection by bone scintigraphy with the 99mTc-labeled polyphosphonates, e.g., 99mTc-methylene diphosphonate. This imaging procedure affords visualization of the entire skeleton with an extremely high sensitivity, approaching 100 % for breast and prostate cancer (for reviews, see [6] and [19]). Purely lytic metastases such as those due to renal carcinoma or plasmocytoma may not increase bone metabolism and thus escape diagnosis by bone scintigraphy. This is also the case of sclerotic neoplastic osseous foci after treatment, e.g., with bisphosphonates, which are occasionally difficult to differentiate from bone islands.
The specificity of bone scintigraphy is rather low, as benign conditions, too, may be accompanied by an increase in bone metabolism. Pertinent examples are spinal degenerative conditions such as osteochondrosis and spondyloarthropathy, as well as osteoporotic fractures of the vertebral bodies. They pose a particular problem as they have a very high incidence in elderly subjects—an age group in which malignant disease is common. In addition, benign primary bone tumors such as enchondromas or fibrous dysplasia, as well as inflammatory diseases such as osteomyelitis, may be difficult to differentiate from metastases on the basis of radionuclide bone imaging alone. Its rather low specificity, therefore, often necessitates further investigation with, e.g., planar X-ray radiography, CT or MRI.
In the case of indeterminate bone lesions detected by bone scintigraphy for which a definite diagnosis cannot be reached, SPECT/CT offers the unique opportunity to directly correlate the scintigraphic findings with CT images to improve lesion classification (Fig. 1). Immediately after the introduction of the first hybrid SPECT/CT system in 2006, this advantage was investigated systematically in a trio of studies.
Transaxial SPECT, CT and SPECT/CT fusion images through a lumbar vertebral body from two patients with breast cancer (upper and lower row). The focus of abnormal tracer accumulation in the upper row of images is explained by arthritis of the facet joint, exhibiting joint space narrowing, subchondral sclerosis and osteophytes. In the lower row of images, maximal tracer uptake projects slightly behind the joint space to a region that is less dense than its contralateral counterpart. This constellation points to a small osteolysis in the posterior arch of that vertebral body (color figure online)
Horger et al. [20] studied 47 patients with 104 equivocal lesions on bone scintigraphy, taking histological confirmation or long-term follow-up as the reference gold standard. SPECT/CT allowed correct diagnosis in 85 % of the cases, particularly by improving characterization of the true nature of focal areas in the spine, ribcage, skull and pelvis. The term “SPECT-guided CT” refers to the adaptation of the CT field of view to foci of increased bone metabolism and was introduced by Römer et al. [11]. Using this method in 52 indeterminate lesions in 44 patients, 92 % of abnormal uptake foci visualized by SPECT/CT were correctly classified, with a pronounced benefit for lesions in the spinal column, ribs and pelvis. In addition to the improved diagnostic accuracy obtained by correlating functional with morphological images, Utsunomiya et al. [21] also reported a better diagnostic confidence for fused SPECT/CT image datasets than for side-by-side viewing of images from the two modalities.
Since these three initial reports, at least seven further publications have analyzed the potential of SPECT/CT to elucidate osseous hypermetabolic foci [22–29]. Table 1 gives a rough overview of the characteristics of each of these different studies and the results obtained. Despite various apparent weaknesses in the available evidence, linked to heterogeneities in study design, the results obtained are remarkably consistent: SPECT/CT enables a definitive diagnosis in between 71.0 and 95.3 % of lesions deemed equivocal on planar scintigraphy/SPECT (planar/SPECT) imaging [11, 23–25, 27]. SPECT/CT with bone-seeking radiopharmaceuticals is becoming a cost-effective, standard-of-reference imaging technique in the evaluation of patients with various types of cancer.
Differential diagnosis of pain associated with the musculoskeletal system
Although MRI currently represents the standard of reference for benign orthopedic disease, bone scintigraphy is still frequently used for these indications due to its cost-effectiveness and the high sensitivity to osseous lesions and the complete view of the skeleton it provides. However, aside from its inability to visualize the soft-tissue structures of the joints, its major drawback is its low specificity.
SPECT/CT appears to overcome most of the diagnostic limitations of purely nuclear bone scintigraphy by allowing precise anatomical localization of bone turnover abnormalities. This advantage is also useful in non-oncological diseases (for recent reviews, see [30–34]).
One early retrospective study systematically analyzed the clinical benefit of SPECT/CT in benign orthopedic conditions of various origins pooled from all body regions. These authors investigated data from 89 consecutive non-oncological patients with inconclusive bone scans, for which further correlation with morphological imaging was required [35]. Rather than histological confirmation, consensus opinion between two nuclear medicine physicians and one musculoskeletal radiologist served as a gold standard. In 59 % of the subjects, multislice low-dose CT added to SPECT was critical for diagnosing the lesions as either fractures, osteochondral lesions, non-ossifying fibroma, enchondroma, fibrous dysplasia, herniation pits, spurs, posterior osteophytes, osteoid osteomas, bursitis, osteoarthritis, exostosis, spondylolysis, hemilumbalization or vertebral collapse. In another 30 % of the patients, SPECT/low-dose CT was used to optimize further patient imaging procedures. In the light of these findings, the authors concluded that SPECT/low-dose CT represented a clinically relevant component of the diagnostic process in patients with non-oncological orthopedic conditions referred for bone scintigraphy.
More specific evidence is continuously emerging in support of this conclusion. Below we first review findings regarding painful conditions affecting the axial skeleton and then provide a commentary on those concerning the appendicular skeleton.
Axial skeleton Bisphosphonates are increasingly used to treat lytic bone metastases as they reduce pain, pathological fractures, limited mobility, malignant hypercalcemia and spinal cord compression (for a review, see [36]). Osteonecrosis of the jaw is one of the complications associated with this therapy, particularly when it is given intravenously, and potentially affects up to 6.7 % of patients treated with these drugs. Besides conservative treatment such as antibiotics, operative resection of the necrotic core is usually performed. The diagnosis of this condition is usually based on typical symptoms and the detection of an unexposed extraction socket upon inspection. Imaging helps in differentiating this condition from neoplastic spread or radiation-induced osteonecrosis and in defining the extent of the osteonecrotic core. On bone scintigrams, increased tracer uptake in all three phases is usually seen. With planar and stand-alone SPECT imaging, a clear delineation of the necrotic tissue is not usually feasible, and SPECT/CT is thus an option to serve this purpose. In 2009, Dore et al. [37] assessed the value of this technology in diagnosing osteonecrosis of the jaw associated with intravenous bisphosphonate therapy in a group of 15 patients. They demonstrated that SPECT/CT allowed delineation of the osteonecrotic core, even in the presence of nearby hyperactivity due to viable bone. In their selected group of patients, MRI was unable to visualize bone loss, but proved helpful to detect soft-tissue involvement, suggesting the need for a multimodal approach to this disease including SPECT/CT.
Lower back pain has a very high incidence in western populations and a vast gamut of differential diagnoses (for a review, see [38]). Disk herniation is not amenable to bone scintigraphy and can only be diagnosed by MRI. Active degenerative disease of the axial skeleton, however, being accompanied by an increase in polyphosphonate uptake, is amenable to bone scintigraphy (Fig. 2). This applies to osteochondrosis radiologically characterized by disk space narrowing, subchondral sclerosis of the vertebral bodies, osteophytes, and radiological signs of disk degeneration such as the occurrence of gas in the disk—the so-called vacuum phenomenon. More relevant to clinical management is the detection of active osteoarthritis at facet joints, as this diagnosis and localization helps in directing topical therapies such as a medial branch block or intra-articular instillation of corticosteroids.
Common causes of back pain as seen on CT (left column) and SPECT/CT fusion (right column): upper row Osteochondrosis with gas in the intervertebral disk as a sign of its degeneration (vacuum phenomenon), subchondral sclerosis, and metabolically active osteophytes. Middle row facet arthritis with subchondral sclerosis and osteophytes. Lower row impending compression fracture of a lumbar vertebral body with increased tracer uptake in the end plate and accompanying end plate impression (color figure online)
Active facet joint disease can be diagnosed by SPECT/CT: Matar et al. [39] reported a frequency of 65 % for metabolically active facet joint disease in 72 patients referred for SPECT/CT for workup of chronic neck or back pain. In their retrospective study, SPECT/CT identified potential pain generators in 92 % of the study population. Makki et al. [40] reported that 91.1 % of 486 patients consecutively studied by SPECT/CT for spinal pain over 7.5 years had at least one abnormality visible on SPECT/CT potentially causing the symptoms. In their cohort, they found a prevalence of 42.8 % of subjects with increased uptake in at least one zygapophyseal joint. In a further large retrospective study, Lehmann and coworkers analyzed data from 212 patients referred to their department for spinal SPECT/CT over a period of roughly 4 years [41]. 191 of these subjects had been examined for workup of back pain, with suspicion of abnormal facet joint activity being the most frequent indication (37 % of the total). In 50 % of the whole group, pathological uptake was described in at least one facet joint. Most noteworthy, 40 % of the whole group had undergone SPECT/CT after prior MRI examinations, and 35 % of the subjects referred for differential diagnosis of pain had had prior percutaneous interventions with incomplete response. As recorded on the treating physicians’ clinical notes, SPECT/CT findings led to a change in clinical management in 79 % of patients, a result that impressively documents the level of acceptance and the utility of hybrid SPECT/CT imaging.
The evidence presented above suggests that skeletal SPECT/CT might have the potential to guide percutaneous therapy of facet joint arthritis. Additional data on the use of stand-alone SPECT also point in this direction [42–44]. In a further publication, however, Lehmann et al. [45], in a group of 74 patients, analyzed the relationship between the localization of abnormal tracer uptake in the facet joint and the joint percutaneously treated. In 70 % of these subjects, site of treatment and SPECT/CT abnormality did not coincide. Furthermore, 46 % of the subjects had a right versus left discrepancy. This shows that the relationship between the scintigraphic abnormality and the occurrence of back pain is not as straightforward as initially expected. The type of treatment is also a variable that should receive consideration in this context: in a prospective double-blinded outcome study, Ackerman and Ahmad showed that SPECT/CT performed better in predicting pain relief after intra-articular injections of cortisone than after medial branch blocks [46]. Clearly, more evidence from further prospective—ideally, double-blinded—investigations with pain relief as an outcome variable would be necessary to establish the value of SPECT/CT for planning local therapies of painful facet arthritis.
Another frequent cause of back pain, particularly in the elderly, is osteoporotic compression fracture of vertebral bodies. Within the first year of occurrence, this condition is metabolically active and can thus be visualized by bone scintigraphy. SPECT/CT may help in localization and also in differentiating this condition from metabolically active osteochondrosis. Vertebral osteoporotic fractures may be treated by percutaneous vertebroplasty. In a recently published prospective study of 33 consecutive patients with this condition, positive SPECT/CT images predicted, in 91 % of these subjects, clinical improvement induced by this minimally invasive procedure [47]. Furthermore, it identified alternative causes of pain in the subgroup of nine patients in whom the therapy in question had not been performed. It can be surmised, on the basis of anecdotal evidence, that SPECT/CT might also be helpful in acute spinal traumas and, in particular, in diagnosing stress fractures in bilateral pedicles of the spine, as can occur in athletes [30].
Spinal fusion surgery is performed in patients with severe chronic back pain when segmental instability is believed to be the cause of the symptoms (for review, see [48, 49]). The rationale for this is that pain relief will be achieved once the fusion restricts motion in the painful segments. An estimated ten to twenty percent of patients develop lumbar pain after lumbar fusion surgery. This may be related to loosening of the metallic implants or failure of a stably implanted graft to immobilize the fused segments. A further differential diagnosis is degenerative disease involving the spinal segments above or below the instrumented region. Differentiation between these conditions has therapeutic consequences: in the first case, a complementary ventral spondylodesis must be considered, in the second an amplification of the instrumentation in cranial or caudal direction. Near to metallic implants, CT quality is considerably degraded by streak artifacts and that of MRI by susceptibility phenomena, thus reducing the accuracy of these two modalities in differentiating between the above-described causes of pain after spondylodesis. Bone scintigraphy, which is either not affected by these artifacts or affected only indirectly via attenuation correction, might thus be of particular value for this purpose [50].
Sumer and coworkers compared skeletal SPECT/CT to planar/SPECT imaging in 37 patients suffering from back pain after lumbar fusion surgery [51]. SPECT/CT led to a change in diagnostic category in approximately half of the patients. The superiority of SPECT/CT over planar/SPECT was, however, not due to an increase in the sensitivity of SPECT/CT in detecting pathological foci of uptake compared to standard scintigraphic imaging. Rather, as when staging malignant disease, SPECT/CT improved the specificity of nuclear medical imaging via two avenues: (1) through its ability to localize pathological foci of uptake more precisely, and (2) through its capacity to characterize the CT morphology of the lesions underlying the increase in bone metabolism depicted by scintigraphy. These data suggest that planar/SPECT misses the correct diagnosis in roughly half the patients studied. It follows that they also indicate that, for similar patient cohorts, planar scintigraphy should be complemented by a SPECT/CT examination.
The publication by Sumer et al. lacks a gold standard which, in such cases, could take the form of an intraoperative examination of the stability of the implant in the course of a reoperation. Damgaard et al. [52] performed such a study and indeed showed that this evaluation confirmed the SPECT/CT diagnosis of metal loosening in their sample of nine patients suffering from lower back pain after lumbar instrumentation. Similar data have been published by Rager et al. [53]: in their case series of ten patients, all screws deemed loosened on reoperation had corresponding increased tracer uptake on SPECT/CT. In six cases, metabolic activation was found in facet joints that had no CT abnormality, and in three of five subjects SPECT/CT did not confirm the CT diagnosis of nonunion through or around cages. SPECT/CT thus holds considerable promise in this field and further prospective studies further underscoring its value would be of utmost interest.
Appendicular skeleton A wide array of conditions may lead to pain of the extremities. Imaging workup usually starts with planar radiographs, followed by CT or MRI, depending on the differential diagnoses under consideration by the treating physician. Bone scintigraphy is another option, but in this setting it, too, suffers from the aforementioned low specificity. Therefore, SPECT/CT has received considerable attention for such indications, as highlighted by several pertinent review articles [32, 33].
In a retrospective study, Linke et al. [54] reported 71 non-oncological patients with pain in the extremities who had undergone a conventional three-phase bone scan and SPECT/CT of either the arms (n = 20) or legs (n = 51). Four patients exhibited no abnormal bone metabolism or CT abnormality in the extremities. Of the 34 lesions classified as osteoarthritis on the planar/SPECT images, seven were reclassified as fracture and one as benign tumor by SPECT/CT; of the 15 lesions classified as osteomyelitis, four were diagnosed as osteoarthritis, four as fracture, and one as inflammation of the soft tissue only. Two of eight patients in whom a fracture had been diagnosed by the conventional approach were reclassified as osteomyelitis and two as osteoarthritis. In one of the ten patients diagnosed with a tumor-like lesion, the diagnosis was changed to trauma and in another to osteoarthritis on the basis of SPECT/CT findings. Overall, SPECT/CT led to revision of the diagnostic category in 23/71 patients (32 %; χ 2 = 10.82, p < 0.01).
A multitude of further publications has addressed a range of more specific issues, such as SPECT/CT imaging of the feet and hands. SPECT/CT has been found to show good diagnostic accuracy in patients with obscure pain of the wrist or hand, being able to differentiate between osteoarthritic lesions, occult fractures and osteonecrosis [55–58]. A particularly elegant approach is that of combining SPECT/CT with arthrography, the latter yielding information on the intactness of articular cartilage and other soft-tissue structures such as the scapholunate and lunotriquetral ligaments [59].
Pain in the foot may be due to a plethora of different conditions, including osteoarthritis caused by accessory sesamoid bones, tarsal coalition and osteochondrosis dissecans. In addition, impingement syndromes, inflammation, trauma and soft-tissue pathologies may also give rise to complaints in the distal extremities. Pagenstert et al. [60] demonstrated an excellent inter-observer reliability of SPECT/CT in localizing osteoarthritic changes in the foot. Studying 50 patients with SPECT/CT of the foot in retrospect, Singh et al. [61] reported a change in the treatment plan in 78 % of subjects and a resulting accuracy of 94 %. The patients studied by these authors had, however, not previously received an MRI. In a prospective study, 27/30 (90 %) patients treated by infiltration with local anesthetics of the structures most active on SPECT/CT reported significant pain reduction [62]. Based on the available evidence and their own clinical experience, Mohan et al. proposed a diagnostic algorithm for the imaging of patients with chronic foot pain, recommending SPECT/CT as the first tomographic imaging procedure in patients with previous surgery or metal implants and as the second tomographic examination in cases with an inconclusive MRI [32].
Several review articles suggest the usefulness of SPECT/CT also for the workup of patients with pain in the shoulders and the hips [32, 33]. Original articles presenting conclusive evidence proving this plausible assumption are, however, still scarce. This also applies to the diagnostic role of SPECT/CT in painful hip implants.
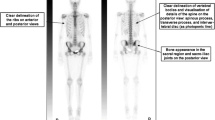
Osteoarthritis of the knee has received more attention in the recent literature. Figure 3 presents a pertinent example. In a series of carefully conducted studies, Hirschmann et al. and Rasch et al. [63, 64] established that intensity of tracer uptake as visualized by SPECT/CT reflects the specific loading patterns of the knee with regard to its alignment and that abnormal increases in tracer uptake are reversible on tibial osteotomy correcting for varus misalignment [65, 66]. Furthermore, they proposed a standardized, semi-automatic approach for the evaluation of tracer uptake in the knee in relation to component position following arthroplasty [67]. Using this method, they demonstrated that SPECT/CT imaging had therapeutic impact in 19/23 of the knees studied [68]. In a review article, Hirschmann et al. [69] proposed a central role for SPECT/CT for evaluating painful knee arthroplasty and recommended it as a second imaging procedure after planar radiography.
Methodological perspectives
For some years now, another nuclear medical technique for studying bone metabolism, i.e., PET with F-18-fluoride, has been a focus of increasing attention (for reviews, see [70, 71]). Some studies comparing its diagnostic performance in staging malignant disease with that of conventional nuclear medical bone imaging have demonstrated its superiority over planar bone scans and—albeit to a lesser degree—also over SPECT [72–75]. Evidence comparing F-18-fluoride PET/CT to skeletal SPECT/CT is still scanty [76], but nevertheless also indicates a slightly higher accuracy of PET/CT compared to hybrid SPECT/CT imaging for diagnosing osseous spread of malignancy. These results seem plausible in view of the superior imaging qualities of PET compared to SPECT, including its higher spatial resolution and its ability to measure tissue radioactivity concentration in vivo. Nevertheless, some technological progress in the field of SPECT/CT might help fill the gap between these two technologies as detailed below:
Very recent advances in skeletal SPECT/CT provide the possibility of measuring the uptake of the Tc-99m-labeled polyphosphonates in absolute units, e.g., in kBq/ml, as well as the possibility of performing multimodal image reconstruction which dramatically improves SPECT image quality.
Quantitative SPECT (QSPECT) was first introduced into nuclear medicine in the 1990s. In 1995, Rosenthal et al. [77] predicted that estimates of absolute SPECT tracer concentration would enter the clinical arena in the near future. However, to date, their prediction has not come to fruition, as only a few approaches based on QSPECT have been established in clinical practice (for reviews, see [15, 16]).
One of the first QSPECT protocols validated in humans was reported by Willowson et al. [78], who quantified the concentration of Tc-99m in the cardiac cavity in patients studied by radionuclide ventriculography. Other work by our research group proposed a QSPECT protocol for quantifying the tissue concentration of Tc-99m [79]. Our methodology, as well as that of Willowson et al., involves the use of co-registered data from X-ray CT to correct for attenuation and a window subtraction approach (dual-energy window) to correct for scattered counts. In each of these two studies, a gold standard was provided via an independent measurement of a patient’s blood or urine in an activimeter.
Building on the methodological setup developed by Zeintl et al. [79], we measured the activity concentration of Tc-99m-diphosphono-propanedicarboxylic acid in healthy spongious bone tissue, without focal SPECT and CT abnormalities, in 50 women referred for bone scintigraphy [80]. The concentration was found to be 48.15 ± 13.66 kBq/ml, translating into an average standardized uptake value (SUV) of 5.91 ± 1.54. These values are in the same range as those reported for F-18-NaF imaged with PET [81]. Furthermore, in this group of subjects, SUV determined in the vertebral bodies correlated significantly with the CT density of these bodies measured in HU (r = 0.678; p < 0.0001).
QSPECT of the bone might be of interest for modeling bone metabolism in osteoporosis and also for longitudinal monitoring of treatment response, e.g., in bone metastases. The integration of QSPECT into commercially available SPECT/CT systems will surely encourage research into its clinical value over the coming years.
The addition of the CT component to stand-alone SPECT systems aids both image reconstruction and lesion localization. Today, SPECT images are typically reconstructed using iterative techniques which benefit from additional CT information via attenuation correction. Further integration of CT information has been achieved in a novel reconstruction algorithm from Siemens Molecular Imaging [82]. This method—known as xSPECT Bone—uses the higher resolution CT data to enhance reconstructed nuclear resolution at tissue boundaries. xSPECT Bone produces images of tracer distribution with considerably higher quality than conventional iterative reconstruction techniques do (Fig. 4). Preliminary evidence shows that the improvement in SPECT image quality translates into higher confidence of diagnosis when staging malignant disease. The potential to more precisely localize increases in tracer uptake within complex structures such as joints leads to the assumption that orthopedic imaging, too, will benefit greatly from this option.
Sagittal SPECT images of the spine in a patient with a compression fracture of lumbar body 1. The multimodally reconstructed dataset (right) provides superior delineation of the osseous structures compared to the dataset reconstructed using a conventional ordered subsets maximum-likelihood algorithm (color figure online)
Conclusions
Skeletal scintigraphy is one of the most frequent in vivo procedures in the field of nuclear medicine. Visualizing bone metabolism, it exhibits a fairly high sensitivity to detect skeletal lesions, but has limitations in terms of specificity and spatial resolution, even when SPECT is used. Combining SPECT with X-ray CT helps overcome these limitations. This has, in particular, been shown when diagnosing bone involvement in malignant tumors. Emerging evidence indicates the benefit of hybrid imaging for bone scintigraphy during the workup of painful conditions affecting the back and the extremities. Methodological advances holding considerable promise for further improving its value are the quantitation of skeletal tracer uptake in absolute units, as well as multimodal image reconstruction techniques that have recently become available for use in clinical routine.
References
Myers WG (1975) The first radioindicator study in the life sciences with a man-made radionuclide: “Radioactive indicators in the study of phosphorus metabolism in rats, by O. Chievitz and G. Hevesy, reprinted from Nature 136: 754–755, Nov. 9, 1935”. J Nucl Med 16:1106–1108
Subramanian G, McAfee JG, Blair RJ, Kallfelz FA, Thomas FD (1975) Technetium-99m-methylene diphosphonate—a superior agent for skeletal imaging: comparison with other technetium complexes. J Nucl Med 16:744–755
Brenner AI, Koshy J, Morey J, Lin C, DiPoce J (2012) The bone scan. Semin Nucl Med 42:11–26. doi:10.1053/j.semnuclmed.2011.07.005
Schwartz Z, Shani J, Soskolne WA, Touma H, Amir D, Sela J (1993) Uptake and biodistribution of technetium-99m-MD32P during rat tibial bone repair. J Nucl Med 34:104–108
Toegel S, Hoffmann O, Wadsak W, Ettlinger D, Mien LK, Wiesner K, Nguemo J, Viernstein H, Kletter K, Dudczak R, Mitterhauser M (2006) Uptake of bone-seekers is solely associated with mineralisation! A study with 99mTc-MDP, 153Sm-EDTMP and 18F-fluoride on osteoblasts. Eur J Nucl Med Mol Imaging 33:491–494. doi:10.1007/s00259-005-0026-x
Even-Sapir E (2005) Imaging of malignant bone involvement by morphologic, scintigraphic, and hybrid modalities. J Nucl Med 46:1356–1367
Seo Y, Mari C, Hasegawa BH (2008) Technological development and advances in single-photon emission computed tomography/computed tomography. Semin Nucl Med 38:177–198. doi:10.1053/j.semnuclmed.2008.01.001
Beyer T, Veit-Haibach P (2014) State-of-the-art SPECT/CT: technology, methodology and applications-defining a new role for an undervalued multimodality imaging technique. Eur J Nucl Med Mol Imaging 41(Suppl 1):S1–S2. doi:10.1007/s00259-014-2696-8
Erba PA, Israel O (2014) SPECT/CT in infection and inflammation. Clin Transl Imaging. doi:10.1007/s40336-014-0092-9
Bach-Gansmo T, Schwarzlmüller T, Joraholmen V, Salbu J, Biermann M, Naum A, Kleven-Madsen N (2010) SPECT/CT hybrid imaging; with which CT? Contrast Media Mol Imaging 5:208–212. doi:10.1002/cmmi.375
Römer W, Nömayr A, Uder M, Bautz W, Kuwert T (2006) SPECT-guided CT for evaluating foci of increased bone metabolism classified as indeterminate on SPECT in cancer patients. J Nucl Med 47:1102–1106
Lohrmann C, Hauschild O, Meyer PT, Mix M, Strohm PC, Weber WA, Rischke HC (2013) Hybrid imaging of peripheral skeletal disease by SPECT/high-resolution flat-panel CT. J Nucl Med 54:1323–1326. doi:10.2967/jnumed.112.116343
Nömayr A, Römer W, Strobel D, Bautz W, Kuwert T (2006) Anatomical accuracy of hybrid SPECT/spiral CT in the lower spine. Nucl Med Commun 27:521–528
Bennewitz C, Kuwert T, Han J, Ritt P, Hahn D, Thimister W, Hornegger J, Uder M, Schmidt D (2012) Computer-aided evaluation of the anatomical accuracy of hybrid SPECT/spiral-CT imaging of lesions localized in the neck and upper abdomen. Nucl Med Commun 33:1153–1159. doi:10.1097/MNM.0b013e32835839cc
Ritt P, Vija H, Hornegger J, Kuwert T (2011) Absolute quantification in SPECT. Eur J Nucl Med Mol Imaging 38(Suppl 1):S69–S77. doi:10.1007/s00259-011-1770-8
Bailey DL, Willowson KP (2014) Quantitative SPECT/CT: SPECT joins PET as a quantitative imaging modality. Eur J Nucl Med Mol Imaging 41(Suppl 1):S17–S25. doi:10.1007/s00259-013-2542-4
Schulz V, Nickel I, Nömayr A, Vija AH, Hocke C, Hornegger J, Bautz W, Römer W, Kuwert T (2007) Effect of CT-based attenuation correction on uptake ratios in skeletal SPECT. Nuklearmedizin 46:36–42
Paycha F, Girma A (2011) Pattern-oriented approach in hybrid imaging (bisphosphonates-(99mTc) SPECT/CT and fluoride-(18F) PET/CT) according to bone abnormality phenotype: The sclerotic/osteoblastic lesion and the osteolytic/osteoclastic lesion. Médecine Nucléaire 35:332–335. doi:10.1016/j.mednuc.2011.02.020
Talbot JN, Paycha F, Balogova S (2011) Diagnosis of bone metastasis: recent comparative studies of imaging modalities. Q J Nucl Med Mol Imaging 55:374–410
Horger M, Eschmann SM, Pfannenberg C, Vonthein R, Besenfelder H, Claussen CD, Bares R (2004) Evaluation of combined transmission and emission tomography for classification of skeletal lesions. AJR Am J Roentgenol 183:655–661. doi:10.2214/ajr.183.3.1830655
Utsunomiya D, Shiraishi S, Imuta M, Tomiguchi S, Kawanaka K, Morishita S, Awai K, Yamashita Y (2006) Added value of SPECT/CT fusion in assessing suspected bone metastasis: comparison with scintigraphy alone and nonfused scintigraphy and CT. Radiology 238:264–271. doi:10.1148/radiol.2373041358
Zhang Y, Shi H, Gu Y, Xiu Y, Li B, Zhu W, Chen S, Yu H (2011) Differential diagnostic value of single-photon emission computed tomography/spiral computed tomography with Tc-99m-methylene diphosphonate in patients with spinal lesions. Nucl Med Commun 32:1194–1200. doi:10.1097/MNM.0b013e32834bd82e
Helyar V, Mohan HK, Barwick T, Livieratos L, Gnanasegaran G, Clarke SE, Fogelman I (2010) The added value of multislice SPECT/CT in patients with equivocal bony metastasis from carcinoma of the prostate. Eur J Nucl Med Mol Imaging 37:706–713. doi:10.1007/s00259-009-1334-3
Zhao Z, Li L, Li F, Zhao L (2010) Single photon emission computed tomography/spiral computed tomography fusion imaging for the diagnosis of bone metastasis in patients with known cancer. Skeletal Radiol 39:147–153. doi:10.1007/s00256-009-0764-0
Sharma P, Kumar R, Singh H, Bal C, Julka PK, Thulkar S, Malhotra A (2012) Indeterminate lesions on planar bone scintigraphy in lung cancer patients: SPECT, CT or SPECT-CT? Skeletal Radiol 41:843–850. doi:10.1007/s00256-011-1304-2
Sharma P, Jain TK, Reddy RM, Faizi NA, Bal C, Malhotra A, Kumar R (2014) Comparison of single photon emission computed tomography-computed tomography, computed tomography, single photon emission computed tomography and planar scintigraphy for characterization of isolated skull lesions seen on bone scintigraphy in cancer patients. Indian J Nucl Med 29:22–29. doi:10.4103/0972-3919.125766
Ndlovu X, George R, Ellmann A, Warwick J (2010) Should SPECT-CT replace SPECT for the evaluation of equivocal bone scan lesions in patients with underlying malignancies? Nucl Med Commun 31:659–665. doi:10.1097/MNM.0b013e3283399107
Strobel K, Burger C, Seifert B, Husarik DB, Soyka JD, Hany TF (2007) Characterization of focal bone lesions in the axial skeleton: performance of planar bone scintigraphy compared with SPECT and SPECT fused with CT. AJR Am J Roentgenol 188:W467–W474. doi:10.2214/ajr.06.1215
Zhang Y, Shi H, Cheng D, Jiang L, Xiu Y, Li B, Gu Y, Chen S (2013) Added value of SPECT/spiral CT versus SPECT in diagnosing solitary spinal lesions in patients with extraskeletal malignancies. Nucl Med Commun 34:451–458. doi:10.1097/MNM.0b013e32835fa552
Van der Wall H, Lee A, Magee M, Frater C, Wijesinghe H, Kannangara S (2010) Radionuclide bone scintigraphy in sports injuries. Semin Nucl Med 40:16–30. doi:10.1053/j.semnuclmed.2009.08.006
Nadel HR (2014) SPECT/CT in pediatric patient management. Eur J Nucl Med Mol Imaging 41(Suppl 1):S104–S114. doi:10.1007/s00259-014-2697-7
Mohan HK, Gnanasegaran G, Vijayanathan S, Fogelman I (2010) SPECT/CT in imaging foot and ankle pathology-the demise of other coregistration techniques. Semin Nucl Med 40:41–51. doi:10.1053/j.semnuclmed.2009.08.004
Huellner MW, Strobel K (2014) Clinical applications of SPECT/CT in imaging the extremities. Eur J Nucl Med Mol Imaging 41(Suppl 1):S50–S58. doi:10.1007/s00259-013-2533-5
Scheyerer MJ, Pietsch C, Zimmermann SM, Osterhoff G, Simmen HP, Werner CM (2014) SPECT/CT for imaging of the spine and pelvis in clinical routine: a physician’s perspective of the adoption of SPECT/CT in a clinical setting with a focus on trauma surgery. Eur J Nucl Med Mol Imaging 41(Suppl 1):S59–S66. doi:10.1007/s00259-013-2554-0
Even-Sapir E, Flusser G, Lerman H, Lievshitz G, Metser U (2007) SPECT/multislice low-dose CT: a clinically relevant constituent in the imaging algorithm of nononcologic patients referred for bone scintigraphy. J Nucl Med 48:319–324
Haworth AE, Webb J (2012) Skeletal complications of bisphosphonate use: what the radiologist should know. Br J Radiol 85:1333–1342. doi:10.1259/bjr/99102700
Dore F, Filippi L, Biasotto M, Chiandussi S, Cavalli F, Di Lenarda R (2009) Bone scintigraphy and SPECT/CT of bisphosphonate-induced osteonecrosis of the jaw. J Nucl Med 50:30–35. doi:10.2967/jnumed.107.048785
Balagué F, Mannion AF, Pellisé F, Cedraschi C (2007) Clinical update: low back pain. Lancet 369(9563):726–728. doi:10.1016/s0140-6736(07)60340-7
Matar HE, Navalkissoor S, Berovic M, Shetty R, Garlick N, Casey AT, Quigley AM (2013) Is hybrid imaging (SPECT/CT) a useful adjunct in the management of suspected facet joints arthropathy? Int Orthop 37:865–870. doi:10.1007/s00264-013-1811-y
Makki D, Khazim R, Zaidan AA, Ravi K, Toma T (2010) Single photon emission computerized tomography (SPECT) scan-positive facet joints and other spinal structures in a hospital-wide population with spinal pain. Spine J 10:58–62. doi:10.1016/j.spinee.2009.06.004
Lehman VT, Murphy RC, Maus TP (2013) 99mTc-MDP SPECT/CT of the spine and sacrum at a multispecialty institution: clinical use, findings, and impact on patient management. Nucl Med Commun 34(11):1097–1106. doi:10.1097/MNM.0b013e328364bfa6
Pneumaticos SG, Chatziioannou SN, Hipp JA, Moore WH, Esses SI (2006) Low back pain: prediction of short-term outcome of facet joint injection with bone scintigraphy. Radiology 238:693–698. doi:10.1148/radiol.2382041930
Dolan AL, Ryan PJ, Arden NK, Stratton R, Wedley JR, Hamann W, Fogelman I, Gibson T (1996) The value of SPECT scans in identifying back pain likely to benefit from facet joint injection. Br J Rheumatol 35:1269–1273
Koh WU, Kim SH, Hwang BY, Choi WJ, Song JG, Suh JH, Leem JG, Shin JW (2011) Value of bone scintigraphy and single photon emission computed tomography (SPECT) in lumbar facet disease and prediction of short-term outcome of ultrasound guided medial branch block with bone SPECT. Korean J Pain 24:81–86. doi:10.3344/kjp.2011.24.2.81
Lehman VT, Murphy RC, Kaufmann TJ, Diehn FE, Murthy NS, Wald JT, Thielen KR, Amrami KK, Morris JM, Maus TP (2014) Frequency of discordance between facet joint activity on technetium Tc99m methylene diphosphonate SPECT/CT and selection for percutaneous treatment at a large multispecialty institution. AJNR Am J Neuroradiol 35:609–614. doi:10.3174/ajnr.A3731
Ackerman WE 3rd, Ahmad M (2008) Pain relief with intraarticular or medial branch nerve blocks in patients with positive lumbar facet joint SPECT imaging: a 12-week outcome study. South Med J 101:931–934. doi:10.1097/SMJ.0b013e31817e6ffb
Solá M, Pérez R, Cuadras P, Diaz R, Holgado S, Puyalto P, Iborra M, Fraile M (2011) Value of bone SPECT-CT to predict chronic pain relief after percutaneous vertebroplasty in vertebral fractures. Spine J 11:1102–1107. doi:10.1016/j.spinee.2011.11.003
Resnick DK, Watters WC 3rd, Mummaneni PV, Dailey AT, Choudhri TF, Eck JC, Sharan A, Groff MW, Wang JC, Ghogawala Z, Dhall SS, Kaiser MG (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 10: Lumbar fusion for stenosis without spondylolisthesis. J Neurosurg Spine 21:62–66. doi:10.3171/2014.4.spine14275
Resnick DK, Watters WC 3rd, Sharan A, Mummaneni PV, Dailey AT, Wang JC, Choudhri TF, Eck J, Ghogawala Z, Groff MW, Dhall SS, Kaiser MG (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 9: lumbar fusion for stenosis with spondylolisthesis. J Neurosurg Spine 21:54–61. doi:10.3171/2014.4.spine14274
Even-Sapir E, Martin RH, Mitchell MJ, Iles SE, Barnes DC, Clark AJ (1994) Assessment of painful late effects of lumbar spinal fusion with SPECT. J Nucl Med 35:416–422
Sumer J, Schmidt D, Ritt P, Lell M, Forst R, Kuwert T, Richter R (2013) SPECT/CT in patients with lower back pain after lumbar fusion surgery. Nucl Med Commun 34:964–970. doi:10.1097/MNM.0b013e328363cf81
Damgaard M, Nimb L, Madsen JL (2010) The role of bone SPECT/CT in the evaluation of lumbar spinal fusion with metallic fixation devices. Clin Nucl Med 35:234–236. doi:10.1097/RLU.0b013e3181d18cdd
Rager O, Schaller K, Payer M, Tchernin D, Ratib O, Tessitore E (2012) SPECT/CT in differentiation of pseudarthrosis from other causes of back pain in lumbar spinal fusion: report on 10 consecutive cases. Clin Nucl Med 37:339–343. doi:10.1097/RLU.0b013e318239248b
Linke R, Kuwert T, Uder M, Forst R, Wuest W (2010) Skeletal SPECT/CT of the peripheral extremities. AJR Am J Roentgenol 194:W329–W335. doi:10.2214/ajr.09.3288
Ito S, Yamamoto Y, Tanii T, Aga F, Nishiyama Y (2013) SPECT/CT imaging in ulnocarpal impaction syndrome. Clin Nucl Med 38:841–842. doi:10.1097/RLU.0b013e31828da39d
Allainmat L, Aubault M, Noel V, Baulieu F, Laulan J, Eder V (2013) Use of hybrid SPECT/CT for diagnosis of radiographic occult fractures of the wrist. Clin Nucl Med 38:e246–e251. doi:10.1097/RLU.0b013e318263819e
Huellner MW, Bürkert A, Schleich FS, Schürch M, Hug U, von Wartburg U, Strobel K, Veit-Haibach P (2012) SPECT/CT versus MRI in patients with nonspecific pain of the hand and wrist—a pilot study. Eur J Nucl Med Mol Imaging 39:750–759. doi:10.1007/s00259-011-2034-3
Schleich FS, Schürch M, Huellner MW, Hug U, von Wartburg U, Strobel K, Veit-Haibach P (2012) Diagnostic and therapeutic impact of SPECT/CT in patients with unspecific pain of the hand and wrist. EJNMMI Res 2:53. doi:10.1186/2191-219x-2-53
Krüger T, Hug U, Hüllner MW, Schleich F, Veit-Haibach P, von Wartburg U, Strobel K (2011) SPECT/CT arthrography of the wrist in ulnocarpal impaction syndrome. Eur J Nucl Med Mol Imaging 38:792. doi:10.1007/s00259-010-1712-x
Pagenstert GI, Barg A, Leumann AG, Rasch H, Muller-Brand J, Hintermann B, Valderrabano V (2009) SPECT-CT imaging in degenerative joint disease of the foot and ankle. J Bone Joint Surg Br 91:1191–1196. doi:10.1302/0301-620x.91b9.22570
Singh VK, Javed S, Parthipun A, Sott AH (2013) The diagnostic value of single photon-emission computed tomography bone scans combined with CT (SPECT-CT) in diseases of the foot and ankle. Foot Ankle Surg 19:80–83. doi:10.1016/j.fas.2012.11.002
Kretzschmar M, Wiewiorski M, Rasch H, Jacob AL, Bilecen D, Walter MA, Valderrabano V (2011) 99mTc-DPD-SPECT/CT predicts the outcome of imaging-guided diagnostic anaesthetic injections: a prospective cohort study. Eur J Radiol 80:e410–e415. doi:10.1016/j.ejrad.2010.09.013
Hirschmann MT, Schön S, Afifi FK, Amsler F, Rasch H, Friederich NF, Arnold MP (2013) Assessment of loading history of compartments in the knee using bone SPECT/CT: a study combining alignment and 99mTc-HDP tracer uptake/distribution patterns. J Orthop Res 31:268–274. doi:10.1002/jor.22206
Schön SN, Afifi FK, Rasch H, Amsler F, Friederich NF, Arnold MP, Hirschmann MT (2013) Assessment of in vivo loading history of the patellofemoral joint: a study combining patellar position, tilt, alignment and bone SPECT/CT. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2698-2
Mucha A, Dordevic M, Hirschmann A, Rasch H, Amsler F, Arnold MP, Hirschmann MT (2014) Effect of high tibial osteotomy on joint loading in symptomatic patients with varus aligned knees: a study using SPECT/CT. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3053-y
Mucha A, Dordevic M, Testa EA, Rasch H, Hirschmann MT (2013) Assessment of the loading history of patients after high tibial osteotomy using SPECT/CT–a new diagnostic tool and algorithm. J Orthop Surg Res 8:46. doi:10.1186/1749-799x-8-46
Hirschmann MT, Mathis D, Rasch H, Amsler F, Friederich NF, Arnold MP (2013) SPECT/CT tracer uptake is influenced by tunnel orientation and position of the femoral and tibial ACL graft insertion site. Int Orthop 37:301–309. doi:10.1007/s00264-012-1704-5
Hirschmann MT, Konala P, Iranpour F, Kerner A, Rasch H, Friederich NF (2011) Clinical value of SPECT/CT for evaluation of patients with painful knees after total knee arthroplasty–a new dimension of diagnostics? BMC Musculoskelet Disord 12:36. doi:10.1186/1471-2474-12-36
Hirschmann MT, Henckel J, Rasch H (2013) SPECT/CT in patients with painful knee arthroplasty-what is the evidence? Skeletal Radiol 42:1201–1207. doi:10.1007/s00256-013-1657-9
Bastawrous S, Bhargava P, Behnia F, Djang DS, Haseley DR (2014) Newer PET application with an old tracer: role of 18F-NaF Skeletal PET/CT in oncologic practice. Radiographics 34:1295–1316. doi:10.1148/rg.345130061
Fischer DR (2013) Musculoskeletal imaging using fluoride PET. Semin Nucl Med 43:427–433. doi:10.1053/j.semnuclmed.2013.06.004
Schirrmeister H, Glatting G, Hetzel J, Nussle K, Arslandemir C, Buck AK, Dziuk K, Gabelmann A, Reske SN, Hetzel M (2001) Prospective evaluation of the clinical value of planar bone scans, SPECT, and (18)F-labeled NaF PET in newly diagnosed lung cancer. J Nucl Med 42:1800–1804
Schirrmeister H, Guhlmann A, Elsner K, Kotzerke J, Glatting G, Rentschler M, Neumaier B, Trager H, Nussle K, Reske SN (1999) Sensitivity in detecting osseous lesions depends on anatomic localization: planar bone scintigraphy versus 18F PET. J Nucl Med 40:1623–1629
Even-Sapir E, Metser U, Mishani E, Lievshitz G, Lerman H, Leibovitch I (2006) The detection of bone metastases in patients with high-risk prostate cancer: 99mTc-MDP planar bone scintigraphy, single- and multi-field-of-view SPECT, 18F-fluoride PET, and 18F-fluoride PET/CT. J Nucl Med 47:287–297
Ota N, Kato K, Iwano S, Ito S, Abe S, Fujita N, Yamashiro K, Yamamoto S, Naganawa S (2014) Comparison of 18F-fluoride PET/CT, 18F-FDG PET/CT and bone scintigraphy (planar and SPECT) in detection of bone metastases of differentiated thyroid cancer: a pilot study. Br J Radiol 87(1034):20130444. doi:10.1259/bjr.20130444
Chakraborty D, Bhattacharya A, Mete UK, Mittal BR (2013) Comparison of 18F fluoride PET/CT and 99mTc-MDP bone scan in the detection of skeletal metastases in urinary bladder carcinoma. Clin Nucl Med 38:616–621. doi:10.1097/RLU.0b013e31828da5cc
Rosenthal MS, Cullom J, Hawkins W, Moore SC, Tsui BM, Yester M (1995) Quantitative SPECT imaging: a review and recommendations by the Focus Committee of the Society of Nuclear Medicine Computer and Instrumentation Council. J Nucl Med 36:1489–1513
Willowson K, Bailey DL, Bailey EA, Baldock C, Roach PJ (2010) In vivo validation of quantitative SPECT in the heart. Clin Physiol Funct Imaging 30:214–219. doi:10.1111/j.1475-097X.2010.00930.x
Zeintl J, Vija AH, Yahil A, Hornegger J, Kuwert T (2010) Quantitative accuracy of clinical 99mTc SPECT/CT using ordered-subset expectation maximization with 3-dimensional resolution recovery, attenuation, and scatter correction. J Nucl Med 51:921–928. doi:10.2967/jnumed.109.071571
Cachovan M, Vija AH, Hornegger J, Kuwert T (2013) Quantification of 99mTc-DPD concentration in the lumbar spine with SPECT/CT. EJNMMI Res 3:45. doi:10.1186/2191-219x-3-45
Frost ML, Blake GM, Park-Holohan SJ, Cook GJ, Curran KM, Marsden PK, Fogelman I (2008) Long-term precision of 18F-fluoride PET skeletal kinetic studies in the assessment of bone metabolism. J Nucl Med 49:700–707. doi:10.2967/jnumed.107.046987
Vija HA (2013) Introduction to xSPECT technology: evolving multi-modal SPECT to become context-based and quantitative. Siemens Medical Solutions USA. http://www.healthcare.siemens.com/molecular-imaging/customer-portal-resource/expand-scanner-capabilities/symbia-intevo
Acknowledgments
The author gratefully acknowledges the language review performed by James C. Sanders as well as Dr Philipp Ritt's help with submitting the manuscript. Furthermore, the manuscript benefitted considerably from the in-depth discussions on SPECT/CT and related matters with these two colleagues.
Conflict of interest
Torsten Kuwert has an ongoing research collaboration with Siemens Molecular Imaging in the field of SPECT/CT. He gives occasional lectures on behalf of Siemens Molecular Imaging pertaining to SPECT/CT research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Color figures online at http://link.springer.com/article/10.1007/s40336-014-0090-y.
Rights and permissions
About this article
Cite this article
Kuwert, T. Skeletal SPECT/CT: a review. Clin Transl Imaging 2, 505–517 (2014). https://doi.org/10.1007/s40336-014-0090-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-014-0090-y