Abstract
Since the identification of Fetal Alcohol Syndrome over 40 years ago, much has been learned about the detrimental effects of prenatal alcohol exposure on the developing brain. This review highlights recent neuroimaging studies within the context of previous work. Structural magnetic resonance imaging has described morphological differences in the brain and their relationships to cognitive deficits and measures of facial dysmorphology. Diffusion tensor imaging has elaborated on the relationship between white matter microstructure and behavior. Atypical neuromaturation across childhood and adolescence has been observed in longitudinal neuroimaging studies. Functional imaging has revealed differences in neural activation patterns underlying sensory processing, cognition, and behavioral deficits. A recent functional connectivity analysis demonstrates reductions in global network efficiency. Despite this progress, much remains unknown about the impact of prenatal alcohol exposure on the brain, and continued research efforts are essential.
Similar content being viewed by others
Introduction
It is now widely accepted that heavy alcohol consumption during pregnancy can have life-long adverse consequences on the developing embryo and fetus. Despite this knowledge and increased public awareness of the risks associated with drinking during pregnancy, the Centers for Disease Control and Prevention found that in the USA, 7.6 % of pregnant women reported consuming alcohol within the 30 days prior to survey, and 1.4 % reported binge drinking [1].
Perhaps the best-known outcome of prenatal alcohol exposure is Fetal Alcohol Syndrome (FAS), which was documented in the medical literature over 40 years ago [2, 3]. Distinct facial characteristics, growth retardation, and central nervous system anomalies were observed in offspring exposed to large amounts of alcohol in utero. However, a host of factors, such as alcohol dose and timing of exposure, nutritional status, and genetics, converge to affect the phenotype. Fetal Alcohol Spectrum Disorders (FASD) is the non-diagnostic, umbrella term used to refer to the entire continuum of outcome severity. Among the most serious consequences of in utero alcohol exposure are the effects on the brain and the resulting alterations in behavior and cognition. Importantly, these effects can occur even among individuals without all of the features of FAS [4, 5].
Early autopsy examinations of individuals with heavy prenatal alcohol exposure revealed brain abnormalities, including microcephaly as well as anomalies of specific brain structures [6]. While informative, these autopsy studies often represented the most severe cases of prenatal alcohol exposure, limiting their generalizability. Numerous neuroimaging studies are now available describing the detrimental impact of prenatal alcohol exposure on the brain, and several recent reviews are available [7–10]. This review provides an update, highlighting some of the more recent neuroimaging studies within the context of previous research. Tables 1 and 2 summarize the structural and functional research findings from 2011 to the present and additional supplementary tables (Tables 3–6) that outline the neuroimaging findings over the past 4 decades are provided online.
Brain Size
Prenatal alcohol exposure has widespread detrimental effects on the brain, and many studies have reported an association between such exposure and a reduction in total brain size (refer to supplementary Table 3). Some areas of the brain may be particularly affected by alcohol exposure. To examine such effects, Chen et al. [11] divided the brain into 68 cortical and 20 subcortical regions of interest (ROI). Although they did not correct for multiple comparisons, they reported that the absolute volume of nearly every region was significantly reduced in young adults prenatally exposed to alcohol. The authors also identified several specific subcortical and cortical regions that were related to the quantity of exposure or were disproportionately reduced (i.e., above the effects of total brain volume reduction; refer to Table 1). Of note, the posterior corpus callosum and bilateral cerebellum volumes demonstrated a negative relationship with the quantity of prenatal alcohol exposure, while the caudate nuclei were reported as disproportionately reduced. These findings are consistent with prior studies suggesting the vulnerability of these regions to alcohol. In addition, they reported that the bilateral pars opercularis, an area of the frontal lobes important for language ability, is negatively related to the quantity of alcohol exposure. Interestingly, the volumes of the bilateral lingual gyri, areas important for visual processing, were not only negatively related to the quantity of alcohol exposure but also were significantly reduced even after accounting for total brain size. Both verbal ability and visual processing are affected in FASD, and the effects in the pars opercularis and lingual regions may contribute to some of these deficits.
Rajaprakash et al. [12] examined cortical brain alterations associated with heavy prenatal alcohol exposure in children and adolescents diagnosed with Alcohol-Related Neurodevelopmental Disorder (ARND). Reductions in absolute total brain volume and in cortical volume and surface area were found. When examining regional effects, both diminished cortical grey matter volume and surface area were apparent in bilateral frontal regions. Total volume reductions were observed in bilateral parietal and right temporal cortices; while surface area reductions were seen in bilateral temporal and the right occipital cortex. However, these reductions were not evident after correcting for total brain volume and no alterations were seen in cortical thickness. Prior work is mixed regarding the relationship between prenatal alcohol exposure and cortical thickness, reporting both increases [13–15] and decreases [16]. Other studies have found disproportionate volumetric reductions in specific brain areas [17, 18, 11]; however, those reports included individuals with heavy prenatal alcohol exposure who fell along the entire continuum of diagnoses, including those with facial dysmorphology. In the study by Rajaprakash et al. children with ARND had heavy prenatal alcohol exposure and cognitive or behavioral deficits, but no facial dysmorphia. Several previous studies have found that groups composed of individuals diagnosed with FAS may display regionally disproportionate volumetric reductions, while such reductions may not achieve statistical significance in alcohol-exposed groups of children who do not meet criteria for FAS [17, 18].
Brain Shape
Shape measurements provide additional insights regarding brain changes associated with prenatal alcohol exposure, either in addition to or in the absence of volume differences. For example, early reports described corpus callosum malformation. The corpus callosum is a band of white matter that connects the two hemispheres. Some individuals with prenatal alcohol exposure were reported to have complete or partial agenesis [18–21] or displacement [22–25]. The shape deviations also included callosal extension and compression as well as relative thickening and thinning; malformation in either direction was related to deficits in executive functioning or motor control [25].
Recent studies report variations in the shape of the bilateral caudate and hippocampal nuclei [26]. Hippocampal deformations were observed spreading across the body and tail regions on the superior surface and on the head of the inferior surface, bilaterally. In the right hippocampus, the inferior surface deformation spread from the head to the tail region. Furthermore, contraction of the anterior region of the right hippocampus head was associated with greater prenatal alcohol exposure. The left caudate was deformed in the body and tail regions of the lateral surface, and contraction of the tail region of the right caudate was associated with greater alcohol exposure. Although Joseph et al. [26] report significant deformations, only trend-level group differences in absolute volume of the bilateral caudate and left hippocampus were reported. More work will be necessary to determine how shape variation of these regions may relate to the deficits reported in FASD. Given that prior research has found a positive relationship between hippocampal volume and spatial recall [27]; caudate volume and inhibitory control [28]; and volumes of both these regions are implicated in verbal learning and recall deficits in FASD [28, 27], shape deviations may well also be associated with such deficits. As shape deviations in the right caudate and hippocampus were related to the quantity of alcohol exposure, perhaps a relationship between verbal ability and shape variation in these regions would also be detectable among individuals with more moderate or low-dose alcohol exposures.
Shape changes have also been previously reported in the cerebral cortex. For example, reductions were evident in the distance from the center of the brain to surface points in the left hemisphere orbitofrontal cortex and the bilateral inferior parietal/perisylvian areas, giving the appearance of a blunted, narrower brain [29]. More recently, De Guio et al. [30] described changes in cortical folding among children with FASD. Cortical folding abnormalities are seen in several disorders of neuronal migration and the associated malformations may range from lissencephaly (the absence of cortical folding) to polymicrogyria (many small folds). Polymicrogyria was described in a prior case of FAS [31]. De Guio et al. [30] found that cortical complexity, defined as the average ratio of sulcal to gyral surface area, was reduced in children with prenatal alcohol exposure: a smaller proportion of the cortical surface area was buried within the cerebral folds. The children of women who consumed the greatest amount of alcohol per day showed the greatest effect. Furthermore, the authors noted that the fold opening, or distance between the sulcal ‘walls’, was greater in children exposed to gestational alcohol in the majority of cortical regions. These effects were observed in children with and without microcephaly, suggesting that these deviations in the folding pattern were not primarily due to having a smaller brain.
White Matter Microstructure
White matter microstructure in the brain can be assessed with diffusion tensor imaging (DTI), which measures the diffusion of water molecules in tissue. Common measures of tissue integrity include indices of average diffusion (mean diffusivity [MD]), and diffusion isotropy (fractional anisotropy [FA]). These measures of white matter integrity reflect numerous aspects of tissue structure, including myelination, axonal integrity, and fiber organization (for additional discussion see Neil et al. [32]). Widespread diffusion abnormalities are found among alcohol-exposed individuals (refer to Supplementary Table 4). As an example, reduced FA and increased MD are seen in the splenium and genu of the corpus callosum, respectively [33]. Typically, low FA and high MD are associated with poorer microstructural integrity; however, this may not always be the case.
Green et al. [34] described relationships between white matter microstructure and reaction time during prosaccades (eye movement towards a peripheral stimulus) and antisaccades (eye movement away from a peripheral stimulus) in children with FASD. Lower FA in the cerebellum was related to slower reaction times during prosaccades. However, lower FA in the genu of the corpus callosum and the inferior longitudinal fasciculus was related to faster reaction times during prosaccades, and in a large portion of the right corpus callosum lower FA was related to faster reaction time on antisaccades. The authors speculated that the negative relationship between FA in the corpus callosum and inferior longitudinal fasciculus and reaction times may be due to factors that artificially inflate FA, such as a reduced dispersion or branching of axons within a voxel.
Brain Maturation
The brain is highly dynamic and undergoes complex changes across development. In healthy children, brain maturation follows a non-linear, regionally heterochronous trajectory. Maturation of both cortical grey matter and white matter microstructure begins in more posterior regions, progressing towards the later-maturing frontal areas. Cortical grey matter volume development includes a period of brain growth across childhood, followed by a decline in volume during adolescence [35]. In white matter, nonlinear increases in FA and reductions in MD are seen from childhood to adulthood [36].
Children with heavy prenatal alcohol exposure displayed a more linear trajectory of cortical volume loss without much evidence of age-appropriate volume increases in several cortical areas, including the bilateral inferior parietal, and the left lateral occipital and superior parietal areas, and right postcentral and banks of the superior temporal regions [37•]. Additionally, children with prenatal alcohol exposure displayed a greater change in white matter integrity in several tracts, including a steeper decline in MD in the superior fronto-occipital, inferior-fronto-occipital, and superior longitudinal fasciculi [38•]. The blunted grey matter volume change is suggestive of compromised pruning and diminished plasticity in the cerebral cortex, whereas the steeper reduction in MD may reflect delayed myelination in alcohol-exposed children.
It appears that prenatal alcohol exposure has an enduring impact on brain development; however, an important consideration is how the environment may contribute. Environmental experience has an integral role in determining brain morphology, physiology, and chemistry (for review refer to Sale et al. [39]). Environmental input is converted to patterns of neural activity that drive functional and structural plasticity; however, prenatal alcohol exposure may change the brain’s ability to incorporate such experience. Additionally, individuals with prenatal alcohol exposure may have a fundamentally different life experience from those who are typically developing, not only during the fetal period but also in postnatal stages. Experiencing additional stressors, malnutrition, and/or limited enrichment along with the prenatal alcohol exposure may converge to produce a brain with a disrupted developmental trajectory.
Brain Activation: Sensory Processing
Magnetoencephalography (MEG) is a noninvasive imaging method that measures magnetic fields produced by electrical activity in the brain. Several recent studies using MEG have reported brain activity differences in FASD during sensory processing. During auditory stimulus presentation, young children with FASD displayed an approximate 10 ms delay in cortical auditory processing (M100 and M200 latencies) compared with controls [40]. On a prosaccade task, adolescents with FASD exhibited a delay in visual cortex activation (M100 peak latency). Furthermore, during this visual task, gamma-band oscillations differed between FASD and controls. Gamma oscillations are periodic fluctuations in the local field potential, driven by synchronized interactions between a network of inhibitory interneurons and excitatory principle neurons in the cortex. Gamma oscillations tend to increase in magnitude in the presence of a cognitive or perceptual stimulus. This magnitude escalation may reflect increases in local field potential synchrony, amplitude (power) or both [41]. In FASD, relative increases in gamma oscillations were seen in right frontal clusters, while relative decreases occurred in right parietal and left temporal/occipital clusters [42]. These gamma-band power changes occurred despite a lack of difference in task performance in these groups. In addition, in adolescents with FASD there was a positive relationship between M100 peak latency and gamma oscillatory power in a cluster located around the medial frontal eye field region [42]. No such relationship was apparent in controls, and gamma-band power was not correlated with saccadic reaction time in either group. Stephen et al. [42] suggested that the altered gamma-band power might represent an imbalance between neuronal excitation and inhibition.
Brain Activation: Cognition
Functional brain changes associated with FASD have also been examined with functional magnetic resonance imaging (fMRI), which measures the blood oxygen level-dependent (BOLD) change in the brain (i.e., the hemodynamic response). Neural activation differences associated with prenatal alcohol exposure as compared with healthy control subjects have been observed during several different cognitive tasks, including response inhibition [43, 44], working memory [45, 46•, 47, 48, 49•, 50], arithmetic and number processing [51, 52], and verbal learning [53]. Many of these studies have been described in prior reviews [7, 9]. Of note is the large number of fMRI studies that report differences in activation among individuals with FASD in frontal regions relative to healthy controls regardless of the task used (refer to Supplementary Table 5).
On a go/no-go, task O'Brien et al. [44] found that, despite similar inhibitory behavioral performance across trials, children with prenatal alcohol exposure displayed greater neural activation in several frontal and parietal regions during response inhibition, which is similar to a previous report [43]. However, the authors also found that when a predictive cue signaled the need to inhibit a response, alcohol-exposed subjects displayed poorer ‘go’ response accuracy and a more conservative response bias, as well as reduced activation in left pre- and postcentral gyri. The authors suggest that the alcohol-exposed children were not utilizing the cue signal to the same extent as controls and that deficits in nonverbal learning may contribute to the poorer cued-trial performance.
In an n-back verbal working memory task, Diwadkar et al. [54] observed activation patterns that differed not only between controls and prenatal alcohol exposed subjects, but also between the alcohol-exposed subjects with and without dysmorphic facial features. As task difficulty increased, each group displayed unique activation patterns. The non-exposed controls increased activity in Broca’s area; non-dysmorphic alcohol-exposed subjects exhibited increases in fronto-striatal network activation; and alcohol-exposed subjects with facial dysmorphism showed activity increases in cerebellar and parietal areas. Furthermore, the between-group comparisons revealed that the non-dysmorphic children displayed greater activation of the dorsolateral prefrontal cortex, while children with facial dysmorphology had reduced activation in a specific region of Broca’s area associated with sub-vocal rehearsal. These group differences in activation occurred despite a lack of difference in behavioral task performance. However, the two alcohol-exposed groups did differ in the quantity of alcohol exposure. The children in the dysmorphic group were exposed to more alcohol on average and per occasion. The differences in alcohol dosage may have contributed to the distinct activation patterns observed between the dysmorphic and non-dysmorphic alcohol-exposed groups. Regardless of the dosage, the alcohol-exposed children displayed altered activation compared with controls.
Brain Activation: Resting-State
An alternative to measuring fMRI response activation during a task is to measure BOLD activity fluctuations at rest. The ‘resting brain’ exhibits low-frequency spontaneous BOLD signal changes that are correlated across connected regions [55], allowing for assessment of functional connections among neural networks [56, 57]. Several brain regions are more active at rest than during cognitive tasks (e.g. medial prefrontal cortex, posterior cingulate cortex, precuneus, inferior parietal lobules, and medial temporal regions) and are referred to as the default mode network [58]. Resting-state functional connectivity among several default mode regions (medial prefrontal cortex, posterior cingulate cortex, and inferior parietal lobules) was reduced in young adults with FASD [59]. In addition, children and adolescents with FASD displayed interhemispheric functional connectivity disruption [60]. In a recent analysis of functional connectivity that sought to examine brain network efficiency, Wozniak et al. [61] found that children with FASD displayed a 3.1 % increase in characteristic path length, implying less reliance on long-distance communication and a greater reliance on multiple smaller connections in the neural network. In addition, they showed a 1.9 % reduction in global efficiency, suggesting reduced network capacity for parallel information processing. The clinical significance of such change is not yet understood, but the alcohol-exposed brain appears to be working in a less efficient manner. Wozniak et al. [61] also examined the relationship between cognitive performance and both characteristic path length and global efficiency. While the relationship did not survive correction for multiple comparisons, the findings suggested an association with poorer immediate memory capacity measured with the California Verbal Learning Test.
FASD Versus Contrast Groups
Many imaging studies have compared prenatal alcohol-exposed youths with healthy controls, providing substantial information regarding how such exposure results in deviations from more typical neurodevelopment. However, there are a number of factors that may contribute to the FASD phenotype, above and beyond alcohol-exposure histories. Several recent studies compared subjects with prenatal alcohol exposure with other relevant contrast groups to examine differences in brain activation [46•, 49] and white matter microstructure [46•].
Given that a large degree of variance in alcohol usage in the population can be attributed to genetic influences (heritability estimates are 50–60 % [62]), the genetic factors that contribute to maternal proclivity towards alcohol consumption may also contribute to the observed functional brain changes in FASD. To examine the potential role of family history of alcoholism, Norman et al. [49•] examined brain activation patterns during an fMRI spatial working memory task among children with (1) heavy prenatal alcohol exposure; (2) family history positive for alcoholism (FHP); and (3) healthy controls. In general, the greatest differences in BOLD activation were between alcohol-exposed and control groups, while the FHP group displayed a more intermediate pattern of activation. Relative increases in BOLD activation of frontal areas during the spatial working memory task were unique to the alcohol-exposed children and likely due to their exposure rather than a family history of alcoholism. However, having a family history of alcoholism may have contributed to the increased activation of the lentiform nucleus and insula, as these areas were activated in both the alcohol-exposed and the FHP groups.
Co-occurring psychiatric conditions may also contribute to altered brain activation observed in FASD. Attention deficits are prevalent among individuals with prenatal alcohol exposure, and many of these children meet diagnostic criteria for attention-deficit/hyperactivity disorder (ADHD) [63]. Malisza et al. [46] reported fMRI BOLD response differences on a spatial working memory task in alcohol-exposed children in comparison with both non-exposed children with ADHD and healthy controls. Task performance was similar between the alcohol-exposed and the ADHD children, although the controls performed better than both clinical groups. The general pattern of activation differences indicated that relative to controls, children with alcohol exposure exhibited increases in activation, while children with ADHD showed decreases in activation on this task. There were no regions in which the ADHD children displayed increased activation relative to alcohol-exposed children, but alcohol-exposed children showed enhanced activation relative to ADHD in the bilateral pre- and postcentral regions, right middle frontal gyrus, and left inferior frontal gyrus. Furthermore, DTI tractography demonstrated that while alcohol-exposed children displayed a reduction in fiber volume and total number of fibers compared with healthy controls, non-exposed children with ADHD did not significantly differ from either the alcohol-exposed or the control groups. Although children with prenatal alcohol exposure may have similar behavioral and cognitive deficits as in ADHD, the underlying neural mechanisms appear to be at least partially distinct.
Facial Dysmorphology
Several areas of the brain display relationships with facial dysmorphology in children with histories of heavy prenatal alcohol exposure. The dysmorphic facial features that are characteristic of FAS include (1) small palpebral fissures (the length of the opening of the eye), (2) smooth philtrum (the vertical groove perpendicular to the nose and lip), and (3) thin vermillion (upper lip) [64]. Shorter palpebral fissure length was related to smaller ventral diencephalon bilaterally [65]; a thinner corpus callosum, particularly in the anterior third [66]; and increased cortical thickness in the right inferior frontal cortex [15]. A higher philtrum lipometer score, which indicated more severe dysmorphology, predicted reductions in the bilateral thalami and left palladium volumes [65]. Greater dysmorphism of both these facial features was also related to a lower full-scale IQ score [65]. Furthermore, there may be some differences in brain maturation among children with and without dysmorphic facial features, as children with more severe facial dysmorphology also displayed more blunted cortical volume change over time [37•].
While facial measures reflect gross structural brain anomalies in prenatal alcohol-exposed individuals, it is not clear whether facial dysmorphology relates to white matter microstructural or functional brain changes. No relationship has been observed between corpus callosum microstructure and facial dysmorphology [67, 68], although a positive relationship between FA in the left middle cerebellar peduncle and diagnostic severity has been reported [69]. There may be a relationship between brain activation and diagnostic severity, as Diwadkar et al. [54] showed that children with a diagnosis of FAS/partial-FAS activated different regions during a working memory task as compared with heavily exposed nonsyndromal children. However, when examining activation patterns during resting state, no relationship between facial dysmorphology and functional connectivity was observed [60, 61]. More work is necessary to determine whether a relationship may exist between facial dysmorphology and measures of white matter integrity and/or brain activation patterns.
Further study of the relationship between facial dysmorphology and the brain may help to elucidate the full nature of the teratogenicity of alcohol. Additionally, characterization of these relationships could also lead to earlier identification of individuals affected by prenatal alcohol exposure, and hopefully earlier and more targeted interventions. A particularly promising avenue in this regard lies within 3D facial imaging methodologies. Suttie et al. [70•] found that among nonsyndromal heavily exposed children, those with more FAS-like facial features performed poorer on neurobehavioral assessment than the children with more control-like features. Given the knowledge of the reciprocal relationships between facial dysmorphology and brain/cognitive changes, sensitive facial imaging methods may prove to be an extremely valuable diagnostic tool.
Summary and Conclusion
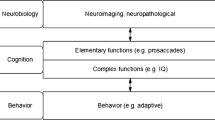
Structural MRI studies demonstrate the global and widespread impact of prenatal alcohol exposure, but also implicate some specific brain areas that may be particularly vulnerable. For example, evidence continues to accumulate indicating that the caudate may be one such region. Disproportionate reductions [11] or deformation [26] of the caudate have been recently reported. Caudate volume has also been shown to predict neurobehavioral disruption [28]. DTI studies are linking the alcohol-induced white matter microstructural changes to specific deficits, most recently oculomotor control [34]. Furthermore, recent evidence demonstrates that the developmental trajectory of both cerebral cortex volume and white matter microstructure is altered [37•, 38•]. Continued longitudinal research examining brain development over the lifespan is necessary. Longer latencies between sensory stimulus presentation and cortical activation detected with MEG demonstrate deficits in auditory processing in young children and visual stimulus processing in adolescents [40, 71]. BOLD changes during cognitive tasks continue to reveal differing activation patterns between alcohol-exposed youth and more typically developing controls [44]. Further, the BOLD activation patterns among individuals with FASD are also at least partially distinct from contrast groups, including ADHD [46]. These findings provide evidence not only for different neuropathology but also suggest that these two clinical groups may be in need of distinct treatment strategies.
In general, the neural anomolies associated with FASD measured with neuroimaging technologies account for only a small proportion of variance that contributes to cognitive or behavioral disruption. These complex relationships involve genetic factors, environmantal experience, and timing of developmental events, among others, and converge to affect the whole brain and resultant behavior. As a majority of the neuroimaging studies to date are cross-sectional, it is not possible to determine whether the observed brain changes are the cause or product of disrupted cogntition and behavior, or whether the observed brain/behavior relationships in FASD vary together due to some other factor(s).
Continued research efforts aimed at identifying vulnerable brain targets of alcohol teratogenicity are essential. Establishing relationships between brain alterations and quantity of alcohol exposure, facial dysmorphology, and behavioral/cognitive deficits will aid in the identification of unique and specific brain markers of exposure. Such markers are needed to aid in the diagnostic process and for discerning novel and specific treatment strategies. Research suggests that earlier identification and diagnosis with an FASD may help in reducing the chance of adverse life outcomes among individuals with prenatal alcohol exposure [72]. Continued research aimed at understanding the relationship between alcohol-induced brain development disruption and the associated functional deficits may also help in developing novel brain-based treatments and interventions for individuals with FASD.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Centers for Disease Control and Prevention (CDC). Alcohol use and binge drinking among women of childbearing age: United States, 2006–2010. MMWR Morb Mortal Wkly Rep. 2012;61(28):534–8.
Jones KL, Smith DW, Ulleland CN, Streissguth AP. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1(7815):1267–71.
Lemoine P, Harousseau H, Borteyru JP, Menuet JC. Les enfants des parents alcoholiques: anomolies observees a propos de 127 cas. Quest Med. 1968;25:476–82.
Mattson SN, Riley EP, Gramling L, Delis DC, Jones KL. Neuropsychological comparison of alcohol-exposed children with or without physical features of fetal alcohol syndrome. Neuropsychology. 1998;12(1):146–53.
Mattson SN, Riley EP, Gramling L, Delis DC, Jones KL. Heavy prenatal alcohol exposure with or without physical features of fetal alcohol syndrome leads to IQ deficits. J Pediatr. 1997;131(5):718–21.
Clarren SK. Neuropathology in fetal alcohol syndrome. In: West JR, editor. Alcohol and brain development. New York: Oxford University Press; 1986. p. 158–66.
Coles CD, Li Z. Functional neuroimaging in the examination of effects of prenatal alcohol exposure. Neuropsychol Rev. 2011;21(2):119–32.
Lebel C, Roussotte F, Sowell ER. Imaging the impact of prenatal alcohol exposure on the structure of the developing human brain. Neuropsychol Rev. 2011;21(2):102–18.
Nuñez SC, Roussotte F, Sowell ER. Focus on: structural and functional brain abnormalities in fetal alcohol spectrum disorders. Alcohol Res Health. 2011;34(1):121–31.
Wozniak JR, Muetzel RL. What does diffusion tensor imaging reveal about the brain and cognition in fetal alcohol spectrum disorders? Neuropsychol Rev. 2011;21(2):133–47.
Chen X, Coles CD, Lynch ME, Hu X. Understanding specific effects of prenatal alcohol exposure on brain structure in young adults. Hum Brain Mapp. 2012;33(7):1663–76.
Rajaprakash M, Chakravarty MM, Lerch JP, Rovet J. Cortical morphology in children with alcohol-related neurodevelopmental disorder. Brain Behav. 2014;4(1):41–50.
Sowell ER, Mattson SN, Kan E, Thompson PM, Riley EP, Toga AW. Abnormal cortical thickness and brain-behavior correlation patterns in individuals with heavy prenatal alcohol exposure. Cereb Cortex. 2008;18(1):136–44.
Fernández-Jaén A, Fernández-Mayoralas DM, Quiñones Tapia D, Calleja-Pérez B, García-Segura JM, Arribas SL, et al. Cortical thickness in fetal alcohol syndrome and attention deficit disorder. Pediatr Neurol. 2011;45(6):387–91.
Yang Y, Roussotte F, Kan E, Sulik KK, Mattson SN, Riley EP, et al. Abnormal cortical thickness alterations in fetal alcohol spectrum disorders and their relationships with facial dysmorphology. Cereb Cortex. 2012;22(5):1170–9.
Zhou D, Lebel C, Lepage C, Rasmussen C, Evans A, Wyper K, et al. Developmental cortical thinning in fetal alcohol spectrum disorders. NeuroImage. 2011;58(1):16–25.
Archibald SL, Fennema-Notestine C, Gamst A, Riley EP, Mattson SN, Jernigan TL. Brain dysmorphology in individuals with severe prenatal alcohol exposure. Dev Med Child Neurol. 2001;43:148–54.
Astley SJ, Aylward EH, Olson HC, Kerns K, Brooks A, Coggins TE, et al. Magnetic resonance imaging outcomes from a comprehensive magnetic resonance study of children with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2009;33(10):1671–89.
Mattson SN, Riley EP, Jernigan TL, Ehlers CL, Delis DC, Jones KL, et al. Fetal alcohol syndrome: a case report of neuropsychological, MRI, and EEG assessment of two children. Alcohol Clin Exp Res. 1992;16(5):1001–3.
Johnson VP, Swayze VWI, Sato Y, Andreasen NC. Fetal alcohol syndrome: craniofacial and central nervous system manifestations. Am J Med Genet. 1996;61(4):329–39.
Swayze VWI, Johnson VP, Hanson JW, Piven J, Sato Y, Giedd JN, et al. Magnetic resonance imaging of brain anomalies in fetal alcohol syndrome. Pediatrics. 1997;99(2):232–40.
Autti-Rämö I, Autti T, Korkman M, Kettunen S, Salonen O, Valanne L. MRI findings in children with school problems who had been exposed prenatally to alcohol. Dev Med Child Neurol. 2002;44(2):98–106.
Sowell ER, Mattson SN, Thompson PM, Jernigan TL, Riley EP, Toga AW. Mapping callosal morphology and cognitive correlates. Neurology. 2001;57:235–44.
Bookstein FL, Sampson PD, Connor PD, Streissguth AP. Midline corpus callosum is a neuroanatomical focus of fetal alcohol damage. Anat Rec. 2002;269(3):162–74.
Bookstein FL, Streissguth AP, Sampson PD, Connor PD, Barr HM. Corpus callosum shape and neuropsychological deficits in adult males with heavy fetal alcohol exposure. NeuroImage. 2002;15(1):233–51.
Joseph J, Warton C, Jacobson SW, Jacobson JL, Molteno CD, Eicher A, et al. Three-dimensional surface deformation-based shape analysis of hippocampus and caudate nucleus in children with fetal alcohol spectrum disorders. Hum Brain Mapp. 2014;35(2):659–72.
Willoughby KA, Sheard ED, Nash K, Rovet J. Effect of prenatal alcohol exposure on hippocampal volume, verbal learning, and verbal and spatial recall in late childhood. J Int Neuropsychol Soc. 2008;14:1022–33.
Fryer SL, Mattson SN, Jernigan TL, Archibald SL, Jones KL, Riley EP. Caudate volume predicts neurocognitive performance in youth with heavy prenatal alcohol exposure. Alcohol Clin Exp Res. 2012;36(11):1932–41.
Sowell ER, Thompson PM, Mattson SN, Tessner KD, Jernigan TL, Riley EP, et al. Regional brain shape abnormalities persist into adolescence after heavy prenatal alcohol exposure. Cereb Cortex. 2002;12:856–65.
De Guio F, Mangin JF, Rivière D, Perrot M, Molteno CD, Jacobson SW, et al. A study of cortical morphology in children with fetal alcohol spectrum disorders. Hum Brain Mapp. 2014;35(5):2285–96.
Reinhardt K, Mohr A, Gärtner J, Spohr HL, Brockmann K. Polymicrogyria in fetal alcohol syndrome. Birth Defects Res A Clin Mol Teratol. 2010;88(2):128–31.
Neil J, Miller J, Mukherjee P, Huppi PS. Diffusion tensor imaging of normal and injured developing human brain - a technical review. NMR Biomed. 2002;15(7–8):543–52.
Lebel C, Rasmussen C, Wyper K, Walker L, Andrew G, Yager J, et al. Brain diffusion abnormalities in children with fetal alcohol spectrum disorder. Alcohol Clin Exp Res. 2008;32(10):1732–40..
Green CR, Lebel C, Rasmussen C, Beaulieu C, Reynolds JN. Diffusion tensor imaging correlates of saccadic reaction time in children with fetal alcohol spectrum disorder. Alcohol Clin Exp Res. 2013;37(9):1499–507.
Raznahan A, Shaw P, Lalonde F, Stockman M, Wallace GL, Greenstein D, et al. How does your cortex grow? J Neurosci Off J Soc Neurosci. 2011;31(19):7174–7.
Simmonds D, Hallquist MN, Asato M, Luna B. Developmental stages and sex differences of white matter and behavioral development through adolescence: a longitudinal diffusion tensor imaging (DTI) study. NeuroImage. 2014;92:356–68.
Lebel C, Mattson SN, Riley EP, Jones KL, Adnams CM, May PA, et al. A longitudinal study of the long-term consequences of drinking during pregnancy: heavy in utero alcohol exposure disrupts the normal processes of brain development. J Neurosci Off J Soc Neurosci. 2012;32(44):15243–51. This is the first longitudinal examination of cortical maturation in FASD using MRI.
Treit S, Lebel C, Baugh L, Rasmussen C, Andrew G, Beaulieu C. Longitudinal MRI reveals altered trajectory of brain development during childhood and adolescence in fetal alcohol spectrum disorders. J Neurosci Off J Soc Neurosci. 2013;33(24):10098–109. This is the first longitudinal examination of white matter microstructure maturation in FASD using DTI.
Sale A, Berardi N, Maffei L. Environment and brain plasticity: towards an endogenous pharmacotherapy. Physiol Rev. 2014;94(1):189–234.
Stephen JM, Kodituwakku PW, Kodituwakku EL, Romero L, Peters AM, Sharadamma NM, et al. Delays in auditory processing identified in preschool children with FASD. Alcohol Clin Exp Res. 2012;36(10):1720–7.
Sedley W, Cunningham MO. Do cortical gamma oscillations promote or suppress perception? An under-asked question with an over-assumed answer. Front Hum Neurosci. 2013;7:595.
Stephen JM, Coffman BA, Stone DB, Kodituwakku P. Differences in MEG gamma oscillatory power during performance of a prosaccade task in adolescents with FASD. Front Hum Neurosci. 2013;7:900.
Fryer SL, Tapert SF, Mattson SN, Paulus MP, Spadoni AD, Riley EP. Prenatal alcohol exposure affects frontal-striatal BOLD response during inhibitory control. Alcohol Clin Exp Res. 2007;31(8):1415–24.
O'Brien JW, Norman AL, Fryer SL, Tapert SF, Paulus MP, Jones KL, et al. Effect of predictive cuing on response inhibition in children with heavy prenatal alcohol exposure. Alcohol Clin Exp Res. 2013;37(4):644–54.
Malisza KL, Allman AA, Shiloff D, Jakobson L, Longstaffe S, Chudley AE. Evaluation of spatial working memory function in children and adults with fetal alcohol spectrum disorders: a functional magnetic resonance imaging study. Pediatr Res. 2005;58(6):1150–7.
Malisza KL, Buss JL, Bolster RB, de Gervai PD, Woods-Frohlich L, Summers R, et al. Comparison of spatial working memory in children with prenatal alcohol exposure and those diagnosed with ADHD; a functional magnetic resonance imaging study. J Neurodev Disord. 2012;4(1):12. This study compares fMRI activation and DTI tractography differences in FASD with non-exposed controls with and without a diagnosis of ADHD.
Astley SJ, Aylward EH, Olson HC, Kerns K, Brooks A, Coggins TE, et al. Functional magnetic resonance imaging outcomes from a comprehensive magnetic resonance study of children with fetal alcohol spectrum disorders. J Neurodev Disord. 2009;1(1):61–80.
O'Hare ED, Lu LH, Houston SM, Bookheimer SY, Mattson SN, O'Connor MJ, et al. Altered frontal-parietal functioning during verbal working memory in children and adolescents with heavy prenatal alcohol exposure. Hum Brain Mapp. 2009;30(10):3200–8.
Norman AL, O'Brien JW, Spadoni AD, Tapert SF, Jones KL, Riley EP, et al. A functional magnetic resonance imaging study of spatial working memory in children with prenatal alcohol exposure: contribution of familial history of alcohol use disorders. Alcohol Clin Exp Res. 2013;37(1):132–40. This study compares fMRI activation differences in FASD with non-exposed controls with and without a family history of alcoholism.
Spadoni AD, Bazinet AD, Fryer SL, Tapert SF, Mattson SN, Riley EP. BOLD response during spatial working memory in youth with heavy prenatal alcohol exposure. Alcohol Clin Exp Res. 2009;33(12):2067–76.
Meintjes EM, Jacobson JL, Molteno CD, Gatenby JC, Warton C, Cannistraci CJ, et al. An FMRI study of number processing in children with fetal alcohol syndrome. Alcohol Clin Exp Res. 2010;34(8):1450–64.
Santhanam P, Li Z, Hu X, Lynch ME, Coles CD. Effects of prenatal alcohol exposure on brain activation during an arithmetic task: an fMRI study. Alcohol Clin Exp Res. 2009;33(11):1901–8.
Colby JB, Smith L, O'Connor MJ, Bookheimer SY, Van Horn JD, Sowell ER. White matter microstructural alterations in children with prenatal methamphetamine/polydrug exposure. Psychiatry Res. 2012;204(2–3):140–8.
Diwadkar VA, Meintjes EM, Goradia D, Dodge NC, Warton C, Molteno CD, et al. Differences in cortico-striatal-cerebellar activation during working memory in syndromal and nonsyndromal children with prenatal alcohol exposure. Hum Brain Mapp. 2013;34(8):1931–45.
Biswal B, Yetkin FZ, Haughton VM, Hyde JS. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med. 1995;34(4):537–41.
Damoiseaux JS, Greicius MD. Greater than the sum of its parts: a review of studies combining structural connectivity and resting-state functional connectivity. Brain Struct Funct. 2009;213(6):525–33.
Damoiseaux JS, Rombouts SA, Barkhof F, Scheltens P, Stam CJ, Smith SM, et al. Consistent resting-state networks across healthy subjects. Proc Natl Acad Sci U S A. 2006;103(37):13848–53.
Greicius MD, Krasnow B, Reiss AL, Menon V. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci U S A. 2003;100(1):253–8.
Santhanam P, Coles CD, Li Z, Li L, Lynch ME, Hu X. Default mode network dysfunction in adults with prenatal alcohol exposure. Psychiatry Res. 2011;194(3):354–62.
Wozniak JR, Mueller BA, Muetzel RL, Bell CJ, Hoecker HL, Nelson ML, et al. Inter-hemispheric functional connectivity disruption in children with prenatal alcohol exposure. Alcohol Clin Exp Res. 2011;35(5):849–61.
Wozniak JR, Mueller BA, Bell CJ, Muetzel RL, Hoecker HL, Boys CJ, et al. Global functional connectivity abnormalities in children with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2013;37(5):748–56.
Stacey D, Clarke TK, Schumann G. The genetics of alcoholism. Curr Psychiatr Rep. 2009;11(5):364–9.
Fryer SL, McGee CL, Matt GE, Riley EP, Mattson SN. Evaluation of psychopathological conditions in children with heavy prenatal alcohol exposure. Pediatrics. 2007;119(3):e733–41.
Hoyme HE, May PA, Kalberg WO, Kodituwakku P, Gossage JP, Trujillo PM, et al. A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: clarification of the 1996 institute of medicine criteria. Pediatrics. 2005;115(1):39–47.
Roussotte FF, Sulik KK, Mattson SN, Riley EP, Jones KL, Adnams CM, et al. Regional brain volume reductions relate to facial dysmorphology and neurocognitive function in fetal alcohol spectrum disorders. Hum Brain Mapp. 2012;33(4):920–37.
Yang Y, Phillips OR, Kan E, Sulik KK, Mattson SN, Riley EP, et al. Callosal thickness reductions relate to facial dysmorphology in fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2012;36(5):798–806.
Wozniak JR, Mueller BA, Chang PN, Muetzel RL, Caros L, Lim KO. Diffusion tensor imaging in children with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2006;30(10):1799–806.
Wozniak JR, Muetzel RL, Mueller BA, McGee CL, Freerks MA, Ward EE, et al. Microstructural corpus callosum anomalies in children with prenatal alcohol exposure: an extension of previous diffusion tensor imaging findings. Alcohol Clin Exp Res. 2009;33(10):1825–35.
Spottiswoode BS, Meintjes EM, Anderson AW, Molteno CD, Stanton ME, Dodge NC, et al. Diffusion tensor imaging of the cerebellum and eyeblink conditioning in fetal alcohol spectrum disorder. Alcohol Clin Exp Res. 2011;35(12):2174–83.
Suttie M, Foroud T, Wetherill L, Jacobson JL, Molteno CD, Meintjes EM, et al. Facial dysmorphism across the fetal alcohol spectrum. Pediatrics. 2013;131(3):e779–88. This study examines facial characteristics of children using 3D facial imaging technology and compares neurobehavioral performance of alcohol-exposed children with and without FAS-like facial features.
Coffman BA, Kodituwakku P, Kodituwakku EL, Romero L, Sharadamma NM, Stone D, et al. Primary visual response (M100) delays in adolescents with FASD as measured with MEG. Hum Brain Mapp. 2013;34(11):2852–62.
Streissguth AP, Bookstein FL, Barr HM, Sampson PD, O'Malley K, Young JK. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25(4):228–38.
Coles CD, Goldstein FC, Lynch ME, Chen X, Kable JA, Johnson KC, et al. Memory and brain volume in adults prenatally exposed to alcohol. Brain Cogn. 2011;75(1):67–77.
de Zeeuw P, Zwart F, Schrama R, van Engeland H, Durston S. Prenatal exposure to cigarette smoke or alcohol and cerebellum volume in attention-deficit/hyperactivity disorder and typical development. Transl Psychiatr. 2012;2:e84.
Nardelli A, Lebel C, Rasmussen C, Andrew G, Beaulieu C. Extensive deep gray matter volume reductions in children and adolescents with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2011;35(8):1404–17.
Cardenas VA, Price M, Infante MA, Moore EM, Mattson SN, Riley EP, et al. Automated cerebellar segmentation: Validation and application to detect smaller volumes in children prenatally exposed to alcohol. NeuroImage Clin. 2014;4:295–301.
Colby JB, Soderberg L, Lebel C, Dinov ID, Thompson PM, Sowell ER. Along-tract statistics allow for enhanced tractography analysis. NeuroImage. 2012;59(4):3227–42.
Burden MJ, Westerlund A, Muckle G, Dodge N, Dewailly E, Nelson CA, et al. The effects of maternal binge drinking during pregnancy on neural correlates of response inhibition and memory in childhood. Alcohol Clin Exp Res. 2011;35(1):69–82.
Roussotte FF, Bramen JE, Nuñez SC, Quandt LC, Smith L, O'Connor MJ, et al. Abnormal brain activation during working memory in children with prenatal exposure to drugs of abuse: the effects of methamphetamine, alcohol, and polydrug exposure. NeuroImage. 2011;54(4):3067–75.
Codreanu I, Yang J, Zhuang H. Brain single-photon emission computed tomography in fetal alcohol syndrome: a case report and study implications. J Child Neurol. 2012;27(12):1580–4.
Roussotte FF, Rudie JD, Smith L, O'Connor MJ, Bookheimer SY,Narr KL, et al. Frontostriatal connectivity in children during working memory and the effects of prenatal methamphetamine, alcohol, and polydrug exposure. Dev Neurosci. 2012;34(1):43–57.
Acknowledgments
The authors thank the National Institute on Alcohol Abuse and Alcoholism (NIAAA) for their continued financial support: U24 AA014811, F31 AA022033, and T32 AA013525. We also thank the participants of current, past and future neuroimaging studies who generously supply their time, allowing valuable insight to be gained into the neuropathology of Fetal Alcohol Spectrum Disorder.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 3
(DOCX 121 kb)
Supplementary Table 4
(DOCX 114 kb)
Supplementary Table 5
(DOCX 123 kb)
Supplementary Table 6
(DOCX 130 kb)
Rights and permissions
About this article
Cite this article
Moore, E.M., Migliorini, R., Infante, M.A. et al. Fetal Alcohol Spectrum Disorders: Recent Neuroimaging Findings. Curr Dev Disord Rep 1, 161–172 (2014). https://doi.org/10.1007/s40474-014-0020-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40474-014-0020-8